Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Acta Médica Costarricense
On-line version ISSN 0001-6002Print version ISSN 0001-6012
Acta méd. costarric vol.60 n.2 San José Apr./Jun. 2018
Articles
Prevalence of parasitosis in children aged 1 to 7 years in vulnerable condition in the South Central Region of Costa Rica
1Sección de Infección y Nutrición. Instituto de Investigaciones en Salud (INISA), Costa Rica
2Departamento de Parasitología. Facultad de Microbiología, Costa Rica
3Programa de Investigación sobre Envejecimiento. Instituto de Investigaciones en Salud (INISA), Universidad de Costa Rica, Costa Rica
4Instituto Regional de Estudios en Sustancias Tóxicas (IRET), Universidad Nacional, Costa Rica
Intestinal parasitosis is a major public health problem.1,2 Currently between 20-30% of the Latin American population suffers from parasitosis.3 However, given that the parasitosis can go unnoticed, it is possible that these prevalences are underestimates and that this disease is neglected because it is not considered a health problem.3 For example, for 2007, it was estimated that approximately 3500 million people were affected by parasitic infections worldwide, but only clinical conditions were reported in 450 million people.4,5 In Costa Rica, as in other poor countries,6 it has been identified that the groups most affected by intestinal parasitosis are children of preschool and school age, which is mainly due to their inadequate hygienic habits and the immaturity of their immune system.4,7,8,9 The last National Nutrition Survey (NNS) conducted in Costa Rica in the years 2008-2009 (n = 227) identified that 8% of children aged 0-6 had pathogenic protozoa, 3% had helminths and 24% had showed commensal protozoa.1,10 However, the findings of the Survey do not reflect the conditions of populations that could be more vulnerable to infection, such as children belonging to the Education and Nutrition Centers and Children’s Nutrition and Comprehensive Care Centers (ENC-CNCCC) of the Ministry of health. The children who benefit from ENC-CNCCC programs come from families that live in poverty, suffer from severe or moderate malnutrition, have signs of some type of aggression, and are children of teenage mothers or poor pregnant or lactating women.11,12,13 This child population is of great relevance, since parasitic diseases are especially prevalent in socially disadvantaged children,14 and generate important sequelae in physical and cognitive development, even when children do not have symptoms of this disease.15
The ENC or CNCC establishments have different programs aimed at children. Undernourished, thin or infants with delayed growth are beneficiaries of the Family Food Distribution Program (FFD), an extramural program (i.e., the child does not stay in the ENC or CNCC establishments, only attends on specific dates for be heavy and measured, while their parents attend once a month to withdraw food for the family group).12,13 Another of the programs offered by the ENC-CNCC establishments is the Child Care and Protection (CCP), of intramural modality, which offers education and daily feeding to children during the hours they remain in the Centers (ENC or CNCC).12,13 Despite the entry criteria of children to be beneficiaries of CCP and FFD, the socioeconomic characteristics of these children can be diverse, depending on the specific center to which they belong and the conditions of each family;16 it has been described that approximately 32% of children benefiting from ENC-CNCC have a high socioeconomic status.17 The few studies conducted in children attending the ENC-CNCC in Costa Rica, have indicated the high prevalence of parasitosis in this population.18,19,20 However, up-to-date information is not available, nor is it known how the different socioeconomic factors influence these parasitosis.18,19,20 That is why the objectives of the study were to determine the prevalence of intestinal parasitosis in children benefiting from the Child Care and Protection (CCP) and Family Food Distribution (FFD) programs of the ENC-CNCC of the South Central Region, and identify the socioeconomic determinants of these parasitosis. It also sought to educate parents and those in charge of the centers in terms of prevention and monitoring of these diseases, and emphasize their appropriate approach to doctors who treat these diseases.
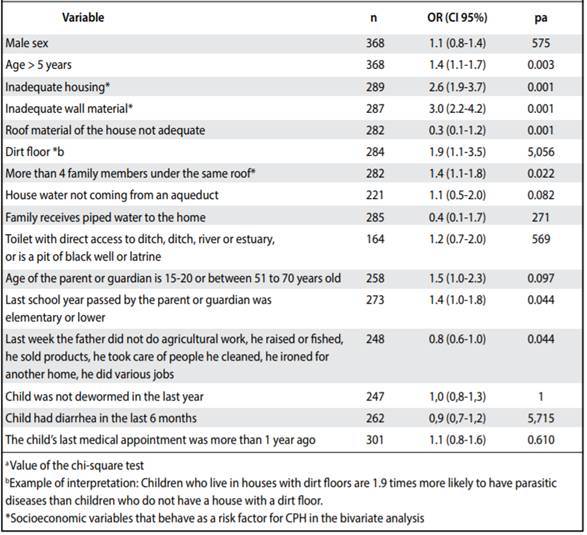
Table 1A. Socio-economic characteristics, deworming and medical attention of parents and children participating in the study who completed the survey and collected fecal samples, beneficiaries of CCP, FFD or both programs of the Central South Region of Costa Rica, 2014-2016.
