INTRODUCTION
Non-Carious Cervical Lesions (NCCL) are characterized by the loss of tooth structure in the cement-enamel junction without being related to an active pathological process of caries. These lesions have been classified as abrasion, erosion, abfraction, attrition, and their possible combinations (1,2). It is considered that the etiology of NCCL is complex and multifactorial. Dietary habits and social lifestyles are part of the many risk factors that have given rise to an increase in the degree of dental wear, therefore to the presence of NCCL. This type of lesion is slow progressing, progressive, and, in the majority of cases, the dental organ forms dentin and achieves isolation from the external environment (3).
Abrasion is a deterioration of the pathological etiology of the tooth structure caused by abnormal mechanical processes, which in turn is caused by foreign objects that, when in contact with the teeth, generate the loss and wear of hard tissues at the level of the cementoenamel junction (4). Erosion or bio-corrosion is the chemical dissolution of dental tissues that does not involve the presence of caries and dental plaque; its etiological factors include acid or chelating agents of intrinsic or extrinsic origin (5). Attrition is the wearing down of dental tissue due to the contact of the teeth during normal or parafunctional activity (6). Another type of wear described by McCoy (1982) is abfraction, derived from the Latin "as a fracture"; the morphology of this type of injury is wedge-shaped in the cement- enamel junction and is caused by eccentric occlusal forces that lead to dental flexion (7,8,9,10).
The integral restorative treatment of a patient with an aesthetic demand can represent a great challenge when the patient presents dentition with generalized NCCL, since the ideal is to propose a minimally invasive one. The treatment of each tooth depends on the type of NCCL and the degree of wear that the tissue presents and whether or not it involves the dentin-pulp complex (11). Treatment planning by segment in the oral cavity of a patient with generalized NCCL in case of loss of vertical dimension, allows us to maintain stable occlusion with provisional restorations that protect the dental organs from mandibular movements (12,13). The objective of this case report was to show and describe the aesthetic restorative rehabilitation of a patient diagnosed with generalized NCCL with ceramic restorations to restore the aesthetics and stable occlusion, describing step-by-step the treatment executed.
CASE REPORT
Male patient, 54 years of age, who is referred to the Specialty in Aesthetic Dentistry, Cosmetic, Restorative, and Implantology of the Faculty of Stomatology, Autonomous University of San Luis Potosí, Mexico, with spontaneous pain in the upper teeth along with NCCL in the upper and lower teeth, compromising the aesthetics and functions of the dentition. His clinical history reports the high and continuous intake of carbonated and acidic beverages, as well as the prolonged consumption of medications during 15 years due to a vehicular accident. Signed informed consent was obtained from the patient to publish his case.
INTRAORAL EXAMINATION
Clinical examination revealed NCCL, anterior cross bite right side and edge-to-edge bite perspective, thick periodontal biotype, middle line deviated to the right, provisional crowns with microfiltration at the cervical level, multiple microfiltered amalgam restorations. The patient was diagnosed with generalized NCCL combined with a loss of the vertical occlusal dimension (Figures 1A, 1B, and 1C). The diagnosis and treatment procedure of each teeth according to the degree of destruction of the dental tissue is shown in Table 1.
PERIODONTAL REHABILITATION
Periodontal phase was performed in the maxilla, which consisted of the extraction of tooth #16 due to an endodontic perforation, and of teeth #25 and #27 due to root caries; tooth #14 was treated endodontically and a fiberglass post was placed for the degree of destruction. Teeth #15, #17 and #26 were treated endodontically by hypersensitivity, and provisional fixed acrylic restorations were placed in the posterior-superior sector for the post-extraction ovoid pontic formation in the zone of teeth #16 and #25 (Figure 1D). Periodontal phase was performed in the lower arch, as well as the removal of amalgam restorations with microfiltration in the occlusal margins of teeth #37, #46, and #47; in addition, extractions of third molars #38, and #48 were indicated (Figure 1E).
