Introduction
Miniscrews are devices commonly used in orthodontic treatments as an alternative to temporary anchorage that allows to improve the direction of the applied forces and, in some cases, to reduce treatment time. Being the extraalveolar miniscrews on which a greater amount of force is applied, which allows a wide versatility of dental movements for the correction of severe malocclusions without the need for extractions or orthognathic surgery, in this conservative way a complete retraction of the jaw dental arch can be achieved (1,2). A success factor for its placement is achieving adequate primary stability through mechanical retention resulting from the interaction between the surface of the miniscrew and the surrounding bone (3,4).
Recently, the Mandibular Buccal Shelf (MBS) has been proposed as an insertion site for extra- alveolar miniscrews (5,6). It is located bilaterally towards the buccal aspect of the roots of the first and second molars and anterior to the external oblique line of the mandibular ramus, providing adequate quantity and quality of bone (7). However, there is controversy in studies about the exact placement site in its structure due to local anato- mical variations and its characteristics in terms of cortical thickness and bone height (1,6,8,9).
Since its introduction in 1998, cone beam computed tomography (CBCT) has been increasingly used in orthodontics. Being the main advantage over conventional radiographs that anatomical structures can be evaluated in three-dimensional (3D) images (10), however, its use must be justified to reduce exposure to ionizing radiation of patients and should only be indicated when routine examinations do not provide sufficient elements for diagnosis and treatment planning (11,12). Although no studies indicate that CBCT is necessary for miniscrews placement, it is very useful to visualize anatomical structures near the insertion sites such as dental roots, mental foramen or the inferior alveolar nerve canal, as well as to evaluate bone characteristics in terms of quantity and quality of cortical and medullary bone (10).
Several studies on CBCT have found that the different sagittal and vertical growth patterns can influence the anatomy of certain structures, including the mandibular symphysis, the mandibular bone plate, and the cortical and alveolar bone (13,14,15). Growth variations in anatomical structures can determine a thicker or thinner cortical bone type (16), which would influence the insertion of extraalveolar miniscrews and their stability during orthodontic treatment (4).
The purpose of this research was the tomographic evaluation of the mandibular bone plate in patients with different vertical growth patterns of the Orthodontic Service of the Teaching Dental Center of the Universidad Peruana Cayetano Heredia (CDD-UPCH) in Lima.
Materials and Methods
The present study was approved by the Institutional Ethics Committee of the Universidad Peruana Cayetano Heredia with registration code 207035, likewise, the confidentiality of the data obtained was kept via enconding scans by a consecutive random number. The design was observational, descriptive, cross-sectional, and retros- pective; the study population was the CBCT of the patient file of the CDD-UPCH Orthodontic Service who attended the CDD-UPCH Radiology Service during the period 2015 to 2019. The sample size was calculated using the formula for estimating a mean with a population size of 267 confidence level of 95%, precision of 6 and variance of 96 considering the standard deviation obtained by Escobar-Correa et al. (14) determining a size of 10 for each vertical pattern group: hypodivergent, normodivergent and hyperdivergent, making a total of 30 orthodontic patients evaluated.
The criteria for the selection of the sample were CBCT exams in which the patient's skull is centered within the field of wiew, patients between 14 and 40 years old, who presented both first and second mandibular molars. Likewise, the exclusion criteria were the CBCT of patients who presented lower orthodontic appliances or extensive coronal restorations in the first and/or second molar, moderate to severe alveolar resorption, signs of facial trauma or previous orthognathic surgical treatment, pathologies near the area of interest or dental malposition of the first and/or second molar causing cross or scissor bite.
To select which CBCT would be evaluated in the study, a database was created with all those who met the selection criteria, a total of 37, who were measured by the facial height index (FHI) according to analysis of Jarabak (17) to determine their type of vertical growth, later by a simple random raffle with the Microsoft Excel program, the 3 groups of 10 participants were completed in order of appearance according to their respective type of growth, the remaining 7 CBCT were not considered for the research sample.
