Introduction
External tooth whitening (TW) is nowadays a common cosmetic procedure which is designed to reduce the body color of the tooth (Tredwin et al. 2006). TW can be applied as in-office or at-home procedures with effective and satisfactory results in color improvement for patients. While both strategies have been considered safe, the effectiveness of at-home whitening protocols is uncertain and several adverse effects have been reported such as cervical resorption, soft tissue burns, increased dental porosity, dental hypersensitivity, pulp inflammation and even necrosis (Eachempati et al., 2018; Alqahtani et al., 2014; Costa et al., 2010; Rodrigues et al. 2018).
An increased concern for whiter teeth in patients has also been reported by orthodontists. A survey in 1182 orthodontists reported that 88.8% of orthodontists had patients who requested tooth whitening, and 76.2% of orthodontists recommended whitening procedures (Slack et al., 2013). The most frequent reason for the recommendation for in-office TW in orthodontic patients is the presence of white-spot lesions adjacent to brackets or after the debonding of brackets (Guzmán-Armstraog et al., 2010). In addition, tooth color changes around brackets are frequent, resulting in a non-uniform tooth shade after bracket debonding (Kamber et al., 2018). Hence, color changes during or after orthodontic treatment (OT) affects the aesthetic result. However, most suggestions for TW in orthodontic patients have been extrapolated from in vitro and few in vivo studies on the debonding effect on brackets after the application of whitening agents (Imani et al., 2020; Mullins et al., 2009). Consolaro et al. (2013) in a critical review suggested that TW procedures should be best performed after brackets are removed to allow for the balance in the oral environment after orthodontic treatment. In addition, the authors recommended against TW during orthodontic treatment due to the limited penetration of the whitening agent under bracket surface. Nevertheless, there is no clear evidence-based recommendation for the use of TW during or after orthodontic treatment. Therefore, the objective of this systematic review was to identify and critically evaluate the available evidence of the appropriate moment to perform tooth whitening in conventional orthodontic patients.
Methodology
The protocol for this systematic review is in fulfillment with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines.
Research question
What is the appropriate moment to perform tooth whitening in conventional orthodontic patients?
Search strategy and limits
Two calibrated independent reviewers (SH, MFN) searched MEDLINE via PubMed and SciELO (gray literature) from inception to February 2021 using the medical subject heading (MeSH) terms and keywords: (dental bleaching (Title/Abstract)) OR dental whitening (Title/Abstract) OR tooth bleaching (Title/Abstract)) OR tooth whitening (Title/Abstract) AND orthodontic treatment (Title/Abstract). The reference list of potential articles was manually searched for additional results.
Articles written in Spanish, English and Portuguese corresponding to randomized clinical trials (RCT), non-randomized clinical trials (non-RCT), case control, cohort, cross-sectional, case series and previous systematic and critical reviews that focused on the application of tooth whitening during or after orthodontic treatment were considered for inclusion. Case reports, in vitro, and animal studies were not considered in this systematic review.
Population, intervention, and comparator
Target population included patients under orthodontic treatment with no restriction of age.
The intervention considered for analysis was defined as external tooth whitening performed in-office by a clinician during or after conventional orthodontic treatment. In-office interventions may have been continued by the patients with at-home whitening agents as instructed by the clinician. Non-vital tooth whitening was not considered for analysis. Clinical studies which evaluated debonding force resistance of brackets after tooth whitening and tooth whitening during clear aligner orthodontics were also not considered.
This review examined interventions with comparators groups which included no intervention or intervention performed at different time intervals or with different whitening agent during or after orthodontic treatment.
Outcomes
This review aimed to identify, and critically assess the findings related to the most appropriate moment to perform tooth whitening in conventional orthodontics patients.
Therefore, the primary outcome was the application of tooth whitening during/after orthodontic treatment as a dichotomic result. A secondary outcome included the time in days after bracket debonding in which tooth whitening was performed.