TREATMENT PLAN
The treatment plan is based on reducing the factors that led to the formation of NCCL. The treatment goals in this case were to restore the damaged tooth structure and reestablish the function and aesthetics, returning the functional anatomy of each tooth, reconstructing the occlusion with the increase of the vertical dimension lost, restoring the esthetic appearance of the teeth, and reducing the hypersensitivity. Prosthetic rehabilitation was planned and divided by arcades and quadrants. Table 1 depicts the treatment plan for each tooth. With information from the study and waxing models of diagnosis, an increase in the vertical occlusal dimension was made, which is based on the esthetic demand and the functionality of the restoration materials.
AESTHETIC PROTOTYPE ATTACHED OF POSTERIOR-INFERIOR TEETH
Through the use of diagnostic waxing, a transparent silicone guide (Elite Transparent, Zhermeack) was performed for the faithful reproduction of teeth #34, #35, #36, #37, #44, #45, #46, and #47. Relative isolation is performed with Teflon, conditioning with 37% phosphoric acid for 15s, washing and drying in order to apply adhesive (AdperTM Single Bond, 3M), photocuring, and the transparent silicone guide was inserted. The fluid composite was injected until it completely fills the space occupied by the wax, this is photocured for 10s, the guide is removed, the excess material is cut in the cervical and interproximal area, and then photocured for 20s per face. Polish and trimming by interproximal, then glycine (DeOx, Ultradent) is set in place to inhibit the last layer of oxygen (Figures 2A, 2B, and 2C). This procedure was performed individually in teeth #34, #35, #36, #37, #44, #45, #46, and #47.
PROVISIONALIZATION OF THE POSTERIOR- SUPERIOR TEETH
The biomechanical preparation of tooth #14, #15, #17, #24, and #26 (Figures 3A and 3B) was performed with round and fine-grain, round-core diamond nose burrs (Brassleer) to set definitive restorations in place with zirconium cores stratified with feldspathic porcelain; temporary restorations of thermocurable acrylic are adjusted, occlusal adjustments are carried out and were cemented with temporary material (PreVISION CEM, Heraus Kulser). In this manner, the upper and lower posterior sectors are provisionally increased and the vertical dimension is increased (Figures 3C and 3D).
PROVISIONALIZATION OF THE ANTERIOR-SUPERIOR TEETH
The mock-up was placed on teeth #13, #12, #11, #21, #22, and #23 from the diagnostic wax for the biomechanical preparations of individual pressed lithium disilicate crowns (IPS e.max System, Ivoclar Vivadent), guide grooves were marked, wear was continued with medium and fine diamond cutters (Brassleer), respecting the juxtagingival cervical margins, with the mesial and distal preparations extending toward the tongue where the intention is to close diastemas and to polish the stumps with carbide burs (Figure 4A). The final impressions were taken with the two-step technique of two steps, with two consistencies (polyvinyl siloxane, putty and light) prior to the placement of retractor wires (#000 and #00). Individual provisional restorations with bis acrylic material (ProtempTM 4, 3M) were set in place and electronic information was sent to the Laboratory to ascertain the color of the substrate.
PROVISIONALIZATION IN THE ANTERIOR-INFERIOR TEETH
The mock-up is placed on teeth #33, #32, #31, #41, #42, and #43 for the carving of vestibular veneers of feldspathic ceramics; guide grooves are marked on the vestibular wall, and next the dental wear is treated with medium- and fine- grain diamond burrs (Brassleer), respecting the juxtagingival cervical margins, and the carvings are polished (Figure 4B).
PROVISIONALIZATION OF THE POSTERIOR- INFERIOR TEETH
Once the increase in vertical dimension is maintained, the esthetic prototype attached to the posterior-lower sector is removed to perform the biomechanical preparation of teeth #34, #35, #44, and #45 with medium- and fine-grained diamond burrs (Brassleer) for occlusal veneers, and teeth #36, #37, #46, and #47 for crowns of pressed lithium disilicate restorations (IPS e.max System, Ivoclar Vivadent) (Figures 4C and 4D). Provisional restorations of self-healing acrylic are set in place.
