Introduction
In recent years, amalgam, once the predominant restorative material, has been replaced by tooth color-like materials, such as composite resins, which offer aesthetic advantages and more conservative preparation techniques (1). Composite resin restorations in posterior teeth have shown annual failure rates ranging from 1 to 8%, and the main reasons for replacement being the presence of fractures and secondary caries (2,3). Thus, the technological improvement of restorative materials and adhesive techniques has been observed in literature, focusing on developing alternative clinical possibilities.
In order to improve the biochemical interaction properties of the materials with dental tissues and decrease the replacement rate due to secondary caries, some chemical and structural modifications have been proposed. Evidence showed that calcium, phosphate, and fluoride ions are associated with increasing the resistance of tooth tissue to acid attack and biomineralization of dentin (4,5,6,7,8). The release of fluoride ions saturates the liquid phase in the restoration-dentin interface, resulting in the precipitation of CaF2 crystals, which have been advocated to negatively affect bacterial metabolism (9) and enhance remineralization (4). Recent evidence suggests that the remineralization of dentin can be achieved with the aid of bioactive materials that promotes calcium ion release (10,11).
Thus, a new generation of bioactive materials has been developed and introduced commercially, as a result of a continuous evolution in dental materials sciences. Biodentine™ is attributed as one of the first bioceramic successfully introduced in dentistry, and is marketed as a replacement material for coronal and root dentin. The composition of Biodentine™ consists of tricalcium silicate, zirconium oxide, and some other additives, such as calcium carbonate, which is added to the powder, and calcium chloride, which is added to the liquid to accelerate the setting reaction (12). Likewise, ACTIVA™ Bioactive Restorative is described as a hydrophilic resin-based bioactive self-adhesive material that stimulates hydroxyapatite formation and natural remineralization at the tooth-material interface by releasing significant amounts of calcium, phosphate, and fluoride (4,13).
Moreover, Cention N™ has been introduced as a powder-liquid filling material containing alkaline glass fillers, capable of releasing fluorides, calcium, and hydroxide ions, and can be used as a bulk material (14,15).
Class II resin composite restorations primary causes of failure are recurrent caries (8), tooth fracture (16), restoration fracture (17), and post-operative sensitivity (18). Previous retrospective and prospective clinical studies have shown that caries and fractures are the main reasons for the replacement of this type of restorations (19). Moreover, studies reported that the risk of marginal ridge fracture could be influenced by the technique and the material used in Class II restorations (16,19,20,21). Consequently, the fracture resistance of restorative materials is a critical factor for the clinical success of Class II MOD restorations. Up to date, there is no study evaluating the fracture resistance and some biomineralization characteristics of these materials. Thus, the objective of our study was to evaluate the biomechanical and chemical behavior of various bioactive materials in class II restorations. The null hypothesis was that there is no difference in the fracture resistance of MOD restorations and calcium ion release between the tested materials.
Materials and methods
The research protocol was approved by the Ethics Committee of Universidad de Costa Rica (CEC-388-2021).
Sample preparation
Forty-eight (n=48) freshly extracted non-carious human molars, stored in 37 °C distilled water, were used. Teeth were cleaned with periodontal curettes to remove residual plaque, soft tissue remnants and calculus. All teeth were evaluated carefully for cracks, caries, wear facets or structural defects under a stereomicroscope (Nikon SMZ645, Tokyo, Japan) at ×20 magnification. Moreover, the dimensions of the teeth were measured with a digital caliper (Mitutoyo, Tokyo, Japan) to ensure that the selected teeth presented an occlusal surface area varying no more than 10% of the sample average.
The teeth were inserted into a PVC cylinder with polystyrene resin (Polyether Impregum soft 3M ESPE, Minnesota, USA) with the cementum- enamel junction (CEJ) 2mm above the surface of the acrylic resin. Each tooth was positioned in a block so that buccal and lingual cusp tips were in a horizontal plane parallel to the base of the mount.