Data extraction
Two independent reviewers (SH, MFN) extracted the information from studies that met the inclusion criteria in a predetermined form which comprised: study identification, objective, age of participants, sex, number of participants, number of participants in intervention group, number of participants in comparison group, time (days) after bracket debonding in which tooth whitening was performed, tooth whitening during orthodontic treatment (yes/ no), time of tooth whitening after bracket installation and conclusions. Any disagreement between the reviewers was discussed and resolved with a third reviewer (JEB).
Risk of bias (quality) assessment
RCTs were assessed using the Cochrane Risk of Bias version 2 (RoB 2). Each study was assessed, and each domain was judged as low risk of bias, some concerns or high risk of bias. An overall judgment of the study was determined as low risk of bias if all domains were low risk; some concerns if at least one domain raised some concerns but not be high risk; and high risk of bias if at least one domain was high risk.
Non-RCTs were assessed using the Cochrane Risk of Bias In Non-Randomized Studies of Interventions (ROBINS-I) tool. Each study was analyzed using the critical domains and judged as low, moderate, serious, and critical risk of bias. A study was judged as low risk of bias if all domains
were low risk; moderate risk of bias if all domains were low or moderate risk; serious risk of bias if at least one domain was at serious risk; critical risk of bias if at least one domain was at critical risk. Critical reviews were not quality assessed.
Data synthesis and analysis
Meta-analysis was not attempted since outcomes were recorded in a qualitative style. Consequently, the findings were synthesized with tabulation and figures, in addition to a narrative summary.
Results
A systematic search in MEDLINE and SciELO yielded 41 potential results after duplicates were removed. The results were screened for the inclusion criteria and 11 were excluded. A total of 30 full-text articles were assessed for eligibility and 22 were further excluded, resulting in 8 articles included in the qualitative synthesis (Figure 1). Excluded records with reasons are presented in the supplementary material 1.
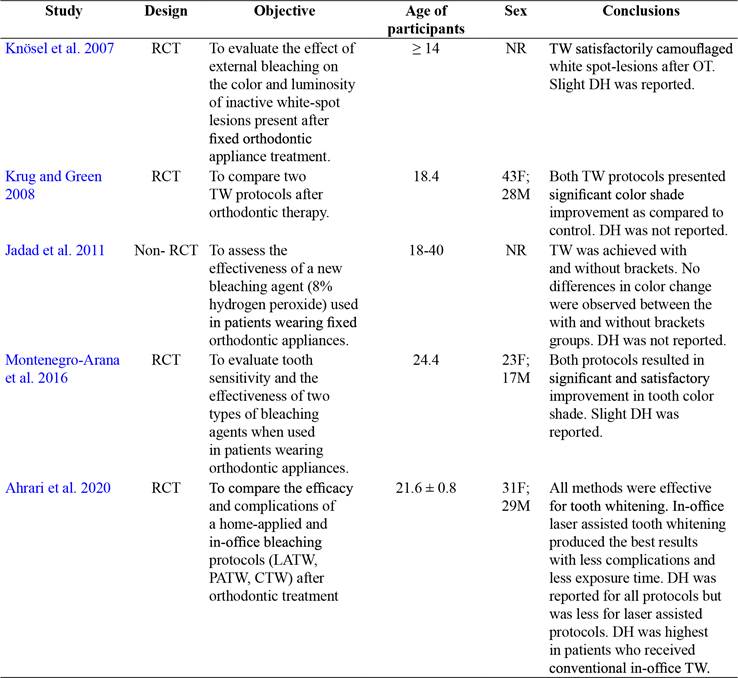
Tables 1,2 and3 depict the characteristics and variables of the 8 included studies and reviews. Four studies were RCTs (Knösel et al., 2007; Krug and Green, 2008; Montenegro-Arana et al., 2016; Ahrari et al., 2020) and one a non-RCT (Jadad et al., 2011). Three results were critical reviews (Consolaro et al., 2013; Márquez et al., 2012; Freire et al., 2018). The age of participants ranged from 14 to 40 years old and were mostly women (table 1).