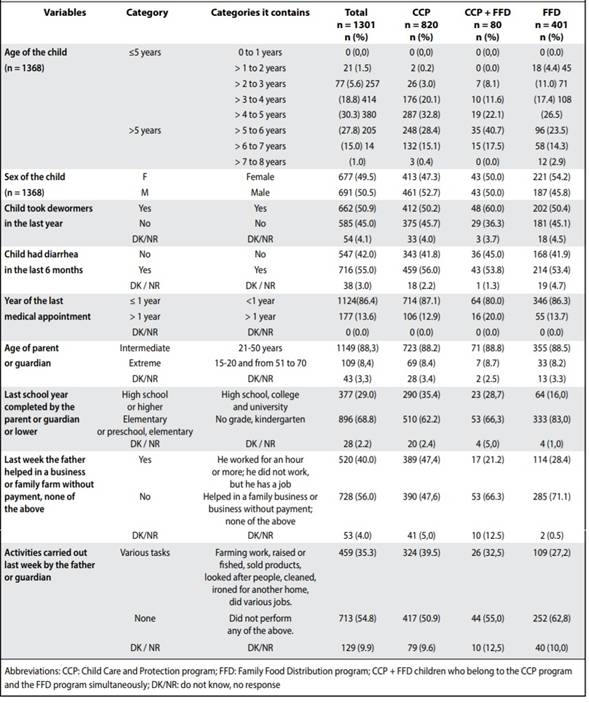
Table 1B. Socioeconomic characteristics of the housing of the families of the children participating in the study who completedthe survey and collected fecal samples, beneficiaries of CCP, FFD or both programs of the Central South Region of Costa Rica, 2014-2016.
Materials and Methods
a. Population and study design An observational cross-sectional study was carried out that included children beneficiaries of the CCP and FFD programs of the ENC-CNCC of the South Central Region of Costa Rica, between August 2014 and May 2016. Only centers were included in the study (ENC or CNCC) that counted simultaneously with the CCP programs (intramural modality) and FFD (extramural modality), so that in each ENC or CNCC information of children of both programs was collected. The Central South Region had 36 ENC-CNCC centers with approximately 3580 children from the CCP and FFD programs (Figure 1). Using as a sampling frame the database generated by the National Directorate of ENC-CNCC of the Ministry of Health in June 2014, 13 of the centers were randomly selected to be counted, a total of 1139 children signed informed consent, of which 733 they corresponded to CCP beneficiaries, 338 to FFD beneficiaries and 68 belonged to both programs (Figure 1). The type of sampling and the size of the sample were chosen based on the size of the population, the available budget and the guideline of the National Directorate of ENC-CNCC to sample all the children in each center, for ethical reasons. All the activities and instruments of the study were approved by the Ethics-Scientific Committee of the University of Costa Rica (VI-2884-2014) and all the parents or caregivers of the participating children signed an informed consent.

Figure 1 Distribution of study participants, according to stool sample delivered and interview (ENHS) performed
b. Interview A part of the National Household Survey of Costa Rica (ENAHO) of 2014 was applied to the parents or caregivers of the children,21 hereinafter referred to as the Extract from the National Household Survey (ENHS). With this survey, sociodemographic information was collected (i.e., child’s age, gender), information on the conditions of the family’s home (i.e., type of dwelling, material of the walls of the house, material of the roof of the house, members of the family under the same roof), of the sanitary conditions (i.e., source of water in the house, connection of the sanitary service), education and work of the parent or guardian (i.e., age of the parent or guardian, last year of study approved by the parent or guardian, type of work performed by the parent or guardian the previous week) and the child’s health (i.e., if the child took dewormers in the last year, if the child had diarrhea in the last 6 months and year of the child’s last medical appointment). The variables were operationalized as dichotomous variables, whose classification is observed in Table 1. c. Collection of stool samples Stool was collected from 637 children (expanded n = 1368); 593 children (n expanded = 1279) gave a single stool sample and 44 children (n expanded = 89) delivered 2 samples (collected on different days). For that it was explained to the parents or guardians of children orally and in writing how to collect stool samples from children and were given a sterile plastic wide-mouth jar. The samples were transported at room temperature to the Laboratory of Medical Helminthology of the Faculty of Microbiology of the University of Costa Rica, where they were analyzed, in a period< 4hours
d. Determination of parasitosis The stool samples were analyzed by means of the direct examination and assembly of Kato.22 The presence of parasites in the feces was classified as: (a) “prevalence of commensal protozoa”, which corresponds to the percentage of children whose sample had 1 or more commensal protozoa (b) “prevalence of helminthiasis”, is the percentage of children whose sample showed 1 or more helminths (c) “prevalence of parasitosis” percentage of children whose sample had 1 or more pathogenic protozoa and / or helminths in the stool sample (d) “prevalence of commensals, pathogens and / or helminths (CHP) “Percentage of children whose sample had any of the following: commensal protozoa, pathogenic protozoa and helminths in the stool, either independently or in combination. The CPH category was created to compare the results of this study with the results of the last National Nutrition Survey of Costa Rica 2008-2009. It is important to clarify that the categories are not mutually exclusive, as a child who presents parasites in their feces (helminths and pathogenic protozoa), can simultaneously present protozoa commensal.
