Introduction
The mandibular canal is a bony structure located in the mandible that encloses the mandi- bular nerve; its origin is at the level of the mandibular foramen, and it generally ends in the mental foramen at the level of the second premolars (1). The architecture of this intraosseous canal and the location of the anatomic foramina is predetermined by the path of the branching of the blood vessels and the mandibular canal within the mandibular arch, which allows the innervation of the lower molars and premolars and the lower lip and chin to achieve correct functioning of the stomatognathic system (2,3). The morphological characteristics and the location of the mandibular canal may vary according to each individual person and ethnic group. The roots of the teeth at the mandibular level are located relatively close to this canal, meaning it could be damaged during dental treatments (4,5).
Dental procedures, such as endodontics, tooth extractions and dental implant placement, can damage the mandibular canal. Different symptoms, such as paresthesia, pain, hyperesthesia, hypoesthesia and numbness at the level of the lower lip and gums, have been reported in patients when irrigants and endodontic filling materials are extruded, as well as when overinstrumentation occurs (6,7,8,9,10). The incidence of neurosensory alterations of the mandibular nerve during endodontic treatment is 35% (6).
The mandibular nerve is the nerve that is most prone to damage in 68% of cases (11). Furthermore, 48% of patients presenting with facial paresthesias had previously undergone dental procedures that caused damage to the mandibular canal (12). Moreover, most cases of lesions of the mandibular nerve have been observed during treatment of the second molars. However, this can also occur in permanent mandibular first molars and premolars (13). Cone-beam computed tomography (CBCT) is used in different areas of dentistry to make a correct diagnosis and, therefore, to carry out successful treatment (14,15). Examinations performed by this type of tomography allows for accurate linear measurements to be obtained with very high precision and reliability (16). This image provides three-dimensional reconstructions of the maxillofacial structures in a precise, sensitive, and noninvasive way in comparison with conventional images, which have limitations such as overlapping, geometric distortion and errors in the localization of anatomical structures (17,18).
Investigations carried out in different populations indicate that the distances from the apices to the mandibular canal vary according to sex, age and race (17,19,20). At present, there are no studies in the Peruvian population where the distances from the apices to the mandibular canal have been evaluated. Therefore, it is necessary to evaluate the proximity between these anatomical structures to reduce the risk of injury during endodontic treatments and complex surgeries.
Therefore, the aim of this study was to compare the average distances from the apices of the roots of the second premolars, first molars and second molars to the mandibular canal in the Peruvian population according to sex using CBCT.
Materials and methods
A retrospective observational study was approved by the Institutional Ethics Committee of the Universidad Científica del Sur, Lima Perú with CIEI code 612-2020-POS8.
The study included CBCT scans of 80 patients (40 males and 40 females) obtained from the Instituto de Diagnóstico Maxilofacial in Lima, Perú, during the period 2015-2020. The CBCT scans were previously obtained for reasons not related to this investigation.
The sample size was calculated from a previous pilot study using the formula for estimating differences in means with a confidence level of 95% and a statistical power of 80%, considering a mean difference of 0.74mm and standard deviations of 2.65mm and 1.85mm, which were obtained by using the distances from the apices of the second premolars on the left side to the mandibular canal in males and females.
For four consecutive days, the researcher was trained by a maxillofacial radiologist with 6 years of experience in the manipulation of the DICOM storage program, as well as the relevant techniques and procedures, to obtain the images. In addition, the researcher's measurements from the apices of the evaluated teeth to the mandibu- lar canal were calibrated with those of a specialist consultant. This was done by intraand interexaminer calibration using 16 CBCT scans from the pilot study. The respective measurements were taken, and after five days, the 16 CBCT scans were reanalyzed; the specialist and the examiner evaluated the scans separately to determine the concordance and to ensure that the training was correct. The interclass correlation coefficient indicated a strong relationship with a value of 0.99 for intra and interexaminer calibration.
The inclusion criteria were Peruvian patients from 15 to 80 years of age with the presence of permanent monoradicular second premolars, first molars and second molars with their respective adjacent and antagonist teeth, and the following were considered as exclusion criteria: patients with developmental alterations or pathologies, dental/ skeletal malocclusion that could have altered the position of the studied teeth, endodontic treatment, and apical lesions of the teeth. All CBCT scans were performed by trained personnel using the same PROMAX 3D machine (Planmeca, Helsinki, Finland), ensuring the following parameters during the exposures: a kilovoltage of 85, 16 milliamperes, an exposure time of 14 seconds, a field size of 10x10, and a voxel of 200 microns. The images were exported in DICOM storage format; subsequently, the data were imported into Planmeca Romexis 5.3.3.5 software (Planmeca, Helsinki, Finland) to calculate the distances in millimeters.