All clinical studies were small-sample size which comprised 19-71 participants and only one study (Montenegro-Arana et al., 2016) provided information about sample size calculation (table 2). Three studies (Knösel et al., 2007; Krug and Green, 2008; Ahrari et al., 2020) performed tooth
Table 1 Characteristics of the included clinical studies
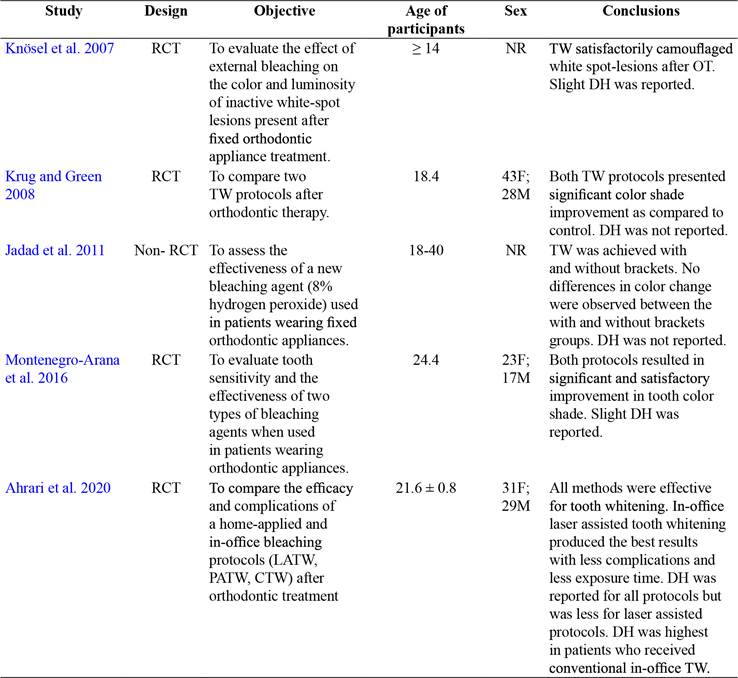
Note: Derived from research. RCT: randomized clinical trial. Non-RCT: non-randomized clinical trial. NR: not reported. F: female. M: male. TW: tooth whitening. OT: orthodontic treatment. DH: dental hypersensitivity. LATW: laser assisted tooth whitening. PATW: plasma arc tooth whitening. CTW: conventional tooth whitening.
whitening (TW) after orthodontic treatment (OT) was finalized (table 2). One study (Montenegro-Arana et al., 2016) performed TW during OT immediately after bracket installation. One study (Jadad et al., 2011) compared TW during OT immediately after bracket installation and TW after brackets debonding (table 2). The time in days after which TW was applied following bracket debonding ranged from 7 to 90 days with a mean value of 40.2 days (Knösel et al., 2007; Krug and Green, 2008; Ahrari et al. 2020) and one study (Jadad et al., 2011) performed TW immediately after bracket debonding (table 2). Studies that applied TW during or immediately (Montenegro-Arana et al., 2016; Jadad et al., 2011) after bracket debonding used lower whitening agent concentration (8-10%). In contrast, studies that performed TW 90 days after bracket debonding (Knösel et al., 2007; Ahrari et al. 2020) used concentrations between 30-46% of the whitening agent (table 2).
Table 2 Variables of the included clinical studies
Note: Derived from research. NA: not applicable. TW: tooth whitening. OT: orthodontic treatment. LATW: laser assisted tooth whitening. PATW: plasma arc tooth whitening. CTW: conventional tooth whitening. *Days after brackets removal. **Days after brackets installation.
All studies reported satisfactory improvements in tooth color shade during or after OT independent of the protocol used with no significant differences among them (Knösel et al., 2007; Krug and Green, 2008; Montenegro-Arana et al., 2016; Ahrari et al., 2020; Jadad et al., 2011) However, the two studies (Montenegro-Arana et al., 2016; Jadad et al., 2011) that performed TW during OT are from the same group of researchers with the same protocol and therefore the external validity remains inconclusive.