e. Statistical analysis Given that each establishment differed in the number of beneficiaries of the CCP and FFD programs and in the percentage of children with stool samples analyzed, an expansion factor was used prior to the analysis of the data.23 Then, the prevalence of parasitosis and CPH was estimated, for the total population studied, for each of the ENC or CNCC centers and for each aid program. The prevalence of helminthiasis in the total population studied was determined. The differences in the prevalences of parasitosis and CPH were estimated according to sex and program of adscription. In the bivariate analyzes, chi-squared tests were run and odds ratios (OR) were calculated, with their respective 95% confidence intervals (95% CI) to examine the associations between CPH and the different socioeconomic factors (Table 3). Finally, a predictive logistic regression model for CPH was run (Table 4).
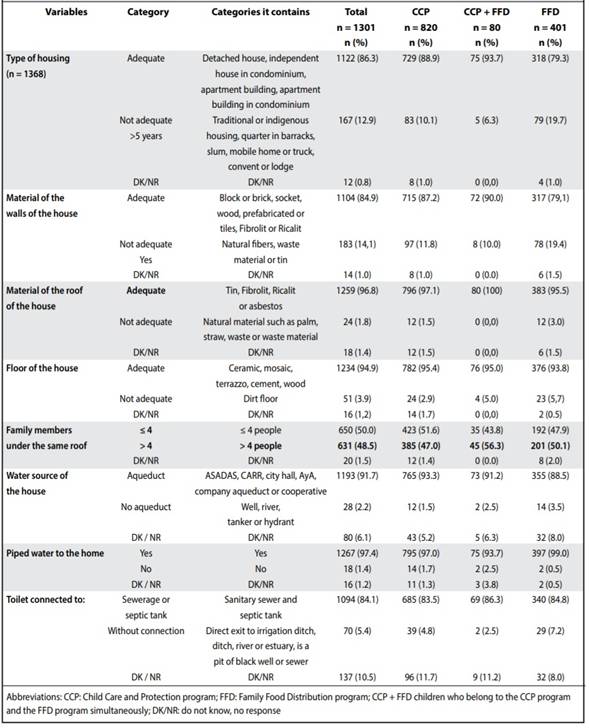
Table 2 Percentage of CPH and parasitosis in the beneficiary children CCP-FFD of the South Central Region, according to center of affiliation, 2014-2016 (n = 1368)
f. Educational sessions Educational sessions were held with 83 teachers and members of the administrative staff of ENC-CNCC, 1200 parents, 23 medical heads and epidemiologists from the Health Areas of the South Central Region of the Costa Rican Social Security Fund (CCSS). Teachers and parents were explained what intestinal parasites are, their clinical manifestations and methods of prevention. The importance of performing a serial stool test (≥ 3 stool samples collected on non-consecutive days) was emphasized when the child had symptoms, but no parasites were observed in the first stool test. Parents were instructed on the proper collection of stool samples; the medical heads and epidemiologists were stressed the importance of the timely attention of the referred children, the need to use appropriate protocols for the approach of the parasitosis and they were updated on the topic of antiparasitic resistance.
Results
a. Characteristics of the study population Table 1 summarizes some of the socioeconomic characteristics of the children who participated in the study and their families. The families of the children studied, despite the low economic level (according to their selection criteria to be beneficiaries of CCP or FFD), mostly had access to basic sanitary conditions (piped water to the home, not having an earth floor) and use of antiparasitics (Table 1). When comparing the characteristics of the families, according to the program to which the child belonged, it was observed that the families of the CCP children had better socioeconomic conditions (eg, better type of housing, better materials of the walls of the house, type of floor, water quality, parents with a higher educational level and more employment) than FFD beneficiaries (Table 1; p <0.05 in all cases).
b. Prevalence of parasitosis b.1. Prevalence of commensals, pathogens and helminths (CPH) Stool samples were analyzed in 1368 children. The prevalence of CPH was 24.1% (95% CI: 21.9-26.4). There were no statistically significant differences in the prevalence of CPH among boys and girls (24.8% vs. 22.8%, respectively, p = 0.40) or between the different aid programs (23.0% of CPH in children beneficiaries of CCPvs. 27.4% in FFD vs. 20.1% in CCP + FFD, p = 0.14). In contrast, differences were found in the prevalence of CPH among the different establishments of the ENC-CNCC (p<0.001, Table 2), with the CNCC La Uruca having the highest prevalence.
