Introduction
Ectodermal dysplasia (ED) defines a group of syndromes characterized by more than 170 clinical signs of congenital defects involving at least 2 structures derived from the embryonic ectoderm (1). The condition is observed in 1 out of 100,000 live births, and it was related to approximately 132 different hereditary genetic syndromes (2-3). Hypohidrotic ED (Christ-Siemens Touraine syndrome) and Hidrotic ED (Clouston syndrome) are the 2 most common forms of ED and are characterized by an X-linked recessive inheritance. Hypohidrotic ED is the most widespread form in humans, and it affects at least 1 in 17,000 people world- wide (4). ED disorders may lead to a combination of symptoms including sparse hair, brittle nails, dental malformations, skin problems, absence of sweat glands, complications of swallowing, vision and hearing (5). Considering the craniofacial district, the most common anatomical features are maxillary hypoplasia, mandibular protrusion, midface depression, reduced facial height, frontal bulging, abnormal or missing sweat glands, hypotrichosis, dry skin, protuberant lips, saddle nose (6-7). Furthermore, oral manifestations are also frequently observed including hypodontia, defective enamel, peg shaped teeth, delayed dental eruption and severe alveolar ridge deficiency (8). Hypodontia is the most frequently found sign of oral anomalies, with an estimated prevalence of 80% in ED patients (9,10,11). All these alterations can hinder the mastication, and as a consequence reduce nutritional intake. Furthermore, the craniofacial signs can lead patients to low self-esteem, psychological issues, and reduced social connections (7). Prosthodontic treatment options include tooth- and partial implant-supported fixed dental prostheses and removable partial protheses in case of hypodontia, while complete-arch implant- supported fixed dental prostheses and dentures are recommended in case of anodontia (3). Different factors have to be taken into account during the reconstruction strategy including patient age, developmental stage, soft and hard tissues anatomy, and number of missing teeth (7). Although ED patients are featured with anatomical alterations of the cranio facial districts in terms of bone volume, implant therapy seems to be the best option, even though a higher failure risk has been noticed in patients younger than 18 years (12,13,14,15,16,17). Teeth absence affects the alveolar bone development making it difficult to fabricate stable dentures and at the same time dental implant placement could be complicated, due to the reduce amount of bone available, often requiring bone grafting procedures before implant placement (10-11, 18,19,20).
Different grafting procedures have been proposed to increase the amount of bone available for implant insertions such as autogenous bone grafts, guided bone regeneration (GBR), maxillary sinus lifts, and distraction osteogenesis. There is no agreement on the clinical applications of the reported methodologies and relative outcomes of bone augmentation (7, 21,22,23).
Besides, different disadvantages have been reported when performing bone grafting procedures including donor site morbidity, unpredictable resorption of grafting, staged placement of implant, and prolonged therapy (24).
The bone grafting limitations and drawbacks suggested the search of alternative anchoring sites for dental implants (25,26,27,28). Zygomatic bone was proposed as a potential implant site when dealing with the upper jaw, even if ED was proven to produce thickness and length alterations also to the zygomatic bone, suggesting the center of the zygoma close to the infraorbital area as the best anchoring site (29).
The placement of zygomatic implants in ED patients showed a survival rate from 95.1% to 100%, so it was suggested as a potential alter- native to bone grafting procedure in the upper jaw even if difficulties were observed for the “quad approach” (30,31,32,33).
The present study describes the application of an immediately loaded quad zygomatic approach in the upper jaw of an ED patient through the use of a surgical template derived from computer guided implant planning.
Relevant sections
A 32-year-old Caucasian man diagnosed with ED presented to the dental clinic Policlinico Umberto I of Rome, Sapienza University of Rome. The patient presented with a mobile denture in the upper jaw and an implant supported rehabilitation in the lower jaw, complaining for poor esthetics, masticatory inefficiency and pain, due to the existing removable prosthesis (Figure 1).
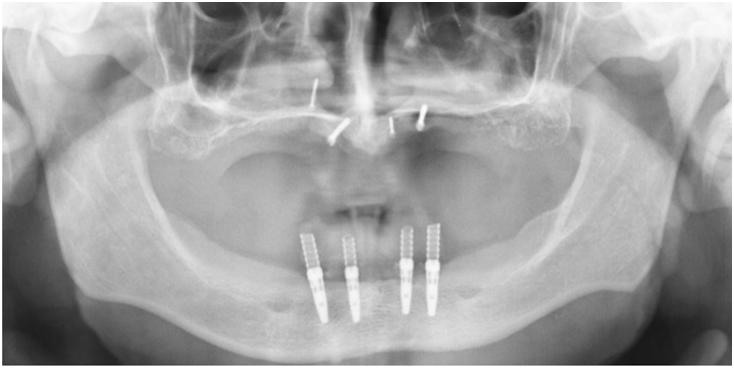
Data collection, including medical history, radiographs, clinical examination, videographic and photographic examinations, was carried out. Preoperative orthopantomography revealed an extreme maxillary atrophy, with little remnant bone (Figure 2).
