Introduction
Oral squamous cell carcinoma (OSCC) represents 90% of all malignant neoplasms of the oral cavity (1,2). The etiology of OSCC is multifactorial (3,4) and its clinical presentation is variable (5).
Potentially malignant disorders (PMDs) are a heterogeneous group of mucosal lesions associated with an increased risk of malignant transformation (6). The rate of malignant transformation of PMDs to OSCC varies depending on the population, their habits, and the site of the lesion (7,8). Moreover, leukoplakia is the most common PMD with a rate of progression to invasive oral cancer in up to 36% (9).
Biopsy remains the gold standard for the diagnosis of OSCC (10,11). The presence of epithelial dysplasia is still considered the strongest predictor of future malignant transformation (12).
The carcinogenic process requires multiple molecular events for the transformation of a normal cell into a cancer cell (13). Tumorigenesis begins long before the growth of a clinically detectable lesion. Field cancerization is the replacement of the normal cell population by a population of cells primed for cancer development (14).
Aldehyde dehydrogenase-1 (ALDH1) promote the intracellular oxidation of aldehydes in the initial stages of stem cell differentiation, and, previously was linked to treatment resistance and poor prognosis for OSCC (15). CD44 acts in cell aggregation, proliferation and migration, and is a common marker for highly tumorigenic cancer stem cells (CSC) in head and neck squamous cell carcinomas (16). Studies suggest that CSC present in OSCC and other types of tumors exhibited resistance to chemotherapy and radiotherapy, and could be involved in the establishment of metastases (15,17).
Fibroblast growth factor two (FGF-2) is one of the prototypes of a large family of growth factors that play a role in collagen synthesis and angiogenesis (18). Studies showed overexpression of the FGF receptor family, mainly FGFR-2, in high-grade malignant tumors and malignant transformation of normal cells (19).
Apoptosis-related disorders can promote the development of cancer (20). Caspase-3 inhibition and downregulation have been implicated in the formation and progression of cancer cells (21).
The stromal microenvironment is a key regulator of self-renewal in the epithelium, and such aberrant changes in the stroma may allow field cancerization of the tissue (22). CSCs are found in the invasive fronts of head and neck squamous cell carcinomas close to blood vessels, at the perivascular niche (23).
Signaling events initiated by endothelial cells during angiogenesis are critical for the survival and self-renewal of these stem cells (23). Thus, this study aimed to analyze the expression and spatial distribution of ALDH1A1, FGFR2, caspase- 3, and CD44 in OSCC and leukoplakia with and without oral mucosal dysplasia. The principal null hypothesis was: (i) there is no correlation between the immunoexpression of these markers and tumor malignancy.
Materials and methods
The research protocol was approved by the Ethics Committee of Universidad de Costa Rica (UCR) (B9300, VR-467-2018).
Fifteen (#15) archived formalin-fixed, paraffin-embedded samples of OSCC (n=5), leuko- plakia with (n=5) and without (n=5) dysplasia obtained by incisional biopsies, were retrospectively chosen from the archives of the Faculty of Dentistry of the UCR.
Immunohistochemical analyses
All samples were processed using conventional histochemical techniques, embedded in paraffin, sectioned at 2-μm thickness, mounted on glass slides, and deparaffinized. The samples were subdivided according to the following primary antibodies and respective dilution ratios (n=5): rabbit polyclonal anti-FGFR2 (1:30 Sigma Prestige Antibodies, St. Louis, MO, USA), rabbit polyclonal anti-ALDH1A1 (1:1000 Sigma Prestige Antibodies, St. Louis, MO, USA), rabbit polyclonal anti-CD44 (1:4000 Sigma Prestige Antibodies, St. Louis, MO, USA), and rabbit polyclonal anti-Caspase-3 (1:500 Cell Signaling Technology, Danvers, MA, USA). Proteinase K (Dako Cytomation, Carpinteria, CA, USA) incubation was performed for antigen retrieval, following the manufacturer's instructions. Nonspecific binding was blocked by incubating sections for 1 h with goat normal serum diluted in PBS. After overnight incubation at 4-C with primary antibodies, the slides were washed with PBS and incubated with the conjugated secondary antibody SignalStain Boost detection reagent (Cell Signaling Technology, Danvers, MA, USA) in a humidified chamber for 30 min at room temperature. Samples were washed, and visuali- zation was completed using the SignalStain DAB Substrate kit (Cell Signaling Technology, Danvers, MA, USA) and counterstaining lightly with Mayer hematoxylin solution.
Images of the immunohistochemically stained tissue sections were acquired using a light microscope (Nikon, Eclipse Ti-5; Minato, Tokyo, Japan). Five images per sample were captured at 20× magnification. Two calibrated investigators analyzed the intensity of the immunostaining of each marker under 20X magnification according to the following criteria:
(0): None (absent cell immunolabeling).
(1): Light (isolated cell immunolabeling).