When comparing the socioeconomic characteristics of the families of the children of CNCC La Uruca with those of the rest of the centers, it was observed that a greater proportion of families of that center were grouped into categories that suggested a possible risk for CPH in most of the centers variables (according to classification in Table 1, data not shown). It is important to note that in the 89 children who delivered 2 stool samples, there was an increase in the prevalence of CPH of 9.0% (95% CI: 3.0-15.1) with the first stool sample. 21.0% (95% CI: 13.0-30.2) when analyzing 2 stool samples.
b.2. Prevalence of pathogenic parasites In the study population, a prevalence of parasitosis of 8.5% (95% CI: 7.5-10.5) was identified. As for CPH, there were no statistically significant differences in prevalences, according to sex (7.8% in children vs. 10.2% in girls, p = 0.13) or aid program (8.3% in girls) children beneficiaries of CCP vs. 10.3% in FFD vs. 10.5% in CCP + FFD, p = 0.47, but between different establishments (p = 0.006, Table 2). The CNCC The Uruca was the center that presented a higher prevalence of parasitosis.
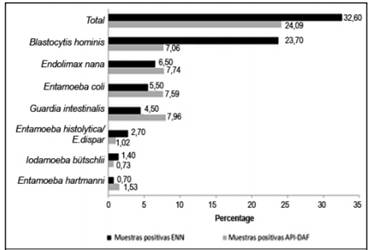
Figure 2 Distribution of intestinal protozoa detected in children aged 1 to 7 years benefiting from the programs of Child Care and Protection (CCP) and Foods to Families Distribution (FFD) 2014-2016 (n = 1368), and in the children 0-6 years old included in the National Nutrition Survey (NNS) conducted in 2008-2009 (n = 227)
b.3. Prevalence of helminths Helminths were found in 10 stool samples (prevalence = 0.7%, 95% CI: 0.1-1.5). Six of these samples presented Ascaris lumbricoides, two showed Trichocephalus trichiurus and two Hymenolepis nana. Two cases of ascariasis were found in the children of ENC de Salitrillos, two cases of hymenolepiasis in children of ENC of Pavas Centro and the rest of helminths were found in children samples of CNCC of La Uruca. The positive ratio of protozoa (pathogens and commensals) with respect to the helminths was 30,8. Figure 2 shows the prevalence of the different protozoa detected in the stool samples of children aged 1 to 7 years who participated in the current study compared to the prevalence found in children aged 0-6 years included in the last National Survey of Nutrition (ENN) performed in 2008- 200910. A greater total prevalence of intestinal protozoa was observed in the ENN; however, ENC-CNCC children had higher prevalences for most protozoa. In the current study, 103 (7.5%) samples were found with 2-4 commensal protozoa, 54 (3.8%) samples with protozoan commensals and protozoan pathogens and 6 (0.4%) samples with mixed infections by protozoa and helminths. Giardia intestinalis was the protozoan of highest prevalence in infants of 2 years, Entamoeba coli was the most frequent in children of 3, 6 and 7 years and Blastocystis hominis was the most frequent in children of 4 and 5 years (data not shown).
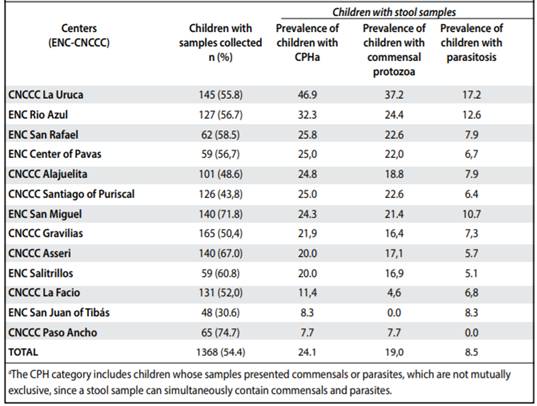
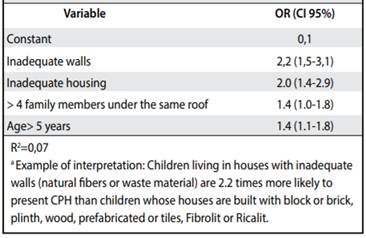
c. Socioeconomic determinants of parasitosis Table 3 shows the results of bivariate analyzes of socioeconomic characteristics with the presence of CPH. It was observed that living in a house with a wall of waste material or tin (OR = 3.0, 95% CI: 2.2-4.2), living in an inadequate dwelling , living in a house with a dirt floor (OR = 1.9, 95% CI): 1.1-3.5), have a family with more than 4 members (OR = 1.4, 95% CI: 1.1-1.8) and an age> 5 years (OR = 1.4, 95% CI: 1.1-1.7) were associated with the presence of CPH.