The patient exhibited typical ED signs, such as alopecia, madarosis, anhidrosis, mild asthma, nasal dryness and hyposcialia. Intraoral findings were edentulism in both deciduous dentition and permanent dentition. A fibro-mucosa hypertrophy lesion on the palate, caused by the incongruous fit of the upper denture, was revealed. In 2008, the patient underwent iliac crest bone grafting in the maxilla. Dental implants were placed in both the upper and lower jaw. The maxillary rehabilitation immediately failed, while an implant supported rehabilitation was delivered in the mandible. A removable denture was then delivered in the upper jaw. The patient request was to solve both the esthetic and the functional problems, which had not been resolved with a conventional removable denture. The upper denture was properly relined and adhesive anatomical landmarks were placed on the flanges. Then it was scanned with an extraoral scanner (EOS) to obtain an standard tessellation language (STL) file of the prosthetic volume (Figure 3).
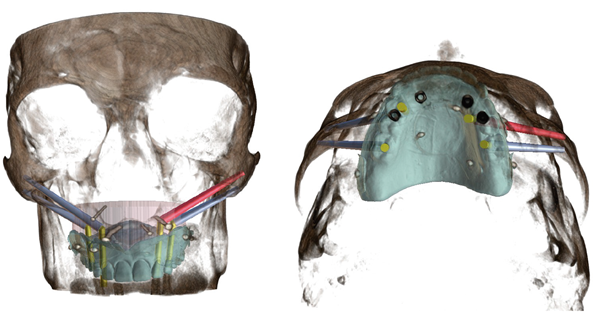
The patient underwent a cone beam compu- ted tomography (CBCT) scan. It was performed wearing the upper denture and a silicon position index to obtain a digital imaging and communication in medicine (DICOM) file including the prosthetic volume position and the bone anatomy.
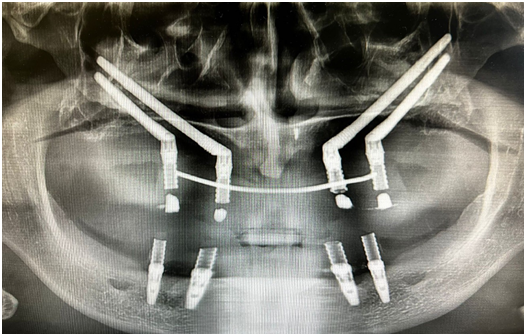
The file gathered were then aligned through the anatomical landmarks on a dedicated software Blue Sky Plan (Blue Sky Bio, Langenhagen, Germany) in order to create a digital implant planning scenario including anatomical and prosthetic data. Due to the severe maxilla atrophy, a quad zygomatic implant-prosthetic rehabilitation for the upper arch was proposed to the patient. Four zygomatic implants were digitally planned, and a surgical template was fabricated to perform a computer guided implant surgery (Figure 4, Figure 5).
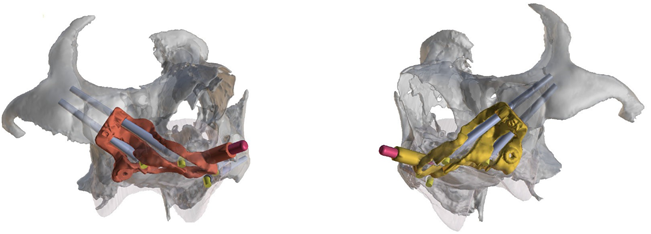
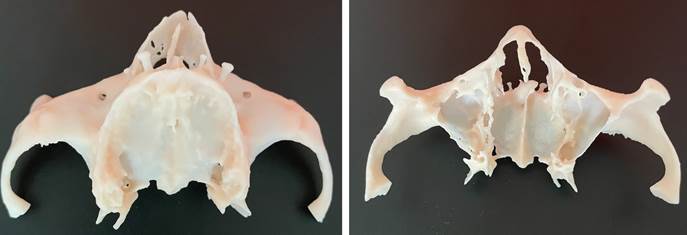
A stereolithographic model was three-dimensionally (3D) printed from the CBCT DICOM file to have better insight into the patient anatomy (Figure 6). Possible difficulties regarding treatment sequence and surgical limitations were discussed with the patient, who finally accepted the treatment plan.