Then, the researcher who performed all the measurements, who is a Specialist in Orthodontics and Maxillary Orthopedics, was trained in the use of the software with a Specialist in the area of Oral and Maxillofacial Radiology of the UPCH with more than 10 years of experience, performed calibrations with 3 CBCTs (2 hypodivergent and 1 normodivergent) that met the selection criteria but were not chosen in the study. Inter-observer calibration with a specialist, and intra-observer calibration at 2 different times 5 days apart was made. The intraclass correlation coefficients (ICC) obtained were 0.991 and 0.998, respectively, indicating a very high concordance. The training and calibration was carried out in order to obtain an efficient methodology, as well as validity, reliability and reproducibility in the results.
All the selected CBCTs were taken with the Carestream Health Inc. (Rochester, NY, USA) tomograph, they were visualized and evaluated with the software CS 3D Imaging v3.8.7 on the computer of the CDD-UPCH Radiology Service (LENOVO brand with Intel Xeon processor with 14GB of. RAM memory, Windows 7 operating system and 22-inch LCD monitor with 1680 x 1050 resolution and 60 Hz).
Determination of the vertical skeletal pattern
To define the vertical skeletal pattern, the following method was used: in the tomographic volume, the orthogonal slice type was used in the sagittal plane with a slice thickness of 168.3mm in average intensity projection (AVG) integration mode to obtain a lateral cephalometric image of the entire skull and the software tools were used to adjust the contrast and brightness for better visualization enabling the location of 4 cephalometric points that the Jarabak analysis requires (17,18).
The Mentonian point (Me), the lowest point of the mandibular symphysis, was located, then 2 lines were drawn for the location of the Gonion point (Go), which is the intersection of the tangent to the posterior border of the ramus and the tangent to the inferior border of the mandibular body. Later, the Sella point (S), the geometric center of the turkish sella, and the Nasion point (N), the anterior limit of the frontonasal suture, were located, for which it was necessary in some cases to temporarily reduce the thickness of the cut.
Finally, posterior facial height (S-Go) and anterior facial height (N-Me) measurements were made, their proportion was determined and multiplied by 100% to obtain the facial height index (FHI) (17,18) (Figure 1).
The values of the pattern of the vertical growth pattern were classified according to the following values: Hypodivergent FHI ((≥64%), Normodivergent DV FHI (59-63%), Hyperdivergent FHI (≤58%) (17,18).
Visualization of mandibular buccal shelf (MBS)
The following method was applied to obtain the appropriate visualization sections of the MBS for the evaluation of bone characteristics:
The axial plane curved cut was used with the dental arch creation tool based on the mandibular teeth passing through the center of the crowns to obtain a panoramic reformation view, which was standardized in AVG integration mode and in a thickness of 20.1mm cut enough to include the mandibular width.
In the panoramic reformation, the cursor was moved and rotated in such a way that it was positioned in the longitudinal axis of the root of the reference tooth, in this way a dynamic transaxial view was generated which was evaluated in AVG mode and bone thickness. 2.1mm cut where measurements were made (Figure 2).
Measurement
For the analysis, four areas of frequent insertion of extraalveolar miniscrews in the MBS were selected, taking as reference: the mesial root of the first molar, distal root of the first molar, mesial root of the second molar and distal root of the second molar.
The measurements made by Escobar-Correa et al. (14) in each area and in both hemiarches as described below:
Angulation: it was measured as the internal angle formed by the axial axis of the molar and a tangent to the outermost surface of the MBS (Figure 3.A).
Height: cortical and medullary buccal bone was measured by drawing two horizontal reference lines from the cement-enamel junction (CEJ), one at 4mm and the other at 6mm parallel to the Y axis. From these, two lines were drawn vertical to the outermost part of the mandibular bone table (Figure 3.B).
Thickness: cortical and medullary buccal bone was measured by drawing two vertical reference lines from CEJ, one at 6mm and the other at 11mm parallel to the X-axis. From these, two horizontal lines were drawn towards the outer- most part of the cortical (Figure 3.C).
The values obtained were recorded in the data collection sheets. To carry out the measurements, the researcher complied with the recommendations of García et al. (19) on ergonomics in the radiology workplace, which are: Use glasses after a long time in front of the monitor, carry out a periodic optical review, use artificial tears to relieve dry eye symptoms, rest your eyes and posture by moving 20 steps away from the screen every 20 minutes for 20 to 30 seconds, avoid high temperatures and dry air, and maintain a proper body posture. All of these principles contributed to increased producti- vity and reduced fatigue for the radiologist, increasing work efficiency and effectiveness.
