Introduction
Diabetes mellitus is a systemic condition that has been associated with an increased likelihood of developing infections in patients. This is due to its immunosuppressive role, which is exacerbated in patients who do not have adequate control of the disease (1). In dentistry, diabetes has been linked to an increase in morbidity and mortality from odontogenic infections (2). This is because diabetes mellitus affects the healing process, and in turn, hyperglycemia affects coagulation, endothelial function, and fibrinolysis (3, 4). Moreover, hyperglycemia alters chemotaxis, adherence, phagocytosis, and other immune system alterations, decreasing the function of neutrophils and monocytes (5,6,7). The possibility of infection progression increases in situations of immunosuppression, where oral abscesses can become deep neck infections. This not only increases the complexity and difficulty of treatment, but also leads to the patient having a higher risk of complications and death (8, 9). This situation has led dentists to postpone dental treatments until the patient reaches "normal" glucose values. Carey et al. (10) in a retrospective cohort study found that patients with type 2 diabetes mellitus had a higher mortality rate related to infection (1.92 (95% CI: 1.75 to 2.10)). Additionally, they reported that 12.4% of deaths caused by infection could be attributed to diabetes. On the other hand, they mention that diabetic patients should receive immediate, adequate, and timely management for any type of infection that has the potential to become complicated.
Chronic suppurative osteomyelitis of the mandible is a complex multifactorial disease (11) whose management represents a challenge for oral and maxillofacial surgeons due to its anatomical location and polymicrobial nature. In addition, its management requires expensive treatments and prolonged hospital stays (12, 13). Baur et al. (14) mentioned that diseases that produce immuno- suppression (such as diabetes, malnutrition, and neoplasms) and other diseases that produce bone hypovascularization could predispose to a higher risk of mandibular osteomyelitis. Furthermore, Sood et al. (15) found that immunosuppressed patients, such as those with diabetes, face harder challenges in the treatment of osteomyelitis because they may require more radical treatments to reduce the risk of osteomyelitis recurrence. The objective of this study is to describe a case that highlights the importance of early and aggressive treatment of a patient with chronic suppurative osteomyelitis of the mandible and diabetes as a comorbidity.
Case report
A 52-year-old male patient presented to the Oral and Maxillofacial Surgery Department of the Hipólito Unanue National Hospital. The patient was referred by the Traumatology department after having suffered a fall three months ago, hitting his hip and chin. The patient reported dental mobility, pain in the lower left region, and loss of sensitivity in the lower lip and chin. His medical history indicated grade III osteoarthritis which was diagnosed five years ago and he was taking oral analgesics/ anti-inflammatories for pain (diclofenac 50 mg, in cases of severe pain associated with dexamethasone 4 mg). In addition, the patient was diagnosed with type 2 diabetes mellitus by the endocrinology service a month ago and he was medicated with metformin 850 mg orally every 8 hours. The patient did not attend his trauma check-ups and reported that he self-medicated with dexamethasone 4 mg orally every 8 hours for three months due to the intense pain he presented after the fall. In the extraoral evaluation, the patient presented swelling in the left genial and masseteric region with hypoesthesia of the chin and lower left lip. In the intraoral evaluation, the patient presented severe periodontitis, trismus, bone exposure of the alveolar ridge of the third quadrant, purulent discharge, and absence of teeth 36, 37, 38. In the imaging evaluation, the tomography showed a fracture in the left mandibular ramus with loss of continuity of the vestibular and lingual cortex in the symphysis, body, ramus, and condyle (Figure 1).

Figure 1 Computed tomography scan of facial mass (3D reconstruction) - Left lateral preoperative view.
The diagnosis was chronic suppurative osteomyelitis of the mandible confirmed by histopathological analysis. The planning of the patient's treatment was carried out in a multidisciplinary way with the participation of three surgical teams: oral and maxillofacial surgery, thoracic and cardiovascular surgery (to obtain the costochondral graft), and traumatology (to obtain the fascia lata of the thigh). The surgical procedure consisted of a hemimandibulectomy performed through a "lip split" extraoral approach, after which the lesion was dissected in layers until the entire lesion was exposed (Figure 2).