Standardized MOD preparations were performed using a high-speed handpiece under water cooling. The cavities were prepared using bur #2131 (KD Sorensen, Sao Paulo, Brazil), and the burs were changed every 4 teeth (16). The class II MOD cavities were performed by a single operator and, standardized as follows: lingual-buccal isthmus width of 4mm and occlusal depth of 3mm, in the proximal box 4mm of occlusal depth, and 1-2mm above the cementoenamel junction of the proximal box (mesially and distally).
The specimens were randomly divided into four groups (n=10) according to the bioactive materials placement techniques. Group 1 (control group): After preparing the cavity, a metal matrix held by a Tofflemire retai- ner (S.S. White Dental Manufacturing Company, Philadelphia, USA) was placed around the tooth. A universal adhesive employing the selective etching technique (Single Bond™ Universal, 3M ESPE, Deutschland, Germany) was applied on the cavities with a disposable microbrush according to the manufacturer's instructions. Light curing was performed using a light-emitting diode light- curing unit (Valo, Ultradent Products Inc., South Jordan, UT, USA) for 20s, with a light intensity of 1200 mW/cm. Successive increments (2mm) of a nano-filled resin composite (Filtek™ Z350 XT, 3M ESPE, Minnesota, USA) were first applied horizontal to the gingival wall, and then, to the pulpal wall. The final increment was applied according to the contour of the tooth. All the increments were light-cured separately. Immediately after filling, the samples were finished with diamond burs at low speed with air-water spray and polished with a disc system (OptiDisc System, Kerr Corporation, Orange, CA, USA).
Group 2: The axial, pulpal and gingival walls of each Class II cavity were lined (2mm) with Biodentine™ (Septodont (Saint-Maur-des- Fossés, France) using a 1mm diameter ballpoint instrument. The matrix band was placed and secured using a Tofflemire matrix retainer. The remainder of the cavity was then treated with the universal adhesive and restored with the composite resin at full contour until replacing the enamel, as described for Group 1.
Group 3: A matrix band was placed and secured also using a Tofflemire matrix retainer, and the cavity was then restored at full contour with Cention N™ (Ivoclar Vivadent, Liechtenstein, Germany) according to the manufacturer's instructions.