Additionally, viewing sessions were in the mornings with a 15-minute viewing break for every 2 hours of work on the computer. Each evaluation was carried out in a programmed time of 20 minutes maximum and a pause of a few seconds was taken between each evaluation, fixing the gaze on a distant point to restore and relax the accommodation system and thus prevent strabismus and visual fatigue (20).
Statistic analysis
Data were subjected to statistical analysis with SPSS 25 software. Descriptive statistics were reported through mean and standard deviation.
Differences between the groups of growth pattern according to sex were evaluated with the Chi square test. The distribution of normality was evaluated using the Kolmogorov-Smirnov test. To evaluate the bone characteristics of the MBS according to the vertical growth pattern and the characteristics of the MBS according to the reference root, the ANOVA test was used; when differences were found, the Tukey post-hoc test was performed.
To compare the features of the MBS according to sex and the features according to hemiarch, the Student's t-test was used. The significance level for all tests was set at P<0.05.
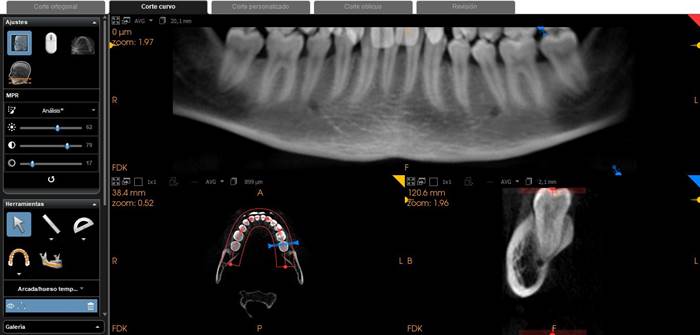
Figure 2 Visualization of the mandibular bone shelf (MBS). In the curved section mode and in the axial plane with the arch creation tool (red horseshoe), a panoramic reformation view was obtained, which was evaluated in AVG mode and 20.1mm section in the same way as the frontal plane in AVG and 2.1mm in a file image of the CDD-UPCH Radiology Service.
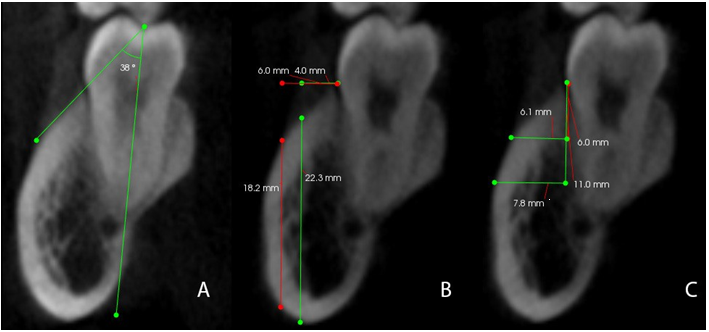
Figure 3 MBS measurement scheme in CBCT. A. Angulation: internal angle formed by the axial axis of the molar and a tangent to the outermost surface of the MBS. B. Height: measured by two vertical lines drawn towards the lowest part of the cortex, from two horizontal reference lines from the cement-enamel junction (CEJ), one at 4mm and the other at 6mm parallel to the Y axis. C. Thickness: measured using two horizontal lines drawn towards the outermost part of the cortex, from two vertical reference lines of the CEJ, one at 6mm and the other at 11mm parallel to the X axis n a file image of the CDD-UPCH Radiology Service.
Results
When comparing the features of the MBS: angulation, height at 4mm and 6mm, thickness at 6mm and 11mm; according to the vertical growth pattern: hypodivergent, normodivergent and hyperdivergent, it was found that there were no statistically significant differences (p<0.05) when applying the ANOVA test (Table 1).
When the features of the MBS were compared according to male and female sex, it was found that there were no statistically significant differences (p<0.05) when applying the Student's t-test (Table 2).
When comparing the angulation, height at 4mm and 6mm, thickness at 6mm and 11mm of the mandibular bone plate according to the left and right hermiarch, it was found that there were no statistically significant differences (p<0.05) when applying the Student's t-test (Table 3).
When the features of the MBS were compared according to the reference root, it was found that there were significant statistical differences (p<0.05) when applying the ANOVA test.