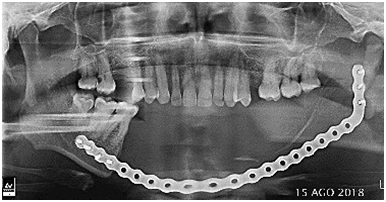
Subsequently, the musculature was disinserted and the left hemimandible was resected considering the margin anterior or proximal to piece 44. Once the defect was exposed, the operating field was cleaned with a saline solution and hemostasis was promoted. The mandibular reconstruction was performed using a costochondral graft plus fascia lata to replace the condyle and joint. Maxillomandibular fixation was then performed and the osteosynthesis material was fixed with the reconstruction plate (Figure 3). After that, the flap was repositioned and closed from the facial planes. Pharmacological treatment consisted of intravenous administration of vancomycin 500 mg every 12 h and meropenem 1 g every 8 h for 12 days. After discharge, the patient continued oral treatment with clindamycin 300 mg every 6 h for 14 days and then with ciprofloxacin 500 mg every 12 h for 14 days. Periodic controls were performed every six months with a favourable clinical evolution of the patient. Figure 4 shows the followup at 3 years and 7 months after surgery.
Discussion
Patients with diabetes mellitus or diseases that compromise the immune system may present mild odontogenic infections that can rapidly progress to deeper spaces in the head and/or neck (16,17,18). This not only makes treatment difficult but also exposes patients to a higher risk of complications and death (2, 18,19,20). The present case reports the early and aggressive treatment of a patient with type 2 diabetes mellitus and arthritis, who self-medicated with dexamethasone for three months (prolonged administration of which produces immunosuppression) and presented a rapid progression to chronic suppurative osteomyelitis of the mandible.
Kasperk et al. (21) reported that diabetes mellitus affects bone metabolism and may increase the risk of fractures. This is due to the suppression of bone formation and stimulation of bone resorption. In addition, if we also consider local factors such as severe periodontitis, it could lead to a higher risk of odontogenic infections. Baur et al. (14) stated that patients with chronic osteomyelitis of the mandible and comorbidities such as diabetes mellitus exhibit arterial stiffness and microvascular rarefaction due to hypertrophic remodeling of blood vessels. This suggests an association between chronic osteomyelitis of the mandible and microvascular involvement in patients with diabetes. Ko et al. (2) found that patients with diabetes mellitus had a higher risk of developing odontogenic infections involving multiple facial spaces (facial cellulitis and deep cervical infections).
In relation to long-term corticosteroid treatment, Giles et al. (22) mentioned that corticosteroids cause immunosuppression by decreasing the proliferation and differentiation of a subset of T cells. However, the exact molecular mechanisms by which this effect occurs are still unknown. In addition, Barshes et al. (23) mentioned that corticosteroids have two main immunosuppressive effects, the first being the sequestration of T-CD4+ lymphocytes in the reticuloendothelial system (RES) and the second being the inhibition of lymphokines and cytokines, especially IL-1 and IL-6. Additionally, there is a relationship between the use of corticosteroids and hyperglycemia, as corticosteroids can increase blood glucose levels which can worsen the severity of diabetes (24).
On the other hand, chronic suppurative osteomyelitis of the mandible in adults is potentially refractory if surgical debridement is inadequate, regardless of antibiotic therapy (2). In the present case, we performed aggressive treatment due to the extensive bone destruction and the patient's systemic condition that led to the rapid progression of the disease.
Baur et al. (14) reported that 50% of patients with chronic suppurative osteomyelitis of the maxilla who underwent marginal resection had a recurrence, compared to a recurrence rate of 5.5% in patients who underwent segmental resection. They mention that conservative management in patients with chronic osteomyelitis of the mandible results in a longer treatment period, more surgeries, and thus increased resource utilization and costs. So, an initially more aggressive surgical treatment could lead to a higher likelihood of success for the patient’s clinical outcome.
Conclusions
In conclusion, the microvascular involvement and immunosuppression caused by diabetes and corticosteroid use, along with local factors (such as periodontal disease and trauma), contribute to the progression of chronic osteomyelitis of the mandible by exacerbating the clinical picture. In patients with these systemic conditions, timely surgical excision of the affected tissue with appropriate pharmacological treatment is crucial for successful management due to the risk of recurrence and postoperative complications.
Author contribution statement
Conceptualization and design: D.C.V.R. and A.R.F.
Literature review: L.C.R.
Investigation and data collection: D.C.V.R., A.R.F. and D.M.V.
Data analysis and interpretation: D.C.V.R., A.R.F. and D.M.V.
Writing-original draft preparation: D.C.V.R., V.C.C. and L.C.R.
Writing-review & editing: D.C.V.R., D.M.V.,V.C.C. and L.C.R.
Supervision: D.M.V.