ADHESION OF FELDSPATHIC VENEERS IN THE ANTERIOR-INFERIOR SECTOR
The restorations of the veneers were tested on the teeth to make any necessary interproximal adjustment, for which the use can be made of pastes such as Variolink Veneer Try in (Ivoclar, Vivadent) or some agent with glycerin (DeOx, Ultradent), to simulate the post-cementing results. The adhesion protocol is described in Table 3.
ADHESION OF LITHIUM DISILICATE PRESSER CROWNS IN THE POSTERIOR-INFERIOR AND ANTERIOR-SUPERIOR TEETH
The same adhesion protocol used in the feldspar veneers of the anterior-lower sector is applied: however, only 9% hydrochloric acid (Porcelain-Etch, Ultradent) is applied to the unpolished surface of the crown for 20s, because it is a porcelain of pressed lithium disilicate, and the resin cement (RelyXTM Venner Cement, 3M) is placed on the silanized surface of the crown.
CEMENTATION OF FELDSPAR CROWNS WITH ZIRCONIUM NUCLEUS IN THE POSTERIOR-UPPER SECTOR
First, the crowns are tested and dental floss is placed in the interproximal areas of the stumps, in that this will facilitate the elimination of cement residues. Glass ionomer cement (Ketac Cem, 3M) was employed following the manufacturer’s specifications, and the crowns are placed on the stumps pressing the occlusal surface. Then a roll of cotton is inserted so that the patient is able to aid us in pressing down until the material has finished its hardening time. The surplus cement and interproximal dental threads are removed. Finally, the occlusion is newly reviewed, providing incisive and canine guides for a mutually protected occlusion. Finally, oral hygiene instructions are indicated to the patient (Figures 5A, 5B, and 5C).
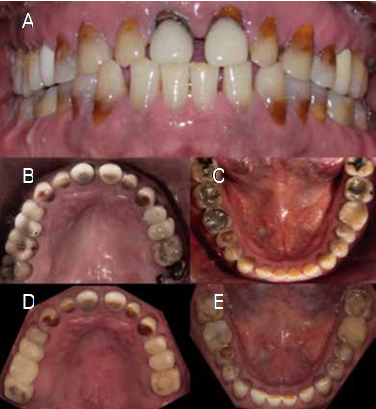
Figure 1 Intraoral clinical evaluation of the initial conditions of the patient, frontal, upper occlusal (B), lower occlusal (C), posterior to periodontal healing eliminating the defective restorations of the upper occlusal (D), and lower occlusal (E).
Table 1 Individual diagnosis, treatment plan, and type of restorative material for each tooth. Feldspathic with zirconium core (FZC), Pressed lithium disilicate (PDL), Feldspathic (FE).
| Tooth | Diagnosis | Treatment | Material | Tooth | Diagnosis | Treatment | Material |
|---|---|---|---|---|---|---|---|
| 18 | Caries | Dental extraction | --- | 28 | Absent | --- | --- |
| 17 | Amalgam with microfiltration | Endodontics Crown | FZC | 27 | Root rest | Dental extraction | --- |
| 16 | Improper metal- porcelain restoration, Furca drilling | Dental extraction (Crown-pontic) | FZC | 26 | Restoration with composite and microfiltration | Endodontics Crown | FZC |
| 15 | Improper metal- porcelain restoration | Endodontics Crown | FZC | 25 | Root caries | Dental extraction Crown (pontic) | FZC |
| 14 | Erosion, Abfracción (NCCL) | Endodontics Fiberglass post Crown | FZC | 24 | Erosión Abfraction (NCCL) | Endodontics Crown | FZC |
| 13 | Erosion, abfraction (NCCL) | Unit crown | PLD | 23 | Erosion, Abfraction (NCCL) | Unit crown | PLD |
| 12 | Erosion, abfraction (NCCL) | Unit crown | PLD | 22 | Erosion, Abfraction (NCCL) | Unit crown | PLD |
