Introduction
The retromolar canal is a neurovascular anatomic variation consisting of a bifurcation of the mandibular canal towards the retromolar area, after the third molar, usually associated with a foramen situated on the retromolar fossa (1,5).
The retromolar canal has been described as a rare anatomic structure or an uncommon anatomic variation. However, it has been shown more recently that the presence of retromolar canal may be frequent, with a variable prevalence according to the study methods (e.g. in dry skulls and imaging exams) (3,5,6) and the population studied (3,6).
In clinical practice, this anatomical variation can be identified only by radiographic methods. However, conventional radiographs, such as panoramic images, have been shown to be insufficient due to overlapping structures that make the retromolarcanal not accurately identified. In this sense, conebeam computed tomography (CBCT), for providing high resolution images for hard tissues, without overlapping and with the possibility of reconstructions in several planes, has been indicated for the diagnosis of retromolar canals (4,7,8).
The clinical relevance of this anatomic variation remains unclear, particularly regarding eventual interference with anesthetic procedures involving the inferior alveolar nerve block (4,6,7,9,10).
The aim of this study was to show whether the presence of a retromolar canal influenced the anesthetic efficacy of the inferior alveolar nerve block in patients with unilateral retromolar canal. The null hypothesis was that there is no difference between the anesthetic efficacy of the inferior alveolar nerve block in regions with and without retromolar canal.
Materials and methods
This study was approved by the Research Ethics Committee of the School of Dentistry of Ribeirão Preto, University of São Paulo (FORP-USP), under registration number 69603817.0.0000.5419. This study was also approved by the Brazilian clinical trials registry (REBEC) under registration number RBR-4SNTGT in 01/06/2018. All methods were performed according to the relevant guidelines and regulations of the Declaration of Helsinki. Written informed consent was obtained from all participants and/or their legal guardians for study participation.
This study was an observational clinical study, as the objective was to observe the behavior of the patient after the anesthetic procedure. Therefore, the focus was on the results of pulp vitality and gingival tissue pressure tests (both reversible to the point that they cannot be consi- dered interventions). In addition, this study was characterized by double-blind randomization, as the tests were performed without the dentists and study participants being aware of which side the retromolar canal was present.
Participants
Nine patients that presented unilateral retromolar canal identified on CBCT exams and with clinical indication of dental procedures requiring anesthetic block of the inferior alveolar nerve were invited to take part in the anesthetic efficacy test. The exclusion criteria were allergy to mepivacaine, presence of mucosal lesions in the retromolar area, and use of systemic medications that may interfere with oral sensitivity.
A trained and experienced evaluator assessed all CBCT exams using OnDemand3D software (Cybermed, Seoul, South Korea). The analyzes were performed in a quiet and dimly lit room. The observer was free to use reconstructed images in all planes to assess the presence and characteristics of the retromolar canal, as well as to use software tools to adjust the images (eg, zoom, brightness/contrast). The morphology and course of the canal were evaluated, and the canals were classified into type A1 (vertical), A2 (vertical with presence of horizontal branch), B1 (curved), B2 (curved with presence of additional horizontal channel) and C horizontal) (6).
Interventions
Anesthetic efficacy tests were carried out on both left and right sides of patients who agreed to participate and signed the informed consent term. The initial side for each patient was randomly assigned using a coin flip. The same procedures (inferior alveolar nerve block, and pre-and post-anesthesia tests) were performed on the other side after one week. A single experienced dentist, blinded to the side of the mandible that had a retromolar canal, performed all the tests and anesthetic procedures.
Assessment of patient response to thermal (pulp vitality test) and pressure (compression of soft tissue) stimuli were done before and 5 minutes after the inferior alveolar nerve block technique, using both visual analogue (VAS) scale and Mc Gill (McG) pain questionnaire.
For the thermal stimulus, Endo-Frost® (Roeko-Germany) was applied for 5 seconds according to the manufacturer's recommendation in the cervical buccal region of the 1st and 2nd molars (near the marginal gingiva).
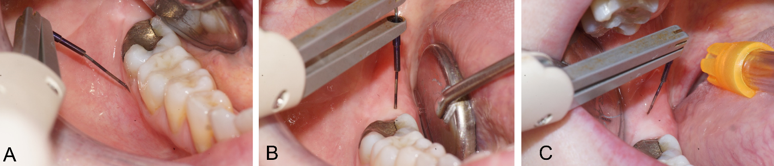
For standardized mechanical pressure stimuli, the Florida Probe® (Florida Probe Co. Gainesville, FL, USA) was used (11). The probe was electro- nically calibrated to have a contact pressure of 25 g (0.25 N) of the active tip with the tissue. The pressure was applied perpendicularly, for 5 seconds, in the following regions: 3mm below the cervical buccal gingival of the 1st and 2nd molar, 3mm below the cervical lingual gingiva of the 1st and 2nd molar and two occlusal regions after the 2nd molar in the anteroposterior direction, the first one being 2mm after the distal of the 2nd molar and the other 2mm after this point (Figure 1).