Table 4 shows the results of the multivariate logistic regression model. After adjusting for other characteristics, it was observed that living in a house with walls of waste material or tin (OR = 2.2, 95% CI: 1.5-3.1), living in an inadequate dwelling (OR = 2.0, 95% CI: 1.4-2.9), have a family of> 4 members (OR = 1.4, 95% CI: 1.0-1.8) and have an age> 5 years (OR = 1, 4, 95% CI: 1.1-1.8) were associated with the presence of CPH.
Discussion
The present study found a high prevalence of CPH and a relatively low prevalence of parasitosis in children aged 1-7 years, from the ENC-CNCC of the South Central Region. No statistically significant differences were found in the prevalences of parasitosis or CPH according to sex, nor according to the adscription program (CCP, FFD, CCP + FFD), but according to the center, with CNCC La Uruca having the highest prevalence, both of parasitosis as of CPH. Among the few studies of parasitosis performed on children of ENC-CNCC in the Greater Metropolitan Area of Costa Rica, the study by Reyes (1987), which reported high prevalences of Giardia intestinalis (25%), Entamoeba histolytica (16%), stands out, Ascaris lumbricoides (25%) and Trichocephalus trichurus (37%).18 The present study showed a prevalence of parasitosis close to that reported for children from 0-6 years old to the last ENN of Costa Rica in 2008-2009 (8.5%), 10 but lower than the prevalences observed in other vulnerable child populations in Latin American countries (30-90%).24,25 As in other studies conducted in Costa Rica, in this research Giardia intestinalis was the most prevalent pathogenic protozoan and the most frequent commensal protozoa were Endolimax nana and Entamoeba coli. 10,18,26 The prevalence of helminthiasis found in the study (0.7%) was lower than that reported for Costa Rica (2.6%) in the NNH of 2008-2009.10 Unlike the ENN, in the stool samples collected in this investigation no hooks were found nor Taenia sp. and two cases were detected of Hymenolepis nana. Ascaris lumbricoides was the most prevalent helminth, a finding that is consistent with what has been observed in some studies carried out in Costa Rica,20,27 but inconsistent with the findings of the 2008-2009 NNE and other national investigations that report Trichocephalus trichiurus as the most prevalent helminth.10,26
Table 4 Model of best fit for the socioeconomic characteristics associated with the presence of CPH in the beneficiary children CCP-FFD of the Central South Region, 2014-2016 (n = 1281)
Despite the low prevalence of parasites found in the study, almost a quarter of the children had CPH; Other studies conducted in Costa Rica have found prevalences of CPH between 20% and 80% in preschool and school populations.20,26,28,29 However, determining the true prevalence of CPH is difficult when analyzing a single stool sample; As observed in the study, in children who presented 2 stool samples, the prevalence of CPH increased significantly, so it can be expected that in other studies also the actual prevalence of CPH is higher than that reported. This has been explained because the cycles of excretion of the parasites in the feces are not continuous, which implies that the parasites are not excreted in the feces daily and hence the importance of performing serial analyzes of stool samples.30,31 The CPH category includes commensal protozoa, which, although not pathogenic, are indicators of ingestion of fecal matter and the risk of being parasitized or of contracting an infection with enteroparasites. In the study, as in other investigations,26,27 the majority of CPH found in the feces were protozoan commensals and a small percentage, pathogenic protozoans or helminths. The high percentage of commensal protozoa could be due to the massive deworming campaigns that take place in the country.32 In these campaigns albendazole is used as an antiparasitic, which is effective against some of the helminths, but not against protozoa, except Giardia intestinalis, in which its effectiveness is limited, since it requires a greater dosage.34,35
The children assigned to CNCC La Uruca had the highest prevalences of CPH and parasitosis, which seems to be related to poor socioeconomic conditions, since the children of CNCC La Uruca, as well as the beneficiaries of the FFD program, showed a greater proportion of families classified in risk categories for these variables. No statistically significant differences were found in the prevalence according to the program to which the child belonged (CCP, FFD, CCP + FFD), despite the fact that there was a trend towards higher prevalences in the FFD beneficiaries, according to the absolute numbers.