| 11 | Provisional crown with microfiltration, Erosion, (NCCL) | Unit crown | PLD | 21 | Provisional crown with microfiltration, Erosion, (NCCL) | Unit crown | PLD |
| Tooth | Diagnosis | Treatment | Material | Tooth | Diagnosis | Treatment | Material |
| 48 | Amalgam with microfiltration | Dental extraction | --- | 38 | Amalgam with microfiltration | Dental extraction | --- |
| 47 | Amalgam with microfiltration (NCCL) | Unit crown | PLD | 37 | Amalgam with microfiltration - Erosion, (NCCL) | Unit crown | PLD |
| 46 | Amalgam with microfiltration-Erosion (NCCL) | Unit crown | PLD | 36 | Cuspidal fracture, Erosion, (NCCL) | Unit crown | PLD |
| 45 | Erosion Abfraction (NCCL) | Occluso- vestibular veneer | PLD | 35 | Erosion Abfraction (NCCL) | Occluso- vestibular veneer | PLD |
| 44 | Erosion Abfraction (NCCL) | Occluso- vestibular veneer | PLD | 34 | Erosión Abfraction, (NCCL) | Occluso- vestibular veneer | PLD |
| 43 | Erosion Abfraction (NCCL) | Veneer | FE | 33 | Erosion Abfraction, (NCCL) | Veneer | FE |
| 42 | Erosion (NCCL) | Veneer | FE | 32 | Erosion, (NCCL) | Veneer | FE |
| 41 | Erosion (NCCL) | Veneer | FE | 31 | Erosion, (NCCL) | Veneer | FE |
Table 2 Adhesion and cementation protocol for pressed lithium disilicate restorations.
| Protocol of adhesion of feldspar veneers in the anteroinferior sector | ||
|---|---|---|
| Hydrofluoric acid at 9% (Porcelain Etch, Ultradent) on the unpolished surface of the veneer. | 60 seconds | |
| Etch and rinse at 37% phosphoric acid (Ultra tch, Ultradent) on the veneer. | 30 seconds | |
| Wash to remove porcelain residues resulting from acid etching. | ||
| Drying with hot air and placement of silane (Silane, Ultradent) on the veneer, which will be applied three times on the surface for the impregnation of the silicon particles. | 60 seconds | |
| Relative insulation and retractor thread to control fluids in the furrow and facilitate the removal of the cement. | ||
| 37% phosphoric acid etching on enamel. | 30 seconds | |
| Flushing the surface of the enamel with a water jet. | 30 seconds | |
| Apply air to the enamel surface. | 15 seconds | |
| Place adhesive (Adper Single Bond, 3M) on the surface of the enamel with a microbrush and apply air to remove the solvent, do not light-cure. | ||
| Place the resinous cement on the silanized surface of the veneer (RelyX Venner Cement, 3M). | ||
| Remove excess with a brush, light cure in the cervical area for 5 seconds. | ||
| Remove excess cement with a No. 15 scalpel blade and place glycerin (DeOx, Ultradent) in the margin to remove the inhibited layer of oxygen. | ||
| Light-cure the surface. | 40 seconds | |
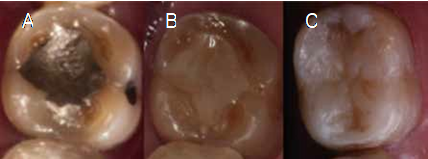
Figure 2 Tooth #37 with an amalam restoration that presents microfiltration (A), elimination of the defective restoration and a conventional composite was set in place (B), the aesthetic prototype is adhered, this procedure was performed individually in the posterior-inferior sectors from both sides of the arch (C).

Figure 3 Biomechanical preparation of teeth #14, #15, and #17 (A), and #24 and #26 (B) for feldspar crowns with zirconium cores. Provisional acrylic restorations are placed to maintain the vertical-dimension increase with the prototype attached to the posterior-inferior sectors (C, D).