Surgery was carried out under general anesthesia (TL1), with orotracheal intubation, due to the invasiveness of the surgery. Anesthesia was induced by Propofol B. Braun (2mg per kg), then Fentanyl (2mcg per kg) and Esmeron (0,6 mg per kg) were administered. The patient was ventilated with 1% Sevorane in 65% Nitrous Oxide (N2O)/35% Oxygen (O2). Infiltrative local plexus anesthesia with vasoconstrictors was performed palatally and buccally along the maxilla.
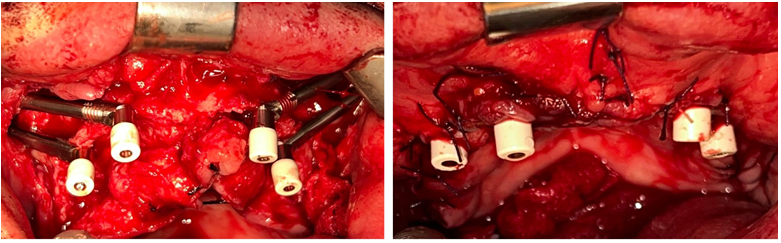
Chlorhexidine rinse and antibiotic prophylaxis with amoxicillin and acid clavulanic 2g (Augmentin, glaxosmithklein, Brentford, UK) by injection were followed before the intervention. The procedure has involved the insertion of 4 zygomatic implants (left and right canine regions, and left and right second premolar regions). Surgery was performed with an open flap: a supracrestal incision was made from one tuberosity to another, from 18 to 28. The 4 residual screws for osteosynthesis, placed in the previous implant-prosthetic rehabilitation, were removed. The positioning and fixation of the surgical template pin was achieved on the right side. Then osteotomy was performed for the implant placement. The pin and the surgical template were removed to allow the site preparation for the insertion of the first 2 implants. The first Zygomatic implant (Straumann, Basel, Switzerland) measuring 55mm of length 4.4mm of diameter was positioned in position 1.3. The second Zygomatic implant (Straumann) measuring 40mm of length 4.4mm of diameter was positioned in position 1.5. The same procedure was performed on the left side, so the positioning and fixation of the surgical template pin was achieved on the left side. Then osteotomy was performed for the implant placement. The pin and the surgical template were removed to allow the site preparation for the insertion of the first 2 implants. The first Zygomatic implant (Straumann) measuring 55mm of length 4.4mm of diameter was positioned in position 2.3. The second Zygomatic implant (Straumann) measuring 52.5mm of length 4.4mm of diameter was positioned in position 2.5. Four healing screws measuring 3.5mm of length were placed.
The surgical procedure was completed by continuous suture and button suture, using Vicryl 3/0 (Ethicon, Jhonson&Jhonson, New Brunswick, NJ, USA) (Figure 7).
The necessary postoperative instructions were discussed. Augmentin (1000mg every 8 hours) was prescribed for 6 days. The patient was informed to follow a cold semi-liquid diet for the first 10 days, and a soft diet for the following 6 months. He was given instructions regarding oral hygiene measures and was followed up at regular intervals of 2, 7, 14, 30, and 60 days. After 48h, implants were loaded, using the previous denture, properly relined onto temporary abutments with the removal of the palatal vault (Figure 8, Figure 9).
No intraoperative and postoperative complications occurred. The patient has been inserted in a strict follow up program. At 1 year follow up no biological nor mechanical complications were reported (Figure 10).
Discussion
Early dental treatment of ED patients is fundamental to provide dentofacial aesthetics and function in terms of language development, chewing and swallowing (34). Deficiency in oral function and facial appearance could lead to a negative impact on the physical and mental well- being of young ED patients, especially during the adolescence (7). Therefore the need of dental treatment is requested at an increasingly younger age, with the frequent premature and long-term use of dentures in ED patients affected by anodontia to enhance self-confidence and quality of life (7). The prolonged use of mobile dentures in growing patients requires frequent adjustments and the deficient supporting anatomy combined with the salivary gland hypoplasia induced xerostomia hamper the prosthesis stability and reduce the young patient tolerance (7). The poor denture stability and the low pediatric patient tolerance often requests the shift from a mobile to a fixed dental prosthesis (5, 35-36). In case of anodontia dental implant insertion timing plays an important role and should consider all the patient-specific aspects, but there is still no consensus about it (5, 37). In the literature dental implant insertion was described already in 4-5 years old patients (5, 37).
Anyway the premature implant placement in patients that still have not completed the craniofacial growth could lead to several issues. An animal study analyzing implant placement in young pigs showed that implants did not follow the growth process of the adjacent teeth resulting in infraocclusion just like ankylosed teeth (42). Therefore, early implant placement could create implant dislocation during the growth and maxillary development issues if implants are fixed together (43).