In the study, socioeconomic factors such as having an age> 5 years, having a family with more than 4 members, living in an inadequate dwelling (indigenous dwelling, quarter in barracks, slum, mobile home, boarding house or convent) or in a House with walls built with waste materials or tin, were determining factors to present CPH. The association of these socioeconomic factors with parasitosis has been explained by other authors who mention that older children may be more exposed to risk factors for parasitosis;34,35 large families are more likely to live in crowded conditions, which facilitates the spread of parasites,21,33 and that the condition of housing and walls are commonly a risk factor for infant mortality and parasitosis.34,37 Other socioeconomic factors such as: that the father of a family has an educational level of primary or lower or living in a house with a dirt floor, were also risk factors for CPH, but only in the bivariate analysis. The literature indicates that a low educational level of parents is related to poor hygienic practices36,38 and that the earth floor is a risk factor for parasitosis, since it provides an adequate means for the development and transmission of geohelminths and favors, in turn, the transmission of protozoa of zoonotic origin.39,40 Although other studies point to the low level of sewage or poor disposal of excrement25,41 and the inadequate quality of the water25,41 as risk factors to have parasites or commensals, in this investigation the source of water supply of the house, presence of piped water to the home and type of sanitary service, were not associated with CPH, possibly due to the homogeneous distribution of said factors in the studied population.
Although intestinal parasitosis is a preventable and treatable disease, which has been reduced significantly in Costa Rica, there are still major weaknesses in its approach. Some of these weaknesses include: lack of a standardized protocol for the care of parasitosis, few therapeutic options (i.e., albendazole, metronidazole and ivermectin),42 scarce research on the subject and poor training of health personnel in the care and treatment of these diseases. Another significant weakness is that empirical treatment is commonly provided for intestinal parasitosis, which is rarely supported by a previous demonstration of infection by parasites.43
Among the limitations of the study is that the socioeconomic information, information about deworming and about the child’s medical care, was referred by their father or guardian, and not through a verification of the houses, for which there may be information bias. It is also not possible to eliminate the conglomeration effect of children (similarity of children belonging to the same center) for the calculation of total prevalence, since a study design by conglomerates was not used. Some strengths of this research include the large number of children analyzed, the support of a team of specialist parasitologists for the analysis of the samples, the collection of socioeconomic data in parallel to the analysis of stool samples, as well as the verification of the care medical of children. This research, beyond generating updated data on parasitosis in children aged 1-7 years in vulnerable condition, is a wake-up call, since it shows that in many regions of our country there are still permissive conditions for the transmission of enteropathogens (evidenced by the presence of commensal protozoa in almost a quarter of children). In addition, there is a need to encourage the use of serial analysis of feces, strengthen the preventive measures of parasitosis, develop protocols for its approach and design a strategy that includes the preschool population within the programs that evaluate the child’s development periodically.
REFERENCES
1. Mata L. Erradicación de helmintos intestinales en Costa Rica. Rev Med Hosp Nal Niños Costa Rica. 1985; 20:151-64. [ Links ]
2. Navarro Rojas P, Reyes Romero H. Infecciones parasitarias en la frontera del tercer milenio. Rev Fac Med Caracas. 2000; 23:9-10. [ Links ]
3. Lucero T, Álvarez L, Chicue J, López D, Mendoza C. Parasitosis intestinal y factores de riesgo en niños de los asentamientos subnormales, Florencia- Caquetá, Colombia. Rev Fac Nac Salud Pública. 2015; 33:171-80. [ Links ]