Group 4: A matrix band was also placed and secured using a Tofflemire matrix retainer and the cavity was then restored at full contour with Activa™ Bioactive-Restorative (Pulpdent, Watertown, MA, USA) according to the manufacturer's instructions.
The teeth were stored at 37°C and 100% humidity in calcium-free PBS for 7 days.
Fracture resistance and fracture mode evaluation
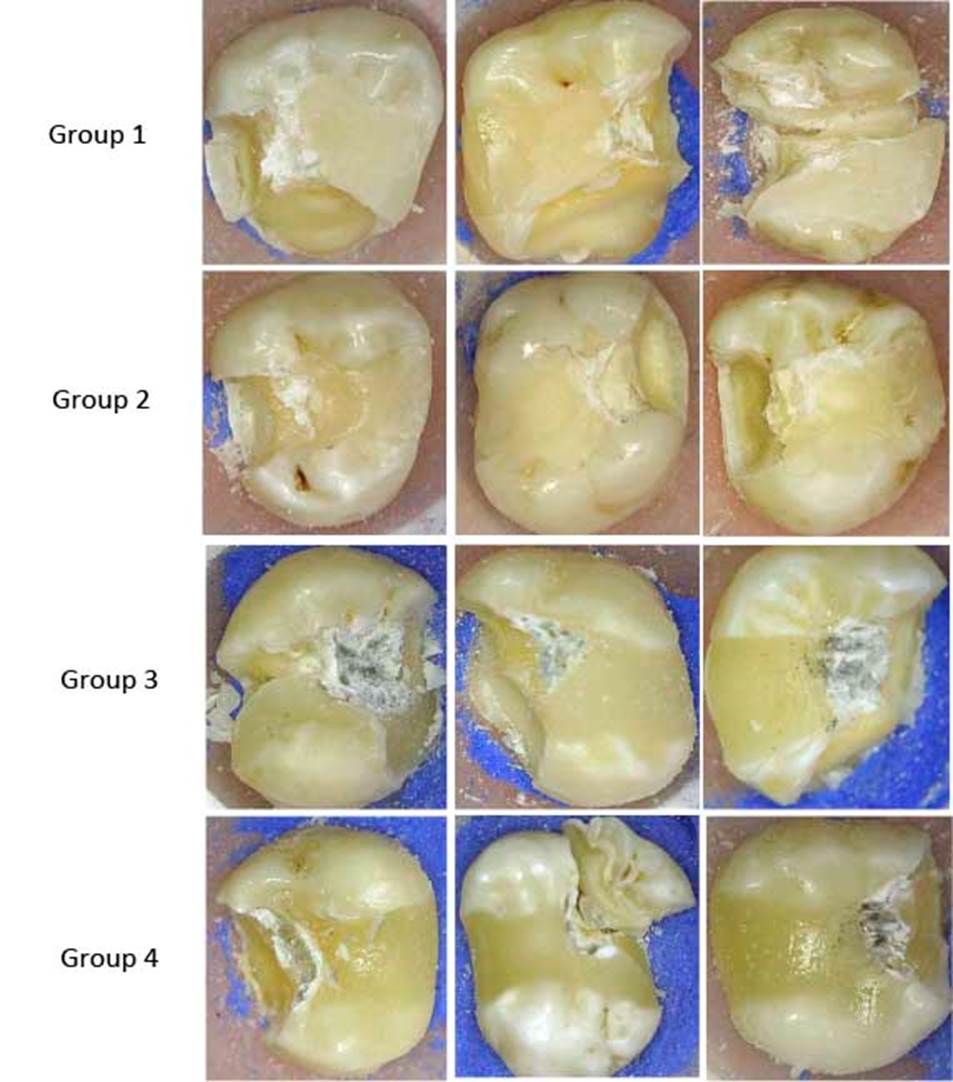
The samples were submitted to a compressive load until fracture (load cell capacity 5kN), with a stainless-steel ball bearing of 6mm in diameter, in a universal testing Machine (Electropuls E 3000, Instron Corporation, Norwood, MA, USA) at a cross-head speed of 5mm/min until specimen fracture. The failure modes of each specimen were assigned to one of four categories and assessed by a single-blinded calibrated evaluator (22): (I) Failure at the restorative material; (II) Failure at the restorative material and coronal tooth structure; (III) Failure at the restorative material and cervical tooth structure with possible periodontal repair and (IV) severe root and crown failure, which were deemed non-restorable. Representative failures/ fractures modes were photographed.
Statistical analysis
Fracture loads were recorded in Newtons (N) and analyzed using an analysis of variance (ANOVA) followed by post-hoc Tukey's Test at a level of significance of p<0.05. The data for fracture patterns are reported, only, as descriptive. The statistical analysis was performed using Prism 9 GraphPad (GraphPad Software Inc., San Diego, CA, USA).
Scanning electron microscopy (SEM)
Two random specimens from each group were selected for SEM observation. Each speci- men was then sectioned, at the half, parallel to the longitudinal axis of the crown using an ISOMET diamond saw (Buehler, Lake Bluff, NY, USA). Specimens were dried at room temperature, mounted on an aluminium stub, placed in sealed glass vials with silica and then in a vacuum chamber, and sputter-coated with a 300Å gold layer. The elemental composition of the materials was analyzed by energy-dispersive X-ray analysis (EDAX) with a scanning electron microscope (S-570, Hitachi, Tokyo, Japan) at 15kV. Serial SEM photomicro- graphs at different magnifications were taken to descriptively analyze the dentin-material interface.