Risk of bias for clinical studies is presented in figures 2 and 3. Three studies were judged to have high risk of bias (Knösel et al., 2007; Krug and Green, 2008; Jadad et al., 2011), one study (Montenegro-Arana et al., 2016) had some concerns that may have introduced bias and one study presented low risk of bias (Ahrari et al., 2020). Concerns about introducing bias in the studies were due to inadequate sample calculation, unclear randomization and concealment and not sufficient description about blinding. In general, the evidence was judged low quality due to the inclusion of RCTs with great uncertainty and methodological issues.
Observations from the included reviews are presented in table 3. Two reviews (Consolaro et al., 2013; Márquez et al., 2013) considered TW during and after OT and one review (Freire et al., 2018) during OT. Regarding the time after bracket debonding in which TW can be applied, the authors recommend a 14-30-day period (Consolaro et al., 2013; Márquez et al., 2012). All three reviews (Consolaro et al., 2013; Márquez et al., 2012; Freire et al., 2018) did not recommend TW during conventional OT. The lack of diffusion of the whitening agent under the brackets which may result in non-uniform color changes and possible enamel cracks during debonding are variables to consider (Consolaro et al., 2013).
Discussion
General issues
Results from this systematic review were limited and meta-analysis was not attempted due to the nature of the data collected. In general, the clinical studies found were low quality with important methodological issues such as small-sample and no calculation of sample size. The inclusion of previous critical reviews offered some points of views based mainly on data from in vitro studies which need to be considered with caution when deciding about TW during or after OT. This narrative review synthesized the findings of quantitative studies which used diverse methodologies or with different conceptualizations to identify the appropriate moment to perform TW in conventional orthodontic patients. It is important to note that all studies that were assessed reported satisfactory improvements in color, independent of the protocol used and therefore will not be subjected to discussion.
Tooth whitening during orthodontic treatment
This systematic review found two studies from the same research group (Montenegro-Arana et al., 2016; Jadad et al., 2011) which performed TW during OT with satisfactory results in color shade. However, the evidence is low quality and there seems to be a lack of rationality for this procedure with no external validity. Color changes of the tooth around brackets is a possible outcome but there is the concern that applying TW procedures with brackets in place would produce a non-uniform color change. Two in vitro studies using bovine teeth demonstrated that the diffusion of the TW agent is impaired under the bracket resulting in significant difference in color between the center (area under bracket) and marginal areas of the tooth (Lunardi et al., 2014; De Melo Oliveira et al., 2021). In contrast, few case reports have obtained satisfactory results of TW used during clear aligner OT suggesting its feasibility with this technique in areas without bonded resin attachments (Oliverio et al., 2019; Sword and Haywood, 2020). Nonetheless, controlled clinical studies are necessary to recommend this last strategy. The decision of TW during conventional OT appears to be based on clinical preference rather than on an evidence-based approach. Therefore, it is not possible to recommend TW during OT.
Tooth whitening after orthodontic treatment
One of the main reasons for TW after OT is the development of white-spot lesions. However, the intervention that has shown moderate effectivity in treating these lesions is fluoride varnish application (Höchli et al., 2017). In addition, the available evidence from a recent systematic review found no support for TW for the management of whitespot lesions after OT (Gizani et al., 2020). On the other hand, extrinsic stains developed during OT can be successfully managed with TW strategies (Rodríguez-Martinez et al., 2019). But the question is: ¿what is the appropriate time in days in which tooth whitening can be performed after bracket debonding? Several aspects are discussed based on the available evidence.
Important changes in pulp tissues occur during OT depending on the magnitude of the force and the type of movement. Pulp vitality is affected with moderate to severe intrusion forces due to vascular congestión (Han et al., 2013). Other researchers found in clinical studies that pulp volume and pulp blood flow are significantly decreased with orthodontic forces (Venkatesh et al., 2014; Abu Alhaija et al., 2019). Pulp blood flow was found to return to baseline values after one month, suggesting that waiting this time would be advisable after bracket removal to perform TW (Abu Alhaija et al., 2019).