4. Solano L, Acuña I, Barón M, Salim AMD, Sánchez A. Influencia de las parasitosis intestinales y otros antecedentes infecciosos sobre el estado nutricional antropométrico de niños en situación de pobreza. Parasitol Latinoam. 2008; 63:12-9. [ Links ]
5. Zonta M, Navone G, Oyhenart E. Parasitosis intestinales en niños de edad preescolar y escolar: situación actual en poblaciones urbanas, periurbanas y rurales en Brandsen, Buenos Aires, Argentina. Parasitol Latinoam. 2007; 62:54-60. [ Links ]
6. Comisión Económica para América Latina y el Caribe (CEPAL). Panorama Social de América Latina. 2017. Santiago: Naciones Unidas, 2018. En: En: http:// repositorio.cepal.org/bitstream/handle/11362/42716/4/S1800002_es.pdf [ Links ]
7. Cerdas C, Araya E, Coto S. Parásitos intestinales en la Escuela 15 de agosto, Tirrases de Curridabat, Costa Rica. Mayo-junio de 2002. Rev Costarric Cienc Médicas. 2003; 24:127-33. [ Links ]
8. Botero D, Restrepo M. Parasitosis humanas. 4ta ed. Colombia: Corporación para Investigaciones Biológicas; 2003. [ Links ]
9. Ledesma AE, Fernández G. Enteroparasitosis: factores predisponentes en población infantil de la Ciudad de Resistencia, Chaco. Bol. Inst. Med. Reg. 2001; 42-44. [ Links ]
10. Ministerio de Salud. Encuesta Nacional de Nutrición 2008-2009, 2009. Recuperado en octubre 2017. Disponible en: https://www.google.com/ webhp?sourceid=chrome-instant & ion=1 & espv=2 & ie=UTF-8#q=Encuesta+nac ional+de+nutrici%C3%B3n+2008-2009 [ Links ]
11. Cañas M, Mora G, Navarro A, Ruiz E, Solano R, Usaga D. Programas no formales para la atención integral a la niñez en Costa Rica: aciertos y limitaciones. Rev Electrónica Actual Investig En Educ. 2007; 7:1-26. [ Links ]
12. Ministerio de Salud. Modelo conceptual y estratégico de la Dirección General de Nutrición y Desarrollo Infantil. 2008. Recuperado en octubre 2017. Disponible en: Disponible en: http://www.cen-cinai.go.cr/index.php/cen-cinai/modelo-conceptual-y-estrategico . [ Links ]
13. Ministerio de Salud. Dirección Nacional de Centros de Educación y Nutrición y Centros Infantiles de Atención Integral, Costa Rica. Preguntas más frecuentes. 2011. Recuperado en octubre 2017. Disponible en: Disponible en: http://www.cen-cinai. go.cr/index.php/preguntas-frecuentes [ Links ]
14. Organización Panamericana de la Salud. Informe Taller sobre la integración de la desparasitación en los paquetes de atención en salud para niños en edad preescolar en las Américas. 2011; 77. [ Links ]
15. Montresor A, Crompton DWT, Hall A, Bundy D a P, Savioli L. Guidelines for the Evaluation of Soil-transmitted Helminthiasis and Schistomiasis at Community Level. WHO. 2012; 1:48-48. [ Links ]
16. Ministerio de Planificación Nacional y Política Económica. Dirección Nacional de CEN-CINAI. CEN-CINAI Perfil socioeconómico de las familias y personas usuarias 2014. 2016. Recuperado en enero del 2018. Disponible en: Disponible en: https://documentos.mideplan.go.cr/alfresco/d/d/workspace/SpacesStore/ ab090d65-2b53-4d05-b594-4c41ca3b07aa/CEN-CINAI_PERFIL_ SOCIOECONOMICO.pdf?guest=true [ Links ]
17. Carmona K, González G, Monge I, Rojas F, Sáenz I, Trejos J. Encuesta de Seguimiento del Gasto Público: Programas CEN-CINAI y Comedores Escolares. 2007. Recuperado en enero de 2018. Disponible en: Disponible en: http://www.iice.ucr. ac.cr/DOC3-INFORME_Final-nov.pdf [ Links ]
18. Reyes L, Marín R, Catarinella A, Vargas A, Valenciano E, Albertazzi C, et al. Parasitosis intestinal en niños En Guarderías de San José, Costa Rica. Rev Costarric Cienc Médicas. 1987; 8: 123-8. [ Links ]
19. Cabrera M, Obando X. Parasitosis intestinal en 330 niños de Upala. Rev Méd Costa Rica Centroam. 1996; 63: 109-14. [ Links ]
20. Arévalo M, Cortés X, Barrantes K, Achi R. Prevalencia de parasitosis intestinal en niños de la comunidad de Los Cuadros, Goicoechea, Costa Rica: 2002- 2003. Rev Costarric Cienc Méd. 2007; 28:37-45. [ Links ]
21. Instituto Nacional de Estadística y Censos (INEC). Encuesta Nacional de Hogares 2014. 2014. Recuperado en octubre 2017. Disponible en: Disponible en: http:// sistemas.inec.cr/pad4/index.php/catalog/148 [ Links ]