(2):Moderate (cell immunolabeling detected in specific or focal areas on the tissue).
(3):Intense (strong immunolabeling with a uniform spatial distribution on the tissue).
Results
The statistical analysis of the data demonstrated a significant difference in the immunoex- pression of all immunomarkers between OSCC and leukoplasia without dysplasia (Figure 1).
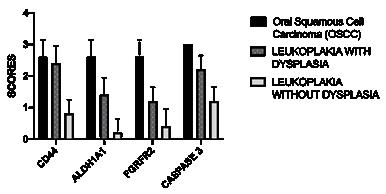
Figure 1 Immunoexpression and statistical analysis of the cell markers in OSCC and in leukoplakia with or without dysplasia. Each bar represents the mean ± standard error of the mean. p < 0.05 represents statistical difference.
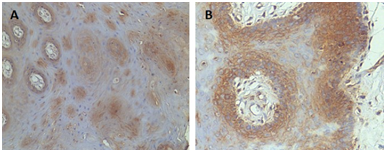
CD44 immunoreactivity was diffusely evident in the non-neoplastic squamous epithelium (Figure 2.A, Figure 3.A). Strong intensity membranous immunostaining for CD44 in epithelial dysplasia and high-rate CD44 positive cells in tumor tissue, in perivascular niche and the inflammatory infiltrate was observed (Figure 2.B-C, Figure 3.B-D). No positive staining for ALDH1A1 was noted in the non-neoplastic squamous epithelium (Figure 2.D, Figure 4). Mild positive expression of ALDH1A1 were observed in specimens with epithelial dysplasia. Moreover, positive ALDH1A1 was noted in budding area, and in tumor nests (Figure 2.E-F, Figure 4). Minimum positive FGFR2 staining was observed in the non-neoplastic squamous epithelium (Figure 2.G, Figure 5). However, mild positive expression of FGFR2 was detected in epithelium with dysplasia, and a high rate of FGFR2 positive cells in tumor tissue and inflammatory infiltrate (Figure 2.H-I, Figure 5). Immunohistochemical mild positive staining of caspase-3 was noted in the non-neoplastic squamous epithelium (Figure 2.J, Figure 6). In epithelial dysplasia, caspase-3 was localized in the proliferative foci of parabasal cells of the epithelium. At the invasive carcinoma, extensive positive caspase-3 staining was observed in carcinoma cells (Figure 2.K-L, Figure 6). In-situ carcinoma caspase-3 immunostaining was observed centrally within the cell nests, and surrounding capillaries, arteries and blood vessels (Figure 6).
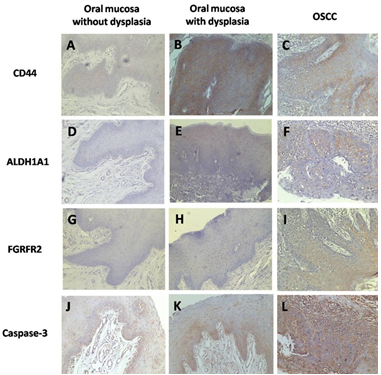
Figure 2 Representative images of CD44, ALDH1A1, FGFR2 and caspase-3 immunohistochemical analysis in OSCC, dysplastic mucosa and in oral mucosa without dysplasia (20X).
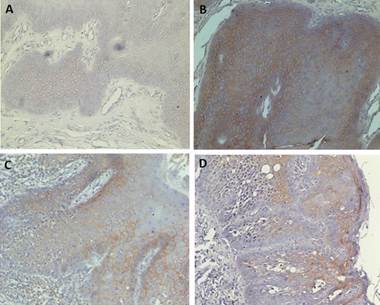
Figure 3 A. CD44 immunoreactivity was diffusely evident in non-neoplastic squamous epithelium (20X). B. Strong intensity membranous immunostaining for CD44 in epithelial dysplasia (20X). C-D Upregulation of CD44 positive cells in tumor tissue and inflammatory infiltrate (20-40X).
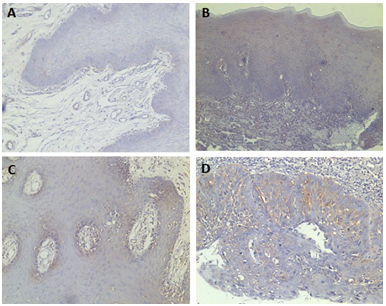
Figure 4 A. Minimum immunostaining for ALDH1A1 was observed in non-neoplastic squamous epithelium (20X). B. Mild positive expression of ALDH1A1 in a specimen with epithelial dysplasia (20X). C. Positive ALDH1A1 in budding area (20X). D. Immunostaining of ALDH1A1 in cell groups, tumor nests (40X).