The distal root of the mandibular second molar presented the highest values in all the features for angulation, height at 4mm and 6mm, thickness at 6mm and 11mm (Table 4).
When applying the post-hoc test, it was observed that for the angulation there are differen ces between all the roots, with respect to the height 4mm there is a significant difference between the distal root of the second molar and the other roots, referring to the height 6mm, thickness 6mm and thickness 11mm there is a significant difference between the distal root of the second molar and the roots of the first molar, but there is no significant difference between the distal and mesial root of the second molar.
Table 1 Features of the mandibular buccal shelf according to vertical growth pattern.
| - | Features of de MBS | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Vertical growth pattern | Angulation | - | - | - | Height 4mm | - | - | - | Height 6mm | - | - | - | Thickness 6mm | - | - | - | Thickness 11mm | - | - | - |
| - | Average | SD | Min | Max | Average | SD | Min | Max | Average | SD | Min | Max | Average | SD | Min | Max | Average | SD | Min | Max |
| Hypodivergent | 23.4 | 4.9 | 21.1 | 25.7 | 16.3 | 4.2 | 14.6 | 18 | 11.3 | 4.4 | 8.9 | 13.7 | 3.2 | 1.8 | 2.3 | 4.1 | 5.0 | 3.0 | 3.5 | 6.4 |
| Normodivergent | 27.5 | 5.0 | 25.2 | 29.9 | 17.1 | 2.8 | 15.7 | 18.5 | 13.3 | 3.6 | 11.5 | 15.1 | 3.7 | 1.3 | 3.1 | 4.3 | 5.4 | 1.3 | 4.8 | 6.0 |
| Hyperdivergent | 27.3 | 7.1 | 23.9 | 30.6 | 17.5 | 3.3 | 15.7 | 19.2 | 14.4 | 4.5 | 12.0 | 16.8 | 3.8 | 1.5 | 3.1 | 4.5 | 5.4 | 1.8 | 4.6 | 6.2 |
| p-value* | - | 0.052 | - | - | - | 0.546 | - | - | - | 0.158 | - | - | - | 0.454 | - | - | - | 0.759 | - | - |
*ANOVA test; SD, estándar desviation; Min, minimum; Max, máximum.
Table 2 Features of the mandibular buccal shelf according sex.
| - | Features of de MBS | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Angulation | - | - | - | Height 4mm | - | - | - | Height 6mm | - | - | - | Thickness 6mm | - | - | - | Thickness 11mm | - | - | - |
| - | Average | SD | Min | Max | Average | SD | Min | Max | Average | SD | Min | Max | Average | SD | Min | Max | Average | SD | Min | Max |
| Male | 25.3 | 5.5 | 22.9 | 27.6 | 16.9 | 3.0 | 15.5 | 18.3 | 13.0 | 3.4 | 11.4 | 14.5 | 3.3 | 1.3 | 2.8 | 3.9 | 4.8 | 1.6 | 4.1 | 5.5 |
| Female | 26.7 | 6.3 | 24.5 | 28.7 | 17.0 | 3.2 | 15.8 | 18.2 | 13.1 | 4.8 | 11.2 | 14.9 | 3.7 | 1.7 | 3.2 | 4.3 | 5.6 | 2.3 | 4.8 | 6.4 |
| p-value* | 0.402 | 0.829 | 0.611 | 0.343 | 0.143 |
*Student's T test; DSDE, standar desviation; Min, minimum; Max, máximum.
Table 3 Features of the mandibular buccal shelf according hemiarcade.
| - | Features of de MBS | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hemiarcarde | Angulation | - | - | - | Height 4mm | - | - | - | Height 6mm | - | - | - | Thickness 6mm | - | - | - | Thickness 11mm | - | - | - |
| - | Average | SD | Min | Max | Average | SD | Min | Max | Average | SD | Min | Max | Average | SD | Min | Max | Average | SD | Min | Max |
| Left | 25.3 | 5.5 | 24.5 | 28.8 | 15.7 | 3.7 | 15.4 | 17.9 | 12.3 | 4.6 | 10.3 | 14.4 | 3.6 | 1.7 | 3.2 | 4.7 | 5.4 | 2.5 | 5.0 | 7.0 |
| Right | 26.8 | 6.4 | 24.6 | 30.0 | 16.6 | 6.4 | 16.0 | 18.6 | 13.6 | 3.8 | 12.1 | 15.2 | 3.5 | 1.3 | 3.2 | 4.3 | 5.1 | 1.6 | 4.8 | 6.1 |
| p-value* | 0.326 | 0.390 | 0.251 | 0.914 | 0.679 |
*Student's T test; SD, standar desviation; Min, minimum; Max, maximum.