Distance assessment
The lower occlusal plane was leveled to the floor in the cross-section, and the panoramic reformation was performed using the ''Manual panoramic''tool. Points were then placed following the path of the mandibular canal using the ''Draw Nerve''tool. The position of the mandibular canal and the apices was assessed in the oblique sagittal view, with an interval of 1mm (Figure 1). The vertical distance from the upper edge of this canal (POINT A) to the apex of the mesial roots of the first molars and second molars (POINT B) was measured in oblique sagittal sections, as well as the distance from the roots of the second premo- lars that presented a single root in the right and left hemiarch in men and women, using Planmeca Romexis5.3.3.3 software (Figure 2) (21). The data were entered into a data collection form, where each tomography measurement was recorded by means of codes, with the following recorded: sex, age, hemiarch, and the vertical distance of each root apex of the first molars, second molars, and second premolars. Planmeca Romexis5.3.3.5 software and iMac MXWT2LL/A (Apple brand with an Intel Core i5-6700K processor with 8 GB of RAM memory and 256 GB of SSD) were used to perform the respective measurements.
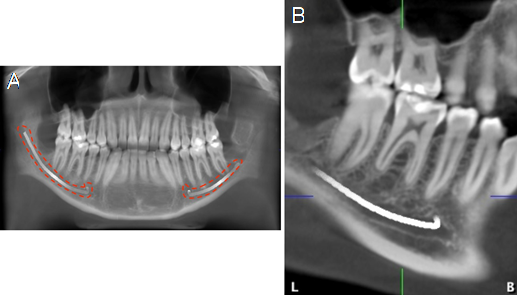
Figure 1 Location of the mandibular canal in CBCT. (A) Panoramic thin-section image showing the mandibular canal (B) Oblique sagital section showing the path of the mandibular dental canal on the right side and its relationship to the apex of the mesial roots of the first and second molars; as well as the second premolar.
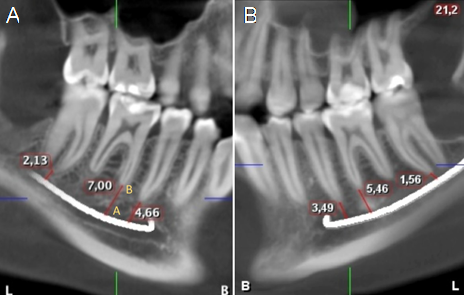
Figure 2 Vertical linear measurements of the distances from the mandibular nerve to the apex of the roots of the posterior teeth on CBCT. (A) Oblique sagittal section showing the vertical measurements from the upper edge of the mandibular canal (POINT A) to the apex of the mesial roots of the first and second molars (POINT B); as well as the distance from the roots of the second premolar on the right side, (B) measurements made in the left hemiarch.
Statistical analysisS
IBM SPSS Statistics v25.0 (IBM, Chicago, USA) was used for statistical processing of the data. Univariate analysis was carried out using descriptive statistics to show the distance values. Bivariate analysis was carried out using inferential statistics by way of Student's t test (paired and unpaired). A p≤0.05 was considered significant.
Results
In the present study, the distances from the apices of the mesial roots of the molars and second premolars to the mandibular canal were evaluated in 80 patients using CBCT. Table 1 shows the average distance by sex according to hemiarchs; in the right hemiarch, the second molars presented a mean of 3.99mm in men and 2.87mm in women, with a significant difference (p<0.05). Regarding the first molars and second premolars of the right hemiarch, it was observed that males presented higher average distances; however, no statistically significant differences were found. In addition, when evaluating the left hemiarch between males and females, none of the distances showed statistically significant differences (p>0.05), although the results showed a higher average distance in males (Table 1).
In the general population, Table 2 shows that no significant difference (p>0.05) was found in the distance from the root apices of the second premolars, first molars and second molars to the mandibular canal when compared bilaterally. However, in the second premolars and second molars of the left hemiarch, the values were higher, with averages of 5.52mm and 3.75mm, respectively (Table 2).
Table 3 shows that the average distances from the second molars to the mandibular canal in females presented a statistically significant difference when compared bilaterally, resulting in averages of 2.87mm for the right hemiarch and 3.76mm for the left hemiarch (p<0.05). With respect to males, there was a statistically significant difference (p>0.05) between the right and left hemiarch of the first molar, with values of 6.05 mm and 5.29mm, respectively (Table 3).