Figure 4 Biomechanical preparation of the anterior-superior sector for individual pressed lithium disilicate crowns (IPS e.max System, Ivoclar Vivadent) in the anterior superior sector (A), anterior-inferior preparations for feldspathic veneers (B), and preparations of the posterior-inferior sectors for occlusal vestibules in premolars and crowns of pressed lithium disilicate (IPS e.max System, Ivoclar Vivadent) (C-D).
DISCUSSION
The patient in our case report presented generalized and severe NCCL, whose synthetic factors are combinable and complex. The patient had a clinical history of an excessive, prolonged intake of medications and a carbonated and acidic diet. It has been reported that the use of medications causes xerostomia, therefore decreasing the capacity of the saliva buffer (14). The multiple NCCL caused excessive demineralization of the dental structure, thus the loss of vertical dimension. Therefore, restoring and returning the function is key to the success of the prosthetic rehabilitation.
The NCCL comprise the most common type of injury that causes dentine exposure in the cervical margins of the teeth, with dentine hypersensitivity being one of the most common symptoms, among others. The damage of dental erosion on dentition in this case was restored with fixed prosthesis utilizing ceramic systems. The correct diagnosis should be made on the basis of the etiology and the clinical characteristics of NCCLs (16). The treatment depends on the indication of the restored material, the depth and commitment of the affected tissue, as well as the clinical symptomatology. Several treatment modalities can be performed depending on the severity of the tooth-structure loss, such as direct restorations of composites, laminated veneers, and complete crowns (17).
When NCCL affect only the clinical crown, the recommendation is to perform a prosthetic restoration; however, if the NCCL only affects the root, it is commonly associated with a gingival recession caused by foreign objects (18) and by a defective brushing technique (19).
Schulyer et al. (2001) describe that NCCL treatment options depends on whether or not there is a loss of the vertical dimension (20); when the dimension loss is less than 2 mm, direct restorations of composites are recommended, while crowns are indicated for a more than 2mm (21).
In this clinical case, because the NCCL affected the clinical crowns and there was a loss of vertical dimension, it was decided to perform a fixed prosthetic rehabilitation with crowns, vestibulo- oculsal veneers, and conventional veneers, in an intent to be minimally invasive. The patient, when demanding an aesthetic rehabilitation, decides to use materials that offer excellent fit, function, and esthetic results, combined with high resistance and that require minimal preparation of the tooth.
It has been reported that provisional restorations evaluate the responses of the muscles of mastication to stabilize the occlusion during the increase of the vertical dimension (22). In this clinical case, it was decided to elevate the vertical dimension using the aesthetic attached prototype in the posterior-lower sector and provisional partial fixed prosthesis in the posterior-upper sector, in order to later place the mockup in the anterior and inferior sectors. On the other hand, because this patient consumed carbonated beverages and acids in his daily diet, emphasis should be placed on the change of diet and food intake, in that this is essential for the success of treatment. Studies have shown that beverages with a low pH, such as carbonated beverages, decrease the hardness of enamel and dentin (23). It has been reported that carbonated beverages can reach a pH of approximately 3.0 due to the content of phosphoric acid and citric acid, while the frequency and prolonged time of intake renders them highly corrosive for dental tissues (24).
CONCLUSION
In this clinical case, we show the management of a patient with generalized NCCL and multiple factors that caused the loss of vertical occlusal dimension. When performing rehabilitation with ceramic materials, we maintained an interaction with the mechanical properties of these and provided adequate masticatory function and esthetics, according to the patient’s expectations. We must always base our clinical cases on the evaluation of all of the diagnostic elements, specifically in patients with NCCL, in that the management of this type of lesion is based on clinical evidence and also, based on the diagnosis and treatment plan, it will achieve favorable results. The knowledge of protocols for the elevation of the vertical occlusal dimension based on diagnostic waxing will provide us with a prescient guide in the reconstruction of lost dental structure. The postoperative follow-up is important in order to monitor the change of the habits in the patient. The diagnostic bases are fundamental evidence for proposing a treatment plan and for predicting a successful long-term rehabilitation and a more predictable result.