Table 4 Features of the mandibular buccal shelf according reference root.
| - | Features of de MBS | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference rooth | Angulation | - | - | - | Height 4mm | - | - | - | Height 6mm | - | - | - | Thickness 6mm | - | - | - | Thickness 11mm | - | - | - |
| - | Average | SD | Min | Max | Average | SD | Min | Max | Average | SD | Min | Max | Average | SD | Min | Max | Average | SD | Min | Max |
| Mesial root first molar | 18.8 | 4.4 | 16.1 | 21.5 | 15.8 | 3.8 | 13.5 | 18.1 | 8.9 | 4.9 | 5.9 | 11.8 | 2 | 1.1 | 1.3 | 2.6 | 4 | 1.4 | 3.1 | 4.9 |
| Distal root first molar | 22.4 | 4.9 | 19.4 | 25.4 | 19.1 | 2.9 | 17.3 | 20.9 | 14.3 | 3.8 | 11.9 | 16.6 | 2.6 | 1.7 | 1.6 | 3.7 | 5.7 | 1.8 | 4.5 | 6.8 |
| Mesial root second molar | 32.6 | 5.4 | 29.3 | 35.8 | 21 | 2.6 | 19.4 | 22.6 | 17.4 | 2.8 | 15.7 | 19.2 | 4.8 | 1.9 | 3.7 | 6 | 7.8 | 1.4 | 7 | 8.7 |
| Distal root second molar | 38.4 | 7.7 | 33.7 | 43.1 | 22.4 | 2.5 | 20.9 | 23.9 | 19.7 | 3.1 | 17.8 | 21.6 | 6.7 | 1.8 | 5.6 | 7.8 | 8.6 | 1.3 | 7.7 | 9.4 |
| p-value* | P<0.05 | P<0.05 | P<0.05 | P<0.05 | P<0.05 |
*ANOVA test; SD, standar desviation; Min, minumum; Max, maximum.
Discussion
It is important to know the bone features and the anatomical variability of the Mandibular Buccal Shelf (MBS) according to the vertical growth pattern presented by the patients in order to obtain an adequate reference during the insertion of the extraalveolar miniscrews and thus avoid contact with any tooth root or other anatomical structure such as the Inferior Dental Canal (IDC), since this turns out to be a frequent cause of failure of the miniscrew (7). The CBCT is very useful for the evaluation of this zone, although no investigations indicate that this examination is indispensable or justified for this use (10).
In the present study, it was found that there were no statistically significant differences in the bone characteristics of the MBP according to the vertical growth pattern. These findings partially agree with those previously reported by Escobar- Correa et al. (14) who indicated that the hypodivergent pattern had a tendency to higher values but this difference was not significant.
In contrast, other authors did find significant differences, Triverdi et al. (21) reported that the hypodivergent group presented a slope angle with a larger area than the hyperdivergent group. Also, Gandhy et al. (22) found that the hypodivergent pattern has a wider MBS, but lower height than the hyperdivergent one. These differences in the results found in the present study and other investigations could be related to the different places of origin of the study populations and their individual and local anatomical variations, and influenced by genetic, racial or environmental factors specific to each region (1,6,8,9).
The horizontal growth pattern is a variable that has not been evaluated in this study and could have influenced the results obtained. In some previous investigations, they have evaluated the Class III group, which is usually the one with the greatest requirement for extraalveolar orthodontic miniscrews in MBS (1,6). Parinapucham et al. (23) found that between hyperdivergent and normodivergent class III subjects, there were no differences for MBS cortical slope angle and bone thickness. While Aleluia et al. (15) found that Class III hypodivergent subjects had greater bone thickness than the other groups.
In this study, the characteristics of the MBS were also evaluated according to sex and the side of the hermiarch, finding that there were no significant differences in both cases, which coincides with what was previously reported by other authors (14,15). Also, Farnsworth et al. (24) observed that there was no difference in the cortical thickness of the mandibular alveolar bone between men and women. In contrast Gandhy et al. (22) reported that alveolar bone height in hypodivergent and hyperdivergent pattern subjects is significantly higher in men than in women. It is recommended to carry out studies with a larger and balanced sample between males and females to reduce any possibility of error in interpretation.