Table 1 Comparison of vertical distances from the mandibular canal to the root apices of the second premolar, first molar, and second molar in males and females.
| Variables | Males (n=40) | - | Females (n=40) | - | T | p |
|---|---|---|---|---|---|---|
| - | Mean | SD | Mean | SD | - | - |
| Right side | - | - | - | - | - | - |
| Second premolar | 5.46 | 2.64 | 4.97 | 1.92 | 0.96 | 0.34 |
| First molar | 6.05 | 2.65 | 5.40 | 2.06 | 1.23 | 0.22 |
| Second molar | 3.99 | 2.85 | 2.87 | 1.78 | 2.12 | 0.04 |
| Left side | - | - | - | - | - | - |
| Second premolar | 5.76 | 2.50 | 5.28 | 1.89 | 0.96 | 0.34 |
Unpaired t-test.
p<0.05 SD=Standard deviation.
Table 2 Comparison of vertical distances from the mandibular canal to the root apices of second premolar, first molar, and second molar in the population.
| Variables | Sides | Mean | SD | Mean difference | SD difference | Paired t-test | p |
|---|---|---|---|---|---|---|---|
| Second premolar | Right | 5.22 | 2.31 | -0.31 | 1.90 | - | - |
| - | Left | 5.52 | 2.22 | - | - | - | - |
| First molar | Right | 5.72 | 2.38 | 0.27 | 1.84 | 1.30 | 0.20 |
| - | Left | 5.46 | 2.20 | - | - | - | - |
| Second molar | Right | 3.43 | 2.43 | -0.32 | 2.20 | -1.31 | 0.19 |
| - | Left | 3.75 | 2.48 | - | - | - | - |
Paired t-test.
p<0.05 SD=Standard deviation.
Table 3 Bilateral comparison of vertical distances from the mandibular canal to the root apices of the second premolar, first molar, and second molar in males and females.
| Variables | Sides | Mean | SD | Mean difference | SD difference | Paired t-test | p |
|---|---|---|---|---|---|---|---|
| Females | - | - | - | - | - | - | - |
| Second premolar | Right | 4.97 | 1.92 | -0.31 | 1.95 | -1.02 | 0.32 |
| - | Left | 5.28 | 1.89 | - | - | - | - |
| First molar | Right | 5.40 | 2.06 | -0.23 | 1.63 | -0.88 | 0.38 |
| - | Left | 5.62 | 1.62 | - | - | - | - |
| Second molar | Right | 2.87 | 1.78 | -0.90 | 2.12 | -2.69 | 0.01 |
| - | Left | 3.76 | 2.27 | - | - | - | - |
| Males | - | - | - | - | - | - | - |
| Second premolar | Right | 5.46 | 2.64 | -0.30 | 1.88 | -1.00 | 0.33 |
| - | Left | 5.76 | 2.50 | - | - | - | - |
| First molar | Right | 6.05 | 2.65 | 0.76 | 1.92 | 2.50 | 0.02 |
| - | Left | 5.29 | 2.66 | - | - | - | - |
| Second molar | Right | 3.99 | 2.85 | 0.25 | 2.16 | 0.74 | 0.47 |
| - | Left | 3.74 | 2.69 | - | - | - | - |
Paired t-test.
p<0.05 SD=Standard deviation.
Discussion
The mandibular canal contains blood vessels and the mandibular nerve, which is prone to damage in 68% of cases due to different dental treatments, such as endodontics, tooth extractions and dental implant placement. This can generate symptoms such as pain, hypoesthesia and numbness, among others, in patients (2,4,5). Injury to the mandibular nerve can be caused by inadequate identification of its location in panoramic radiographs where a diminished appearance of the mandibular canal is observed (22). However, the use of CBCT has led to a reduction in the risk of injury to the mandibular canal (23).
The incidence of neurosensory disorders of the mandibular nerve caused by endodontic treatments is 35% (6). Some of the risk factors that can involve damage to the mandibular nerve are the experience of the dentist, the age and sex of the patient and, most commonly, the anatomical relationship between the posterior tooth apices and the mandibular canal (24). The extrusion of endodontic material beyond the apex can cause damage to the mandibular nerve due to the proximity of the mandibular premolar and permanent mandibular molar apices when perforating the mandibular canal. In the event of overextension of obturating material or irrigation products, the vacuoles facilitate the diffusion of these products into the vasculonervous bundle that runs through the low-density cancellous bone (9,25). Worldwide, the number of root canals performed annually is considerable; therefore, it is essential to understand the procedures that can prevent nerve complications as much as possible. Thus, it is recommended that a complete preoperative radiographic examination is performed, which includes the use of CBCT (9). By using this diagnostic tool, it is possible to ascertain the three-dimensional position in which the mandibular canal is located with respect to the root apices of the posterior teeth, taking into consideration the variables that may influence the distance. This tool is considered the gold standard for judging this relationship due to its high precision and sensitivity, which allows for accurate linear measurements to be obtained with a high level of reliability (14,15,16,17,18,26).