Debonding of brackets results in damage to the enamel, resin tags and increased sensitivity (Zaher et al., 2012; Dumbryte et al., 2017). A study found that sensitivity is higher immediately after bracket debonding and shows a decreased but still positive response after 7 days (Dumbryte et al., 2017). Dental hypersensitivity was a frequent finding in this systematic review. In addition, polishing of the tooth surface with burs and discs after bracket debonding may also affect the enamel quality and result in damage (Faria-Júnior et al., 2015; Vidor et al., 2015). A recent experimental study showed that a remineralization layer can be formed 14 days after debonding when a toothpaste containing calcium sodium phosphosilicate (CSPS) was applied daily (Triwardhani et al., 2019). Therefore, all these variables and possible consequences should be carefully assessed before deciding on performing TW after OT.
Periodontal changes are also associated with OT. Increased plaque accumulation and gingivitis is common in conventional orthodontic patients (Van Gastel et al., 2007). Oral hygiene during OT is a major factor which influence the periodontal condition and successful achievement of treatment objectives (Talic, 2011). Additionally, it has been reported that the levels of plaque, bleeding on probing and gingivitis are significantly reduced 30 days after bracket debonding accompanied by prophylaxis and oral hygiene instructions (Jadad et al., 2011; Sallum et al., 2004). Therefore, any TW procedure after OT would be best applied under proper oral hygiene and healthy periodontal conditions.
A final consideration is the concentration of the whitening agent. Tooth whitening agents, depending on the protocol used, must remained in contact with the tooth surface for extensive periods of time to produce its effects. Home whitening protocols used concentrations between 8-15% for 45 minutes to 1 hour. In contrast, in-office protocols used higher concentrations of the whitening agent (30-46%) for a short exposure time. It has been observed that patients overuse the at-home TW protocols that may result in important complications (Alqahtani et al., 2014). An in vitro study showed that higher concentrations of carbamide peroxide (>10%) caused a reduction in the enamel microhardness. Furthermore, after a post-whitening recovery period in artificial saliva, the microhardness improved but did not reach baseline values (Basting et al., 2003). This may indicate that the changes in the mineral composition and surface of the enamel produced by high concentration of whitening agents are permanent and therefore, could affect the previously altered tooth structure by the mechanical debonding of brackets.
Remineralization of the enamel is possible after orthodontic treatment and this phenomenon occurs naturally by saliva and with the use of fluorides or casein phosphopeptide-amorphous calcium phosphate products. Guzmán-Armstrong et al. (2010) reported that remineralization of white spot lesion is possible after bracket removal, but it depends on the severity of the lesions. Nonetheless, remineralization could take up to 6 months and therefore any treatment for white spot lesion or stains should be delayed until the enamel has recovered. Therefore, TW after bracket debonding should be carefully considered as remineralization of the enamel is occurring and whitening agents could induce further damage to the tooth surface. In all cases, TW after OT must be closely monitored by the clinician in order to control the desired tooth color change and possible adverse effects.
Since no consensus regarding the number of days after bracket debonding in which TW can be safely applied and based on the available data, it seems rational to wait at least 30 days to avoid complications and to allow for the enamel, pulp and periodontal tissues to recover after OT. However, there may be cases in which an extended waiting period is appropriate depending on the clinical appearance of extrinsic stains, white spot lesions and quality of the enamel.
Conclusions
Low quality evidence suggests that the appropriate moment to perform tooth whitening in conventional orthodontic patients is after brackets removal with a waiting period of at least 30 days. There is not adequate evidence to support tooth whitening during conventional orthodontic treatment.
Author contribution statement
All the authors declare that the final version of this paper was read and approved. The total contribution percentage for the conceptualization, preparation, and correction of this paper was as follows: S.H.V. 25%, M.F.N. 25%, J.E.B. 25% and F.A.R. 25%.
Data availability statement
The data supporting the results of this study is available as “supplementary files” on the Uniciencia website.
Ver anexo en PDF


