In this investigation, it was observed that the angulation, height and thickness of the MBS presented higher values the furher back its location, being the bone surrounding the distal root of the second molar, the place with the best features for the placement of extraalveolar miniscrews. While the bone of the mesial and distal root of the first molars did not have sufficient features to ensure adequate installation, as reported by Nucera et al.
(7) in a preliminary evaluation where it was considered that a minimum cut-off value of the buccal extension of the MBS for safe insertion is 5mm thickness of the buccal bone (1.7mm root safety distance, 1.6mm screw diameter, 1.7mm vestibu- lar cortical bone safety distance).
Regarding the angulation of the MBS, it was found in the mesial root of the first molar 18.8°±4.4°, in the distal root of the first molar 22.4°±4.9°, mesial root of the second molar 32.6°±5.4° and distal root of the second molar 38.4°±7.7°, these results are similar to those reported in other studies in a Colombian population (14), while they are lower compared to that reported by Chang and colb. (1) who evaluated subjects born in Taiwan. This suggests that subjects of latin origin could present a lower projection of the MBS than those of asian origin.
Greater bone height was found in the measurements at 4mm compared to 6mm in all roots. Being the distal root of the second molar at 4mm the one with the highest value with 22.4°±2.5°, this area coinciding with that reported by Correia et al. (14) 18.7°±3.8° and Nucera et al. (7) with values of 19.84±3.28 and 19.98±3.22 mm for the right and left sides. This indicates that closer the miniscrew is placed to the root of the tooth, the greater the bone height will be, but it must be kept in mind to leave a safety distance in order to avoid injuring the tooth during its insertion.
Regarding the thickness of the BMS, the present findings agree with previous studies in that the highest value was found 11mm from the CEJ and in relation to the distal root of the second molar. Correia et al. (14) found 7.6±1.6mm at 11mm CEJ, Nucera et al. (7) reported 7.88±1.71mm on the right side and 7.71±1.69mm on the left side. While other authors found slightly lower values, but they measured 8mm from the CEJ (9,25).
In the present investigation, greater bone thickness was found on the distal surface of the mandibular second molar, with an average value of 8.6±1.3mm at 11mm from the CEJ. The data obtained show that the buccal bone thickness increases in the apical and distal portions of the MBS.
It is important to mention that the thick- ness of the soft tissue surrounding the MBS is a variable that has not been taken into account in this study, but it is recommended to evaluate it in future research because it can compromise the long-term stability of the miniscrew according to various authors (7,14,21).
Conclusions
There are no significant differences in the bone features of the MBS between the hypodivergent, normodivergent and hyperdivergent vertical growth patterns, nor between the male and female sexes, nor between the right and left hemiarches.
The angulation, bone depth and thickness increase progressively from the buccal bone to the mesial root of the mandibular first molar to the distal root of the second molar.
The MBS shows greater bone height at 4 mm buccal from the CEJ and greater thickness at 11 mm apical from the CEJ regardless of the reference tooth.
The optimal site for the insertion of minis- crews in the MBS is the buccal bone adjacent to the distal root of the mandibular second molar 4mm buccal to the CEJ.
Ethical considerations
This study was approved by the Institutio- nal Research Ethics Committee of the Universidad Peruana Cayetano Heredia with registration code 207035, dated October 15, 2021.
Author contribution statement
Conceptualization and design: L.A.G.G. and V.E.R.G.Ch.
Literature review: L.A.G.G. and V.E.R.G.Ch.
Methodology and validation: L.A.G.G.
Formal analysis: V.E.R.G.Ch.
Research and data collection: L.A.G.G. Resources: L.A.G.G. and V.E.R.G.Ch.
Data analysis and interpretation: L.A.G.G. and V.E.R.G.Ch.
Writing-preparation of the original draft: L.A.G.G.
Writing: proofreading and editing: V.E.R.G.Ch. Supervision: V.E.R.G.Ch.
Project administration: L.A.G.G.
Acquisition of funds: Self-financed.
