The scientific literature includes several studies where the proximity from the apical molars and premolars to the mandibular canal has been evaluated, from which it is evident that the results may vary according to the population type, as well as the age and sex of the people. For this reason, the aim of the present study was to evaluate, according to sex, the average distances from the root apices of the second premolars and first and second molars to the mandibular dental canal with CBCT in a sample of Peruvian patients. This study showed that men presented greater distances from the apices of the posterior teeth to the mandibular canal. These results are similar to those in studies carried out in the Indian popula- tion, where the second premolars and first and second molars presented a significantly shorter distance in women (19).
In relation to the anatomical characteristics, similarities with previous studies were found (4,20,26,27); in the present study, it was observed that the apices of the second molar roots were closest to the mandibular canal in both men and women. In addition, when compared according to sex and hemiarch, men presented greater distances than women in the second molars on the right side, with a significant difference (p<0.05). This could be explained by the fact that women generally have a smaller body size, so they could be at greater risk of suffering damage to the mandibular canal. Females have a 3.29 times higher risk of mandibular canal injury than men during the placement of dental implants. Risk factors of mandibular canal injury include menopause and subsequent changes to bone metabolism; furthermore, osteo- porosis is related to residual ridge atrophy and lower bone mass (22). On the other hand, it was observed that there was an increase in the distances from the mesial apex of the second molars to the mesial root of the first molars, tapering to the level of the second premolars in females.
Anatomically, the mandibular canal develops in the mandibular process during the fifth week after conception, before there is histological evidence of tooth development (28). This study demonstrated that bilaterally posterior teeth present different distance values. A possible explanation is that the position of the mandibular canal varies during the human functional progression from sucking to chewing. Masticatory muscle activity stimulates bone growth and buccal cortical bone growth, causing the mandibular canal to move more lingually. In addition, the position of the mandibular canal varies according to age, sex and race (29,30). While some studies indicate that the location of the mandibular canal tends to be bilaterally similar if the mandibular shape is symmetrical in individuals without mandibular molar eruptive disorders, the research by Ahmed et al. (31) states that bilateral images show lateral asymmetry in the position of the mental foramen in 40% of patients. In addition, as a result of attrition and dental wear, there is a continuous eruption of the teeth (32). Schierz et al. indicated that occlusal wear increases with age and is greater in men than in women (33). Likewise, it is necessary to compare the distances bilaterally according to sex, since in the dentate population, there is a unilateral prefe- rence for the chewing side, and this is associated with the lateral asymmetry of the bite force and the occlusal contact area shown on CBCT scans, which could cause the distances from the apices of the roots to the mandibular canal to vary (34).
In recent years, research has been carried out on the different positions of the mandibular canal and the mental and mandibular foramens in adults and their relationship to sexual dimorphism, and these possible differences could potentially be used to determine the identity of human remains (35). Simonton et al. (32) indicate that the distance generally increases up to a certain age and then begins to decrease. This maximum peak in the increase in the distance from the mandibular nerve to the apices of the roots is seen in men up to 50 years of age and in women up to 40 years of age, after which a decrease is observed in the distances. The explanation for the above is related to continuous growth in women up to 40 years of age and in men up to 50 years of age (32). However, these findings and their use in the forensic area must be considered with caution, since studies such as that by Angel et al. (36) indicate that the relative location of the canal and the foramina remains fairly constant among sexes and with increasing age, which is why they mention that the values of the distances obtained are unlikely to be used as forensic determinants.
One of the limitations of this research was the difficulty in finding a database with the inclu- sion criteria established for the sample. Most of the scans of patients who met the requirements for the study were within an age range of 15 to 30 years, since most patients had partial edentulism. It is recommended that future research compare the distances from the mandibular canal to the apices of the posterior teeth according to various age ranges and in different populations.
Conclusions
The apices of the second molars were the closest to the mandibular canal. In addition, women presented shorter distances from the apices to the mandibular canal than men. The authors recommend further investigation of this feature for its potential use in forensic science.
Author contribution statement
Conceptualization and design: P.M., A.A and M.G.
Literature review: P.M.
Methodology and validation: M.G and A.A.
Formal analysis: P.M. and M.G.
Investigation and data collection: P.M.
Resources: P.M. and M.G.
Data analysis and interpretation: P.M., A.A. and M.G.
Writing-review and editing: P.M. and M.G.
Supervision: M.G and A.A.
Project administration: P.M.
All authors have read and agreed to the published version of the manuscript.