22. Castro A, Guerrero O. Técnicas de diagnóstico parasitológico. 2a ed. San José, Costa Rica: Editorial de la Universidad de Costa Rica; 2006. [ Links ]
23. Kish L. Survey sampling. 1965. New York Wiley Pty Ltd Google Sch. [ Links ]
24. Amaro M, Salcedo D, Uris M, Valero K, Vergara M, Cárdenas E, et al. Parasitosis intestinales y factores de riesgo en niños. Ambulatorio Tipo II Dr. Agustín Zubillaga Barquisimeto-Lara. Arch Venez Pueric Pediatría. 2011; 74: 010-016 [ Links ]
25. Espinosa M, Alazales M, García AM. Parasitosis intestinal, su relación con factores ambientales en niños del sector “Altos de Milagro”, Maracaibo. Rev Cuba Med Gen Integral. 2011; 27: 396-405. [ Links ]
26. Blanco K, Calderón O. Perfil de parásitos comensales entéricos de comunidades del cantón de Barva, Heredia, Costa Rica. Rev Costarric Salud. 2007; 16: 27- 31. [ Links ]
27. Marín J, Campos M. Parasitosis Intestinal en el Distrito de Chomes, Provincia de Puntarenas. Rev Med Hosp Nal Niños Costa Rica. 2005; 40:20-24. [ Links ]
28. Abrahams E, Solano M, Rodríguez B. Prevalencia de parásitos intestinales en escolares de Limón Centro, Costa Rica. Rev costarric cienc méd. 2005; 26. [ Links ]
29. Hernández F, Matamoros MF. Parásitos intestinales en una comunidad Amerindia, Costa Rica. Parasitol Latinoam. 2005; 60: 182-185. [ Links ]
30. Walsh J. Problems in recognition and diagnosis of amebiasis: estimation of the global magnitude of morbidity and mortality. Rev Infect Dis. 1986; 8: 228-238. [ Links ]
31. Chappell C, Okhuysen P, Sterling C, DuPont H. Cryptosporidium parvum: Intensity of Infection and Oocyst Excretion Patterns in Healthy Volunteers. J Infect Dis. 1996; 173: 232-236 [ Links ]
32. Vargas González W. Atención primaria de salud en acción: su contexto histórico, naturaleza y organización en Costa Rica. 2006. Recuperado en octubre 2017. Disponible en: http://www.binasss.sa.cr/libros/atencionprimaria.pdf [ Links ]
33. Risco M, Ivan A, Ixora P, Ytalia B, Rodolfo D. Uso del albendazol en el tratamiento de niños infectados con Giardia lamblia. Saber. 2013; 25:73-82. [ Links ]
34. Ávila E. Ávila A, Araujo J, Villareal A, Taren D. Factores asociados a la parasitosis intestinal en niños de la consulta ambulatoria de un hospital asistencial. Rev Mex Pediatr. 2007; 74 : 5-8 [ Links ]
35. Rodríguez G, Hernández E, Rodríguez L. Parasitosis intestinal en niños seleccionados en una consulta ambulatoria de un hospital. Rev Mex Pediatr. 2000; 67: 117-22. [ Links ]
36. Londoño J, Hernández A, Vergara C. Parasitismo intestinal en hogares comunitarios de dos municipios del departamento del Atlántico, norte de Colombia. Bol Mal Salud Amb. 2010; 50: 251-260. [ Links ]
37. Ibáñez Romero E. Caracterización de los niños menores de cinco años que murieron por desnutrición, Costa Rica 2005-2007. Rev Costarric Salud Pública. 2010; 19:70-4 [ Links ]
38. Rodríguez C, Rivera M, Cabanillas Q, Pérez M, Blanco, Gabriel J y Suarez W. Prevalencia y factores de riesgo asociados a parasitosis intestinal en escolares del distrito de Los Baños del Inca, Perú. Rev. UCV-SCIENTIA. 2011; 3:181- 186. [ Links ]
39. Dumba R, Kaddu J, Wabwire F. Intestinal helminths in Luweero district, Uganda. Afri Health Sci. 2008; 8:90-96 [ Links ]
40. Alyousefi N, Mahdy M, Mahmud R, Lim Y. Factors Associated with High Prevalence of Intestinal Protozoan Infections among Patients in Sana’a City, Yemen. PLos One. 2011; 6: 1-7 [ Links ]
41. Calvo O. Laboratorio epidemiológico de parasitología en un centro integrado de salud: cantón de Los Chiles: 1985-1986. Rev Med Costa Rica. 1987; 500: 113-118 [ Links ]
42. Caja Costarricense de Seguro Social, Dirección de Farmacoepidemiología. Lista oficial de medicamentos y normativa. ISSN 1659-3847. 2014. Recuperado en octubre 2017. Disponible en: Disponible en: https://www.ccss.sa.cr/lom [ Links ]
43. Ministerio de Salud. Boletín Estadístico de Enfermedades o Eventos de Notificación Colectiva en Costa Rica del año 2014. 2015. Recuperado en octubre 2017. Disponible en: https://www.ministeriodesalud.go.cr/ index.php/vigilancia-de-la-salud/estadisticas-y-bases-de-datos/notificacion-colectiva/2783-boletin-registro-colectivo-2014/file [ Links ]
Received: October 17, 2017; Accepted: February 12, 2018











 text in
text in