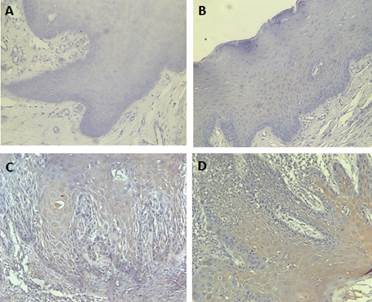
Figure 5 A. Minimum FGFR2 immunostaining was observed in non-neoplastic squamous epithelium. B. Very mild positive expression of FGFR2 in epithelium with dysplasia. C-D High rate of FGFR2 positive cells in tumor tissue and inflammatory infiltrate (20-40X).
Discussion
This study analyzed the expression and spatial distribution of ALDH1A1, FGFR2, caspase- 3, and CD44 in OSCC and leukoplakia with and without oral mucosal dysplasia. Summarizing, all immunomarkers were upregulated in OSCC and leukoplakia with oral mucosa dysplasia, leading to the rejection of the principal null hypothesis.
Oral carcinoma is the fourth most common region of cancer incidence and the second most common region for cancer-related mortality world- wide (24). Studies showed that tumor mass has heterogeneous cell content. A subpopulation of cells with self-renewal potential, high proliferative capacity, differentiation ability, resistance to therapy, and tissue invasion were named cancer stem cells (CSC) (15,22,24)
CD44 and ALDH1A1 are common markers for CSCs in OSCC (24,25). Our study showed that CD44 and ALDH1A1 immunoreactivity was diffusely evident in the non-neoplastic squamous epithelium. However, strong intensity membranous immunostaining for both CSCs markers was demonstrated in epithelial dysplasia. Upregula- tion of CD44 positive cells in tumor tissue and inflammatory infiltrate was denoted in OSCC, and ALDH1A1 was evident in the budding area. Moreover, we observed that in the region with differentiated cells, CD44 was weak or almost absent. Mascolo et al. (2012) (26) demonstrated that 54% of the head and neck carcinomas showed high expression of CD44, of which 33% reported recurrence, metastasis, and death. Moreover, ALDH1A1 and CD44 expression did not showed a pattern of distinct spatial distribution, except in OSCC that was noted at the budding area and in the inflammatory infiltrate. ALDH1A1 is predominantly found in aggressive tumors and demonstrated correlation with metastases, lymph nodes, and high tumor stage (27), being important as a prognostic marker for worse survival rates (24).
FGFR2 plays an important role in collagen synthesis and angiogenesis in several cancers (28). Our data revealed minimum, almost imperceptible FGFR2 expression in leukoplakia with no dysplasia. The upregulation of this marker expression was cytoplasmatic and more observed in basal and parabasal layers of oral mucosa with dyspla- sia and was evident in OSCC tumor cells and in the tumor stroma. Previous studies also demonstrated FGFR2 expression in cancer and precancer (28,29), the staining intensity increased at all levels of dysplasia and was more intense in carcinomas, in accordance with our data.
FGFR2 signaling due to their overexpression can lead to the protection of apoptosis which is one of the hallmarks of cancers (28,30). Caspase-3 is a member of a family of cysteine proteases and is a key enzyme in apoptosis (31). Studies related apoptosis markers downregulation in cancer (31,32,33). The opposite tendency was observed in our study. We observed that with the transition from no dysplasia to oral mucosa with dysplasia to OSCC, Caspase-3 intensity increased. Paradoxically, current evidence reported upregulation of procaspase-3 and caspase-3 in a variety of cancer types (34,35). Overexpression of a pro-apoptotic protein in cancer has been a matter of research. Recently was suggested that caspase-3 activity promotes oncogenic transformation (35).
Our data suggested that the presence of dysplasia is a significant clinic-pathologic predictor for malignant transformation in precancer, in accordance with previous studies (28,32,34). Moreover, we observed a statistical difference in the marker's expression between OSCC and leukoplakia without oral mucosa dysplasia, being more significant for ALDH1A1 and FGFR2. Our results can be useful for evaluating progression and malignant transformation to improve early diagnosis and treatment. However, our study presented a strong limitation regarding the number of samples validated, thus it was performed as a pilot study. Further studies must be done in a large cohort to sustain further conclusions.
Conclusion
Within the limitations of this pilot study, ALDH1A1, FGFR2, Caspase-3, and CD44 appear to be upregulated in OSCC and leukoplakia with oral mucosa dysplasia, suggesting to be impor- tant cell markers to evaluate carcinogenesis and tumor progression.
Author contribution statement
Conceptualization: J.R.-C. Methodology: Y.B.O., J.R.-C.
Validation: Y.B.O., J.R.-C..
Formal analysis: Y.B.O., J.R.-C.
Investigation: Y.B.O., J.R.-C.
Resources: Y.B.O., J.R.-C.
Data curation: Y.B.O., J.R.-C.
Writing-original draft preparation: Y.B.O., J.R.-C.
Writing-review and editing: Y.B.O., J.R.-C.
Visualization: Y.B.O., J.R.-C.
Project administration: J.R.-C.
Funding Acquisition: J.R.-C.
All authors have read and agreed to the published version of the manuscript.