The greatest maxilla development is a transversal growth at the level of the midpalatal suture, for this reason complete-arch implant supported fixed dental prosthesis could limit the palatal expansion (40). Nevertheless, the mandible is featured with an anteroposterior, transverse and vertical growth in late childhood with a rotational growth (39, 41). As a consequence dental implants could be affected by infraocclusion and dislocation in the anteroposterior direction (39). Concerning dental implants placed in the anterior mandible, changes in implant angulation can occur due to the mandibular rotational growth (4). For all these reasons dental implant placement timing should be determined by the patient’s level of skeletal development, even though early implant placement sometimes was described as necessary to solve the poor function and esthetics of removable dentures (7).
Even if a comprehensive preoperative evaluation is always necessary and customized to each patient, implant supported restorations are considered the treatment of choice in ED patients for their superior function (8). Several authors repor- ted that ED patients showed normal healing and osseointegration rates comparable to healthy controls (10, 12, 22, 34, 43,44,45).
A 5 years survival rate of 95.4% was experienced in ED implants and no statistically significant difference was found in the survival rates of implants placed in ED and non-ED patients (7, 46). However, ED patients usually presented with “knife-edge” morphology of the residual alveolar bone, making implant reconstruction challenging (47). Implant surgery of ED patients usually requires bone grafting and/or sinus augmentation procedures, subjecting the patients to additional morbidity (19, 48). Furthermore, the final esthetic outcome could be compromised by soft tissues limitations and a higher risk for biologic complications has to be taken into account (49).
The use of zygomatic implants in ED patients was suggested as a potential alternative to bone grafting in the upper jaw, even if long-term data outcome are very limited (30-31, 50). Zygomatic implants were first introduced by Branemark as a different solution to stabilize implants in a different anchoring zone of atrophic maxilla patients (51-52). The advantages compared to bone grafting and traditional implant placement include reduction of morbidity, costs and number of surgeries (53,54,55). However, zygomatic implants must be considered a major surgery and potential complications can occur such as sinus and soft tissues infections, paresthesia, oroantral fistula, implant failure and drill penetration in the orbital cavity (33, 51, 54, 56,57,58,59,60,61,62). Furthermore ED patients were proven to show limited development of the zygomatic bone thickness and length, leading to a greater complexity of zygomatic implant surgery (29).
Advancements in 3D radiology, implant planning software and computer aided design computer aided manufacturing (CAD-CAM) technology led to the development of computer guided surgery for zygomatic implants by means of bone supported templates (63). Digital implant planning software allow clinicians to prepare the surgical procedure in advance on a virtual patient, selecting the proper implant types and number according to the bone quantity and quality and at the same time considering the ideal prosthetic volume (64). Furthermore integration of 3D printing technologies with 3D radiology allowed the production of 3D models of the patient anatomy derived from the digital imaging and communication in medicine (DICOM) files to give the surgeon a better insight into the patient anatomical features and to simulate the intervention on a realistic 3D-printed model (65).
The present clinical case describes the zygomatic implant treatment of a complete edentulous ED patients with a story of failing bone grafting in the upper jaw and fixed implant supported prosthesis in the lower jaw. The patient presented with a mobile upper denture, responsible for the development of an hypertrophic lesion of the palate. The CBCT examination highlighted the presence of residual fixation screws of the failing upper jaw bone grafting as well as a sever maxilla atrophy. In order to deliver a fixed dental prosthesis zygomatic implant treatment was proposed. ED was responsible also for an altered development of the zygomatic bones, thus it was decided to properly plan the case with a digital implant planning software to find the best anchoring zones. Furthermore, 3D printed bone model was obtained from CBCT to simulate the intervention and give the surgeon a better insight into the patient anatomy. Although the zygomatic bone was atrophic, the digital implant planning allowed for the insertion of 4 zygomatic implants with a primary stability sufficient for immediate loading. At 1 year follow up no biological nor mechanical complications were observed and the patient referred an improvement in the life quality in terms of function and esthetics.
Conclusions
Zygomatic implant placement in ED patients with atrophic maxilla as an alternative to bone grafting and traditional implant placement and in case of failing bone grafting seems to be a valua- ble option. Zygomatic implant surgery must be considered a complex major surgery with potentially severe complications. The digital implant planning and 3D printing of the patient anatomy are auxiliary tools to enhance the intervention.
Author contribution statement
Conceptualization and design: A.L. and D.G.
Literature review: G.C.
Methodology and Validation: A.L.
Formal analysis: F.F.
Investigation and data collection: G.M.
Resources: T.L.
Data analysis and interpretation: P.P.
Writing-original draft preparation: D.G.
Writing-review & editing: A.L.
Supervision: A.L.
Project administration: G.M.
Funding acquisition: T.L.