Anesthetic block of the inferior alveolar nerve was performed using a carpule-type syringe supplied with 1.8mL of mepivacaine 2% 1:100.000 with epinefrine and a long needle for adult use. Inferior alveolar nerve block was performed by introducing the needle into the mucosa in the medial aspect of the mandibular ramus, at the intersection of two lines: one horizontal, representing the height of the injection, and the other vertical, representing the anteroposterior plane of the injection, three-quarters of the anterior-posterior distance of the coronoid notch to the deepest part of the pterygomandibular raphe. Once in the correct position, the operator injected the entire content of the anesthetic cartridge over 60 seconds. With this technique, the regions expected to be under anesthetic effect are the lower teeth (unilateral posteriors and interiors), mandible body and inferior ramus, buccal mucoperiosteum and mucous membrane distal to the mental foramen (mental nerve). Due to concomitant block of the lingual nerve with this technique, the anterior two thirds of the tongue, the floor of the oral cavity, periosteum and lingual soft tissues are also expec- ted to be anesthetized (12).
Data analysis
The study outcome was the patient response (assessed with VAS and McG) to thermal and pressure stimuli before and after inferior alveolar nerve block. The analyzed variable was the percen- tage decrease of patient response to thermal and pressure stimuli. The efficacy of anesthesia was considered in terms of decrease of patient response. Therefore, higher values are interpreted as higher efficacy of the inferior alveolar nerve block. The data were compared for the sides with and without retromolar canal (split-mouth) with Wilcoxon (5% significance level).
Results
In the present study, there were patients with canals type A1 (vertical), B1 (curved) and C horizontal) (11) (Figure 2).
Before anesthesia, hemi mandibles with and without retromolar canal did not differ in terms of response to thermal and pressure stimuli (p>0.05) (Figure 2). After anesthesia, hemi mandibles with and without retromolar canal showed statistically reductions in patient response visual analog scale (VAS) and Mc Gill (McG) pain questionnaires for both thermal and pressure stimuli (p<0.05), indicating that the inferior alveolar nerve blockage had success on a significant level (Figure 2).
Comparing sides with and without retromolar canal after inferior alveolar nerve blockage, the reduction in patient response to pressure stimulus was higher for the hemi mandibles without in five and six cases (according to VAS or McG, respectively) (Figure 2). Similarly, hemi mandibles without retromolar canal had a higher reduction in patient response for thermal stimulus in up to five out of nine cases (McG) (Figure 2). Statistically, the differences were not observed.

Figure 2 Schematic figure of RMC classification and their CBCT sagittal reconstruction for each patient. Values of patient response decrease on the inferior alveolar nerve block for hemi mandibles with and without retromolar canal, according to Visual analog scale (VAS) and Mc Gill scales (McG). With RMC: presence of retromolar canal; Without RMC: absence of retromolar canal. NI: retromolar canal without classification. Asterisk and bold numbers indicate a reduction of patient response on the side without retromolar canal.
Discussion
Previous anatomic studies have suggested a link between failures of anesthetic procedures and the presence of neurovascular anatomic variations, such as retromolar canal (2,3,9). However, no clinical studies have been carried out to support it.
On the nine patients assessed, after the inferior alveolar nerve block procedure, the overall decrease in patient response for both pressure and thermal stimuli was similar among the hemi mandibles with and without retromolar canal. These findings show that the presence of retromolar canal does not necessarily determine anesthetic failure of the inferior alveolar nerve block. However, in most cases (5 or 6 out of 9), the decrease in patient response was higher for the hemimandible without retromolar canal. Consequently, the speculation that the presence of retromolar canal may interfere with anesthetic efficacy may be true for some patients. Such cases may be explained by the previously demonstrated anatomic complexity and particularly the variability of nerve configuration associated with the retromolar canal (6,9).
In this sense, imaging exams, such as CBCT, are essential to assess the presence of different types of canals, to predict the anesthetic response prior to the surgical intervention.
Future randomized clinical studies involving functional neuroimaging data are necessary to investigate the retromolar canal influence in the inferior alveolar nerve block.
Thus, it was possible to conclude that the presence of the retromolar canal is not a determinant factor of failure of the inferior alveolar nerve block. However, the patient's response to pressure and thermal stimuli may be influenced by the presence of retromolar canal, mainly in type A and B anatomical variations.
Author contribution statement
Conceptualization and design: J.H.P.F., C.O.S., C.T.
Literature review: E.D.C, J.H.P.F.
Methodology and validation: J.H.P.F., C.O.S., C.T.
Formal analysis: L.M.M., B.N.F., V.P., H.G.A.
Investigation and data collection: J.H.P.F., L.M.M., B.N.F, V.P.
Resources: C.O.S., C.T.
Data analysis and interpretation: E.D.C, J.H.P.F., P.B.C., H.G.A., C.T.
Writing-original draft preparation: E.D.C, J.H.P.F., P.B.C., H.G.A.
Writing-review & editing: E.D.C, J.H.P.F., P.B.C., L.M.M., B.N.F., V.P., H.G.A., C.O.S., C.T.
Supervision: C.O.S., C.T.
Project administration: J.H.P.F., C.O.S., C.T.