Determination of PH and calcium ion release
Specimens from all the experimental materials (n=5) were placed separately in sterile vials and immersed in a calcium-free and magnesium-free phosphate-buffered saline (PBS) solution at 37°C for 1 month. The PBS solution was collected at 30 days to measure the pH and calcium ion release. After the collection of the solution, the pH was determined with a pH meter (Orion Star A 221, Waltham, MA, USA). Calcium ion release was measured using a Varian atomic absorption spectrophotometer (Spectra A220 Fast Sequential, Palo Alto, CA, USA). Data obtained were recorded and subjected to descriptive analysis.
Results
The means and standard deviation of the load required to fracture the Class II restorations of each of the four groups are displayed in Table 1 and Figure 1. Group 1 (Filtek™ Z350 XT) recorded the highest average load, while Group 2 restorations (Biodentine™/Filtek™ Z350 XT) had the lowest fracture load (p<0.05). Group 1 displayed statistical differences with all groups (p<0.05). Group 3 showed numerically higher fracture resistance than Group 4; however, no statistically significant differences were detected among then.
Table 1 Mean and standard deviation (SD) of the fracture resistance of Class II restorations test.
| Group | Mean | SD |
|---|---|---|
| Group 1 (Filtek™ Z350 XT) | 2540 | 345.9 |
| Group 2 (Biodentine™/ Filtek™ Z350 XT) | 1142 | 280.4 |
| Group 3 (Cention N™) | 1821 | 239.0 |
| Group 4 (Activa™) | 1541 | 321.0 |
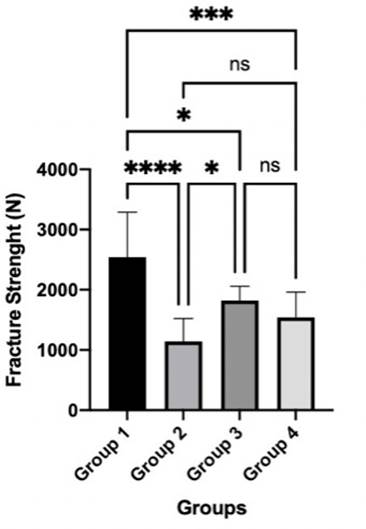
Figure 1 Means and standard deviations for fracture resistance loads (N) *Indicate statistical differences between groups.
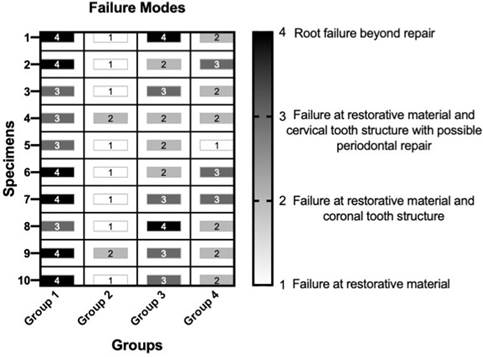
The modes of fracture of all the groups are described in Figure 2 and Figure 3. Group 1 displayed most samples with root failure beyond repair (60%) and failure at restorative material and cervical structure (40%). In Group 3, a mixed-mode of failure was observed, being predominant in categories 2 (40%), 3 (40%) and 4 (20%). Group 4 showed 30% of the samples with failure at category 3, 60% at category 2,10% at category 1, and just one sample with root failure beyond repair. Group 2 displayed failure at the restorative material in 80% of the samples.
The chemical compositions by EDAX of the tested materials are described in Figure 4. Biodentine™ showed Ca and Si at higher concentrations compared to the other materials. Filtek™ Z350 XT presented Si in higher concentrations than other components. Cention N™ and Activa™ denoted an intermediate amount of Ca and the presence of Si.
SEM evaluation showed material-dentin interface (Figure 5). Biodentine™ showed a more homogeneous marginal adaptation with dentin and a more porous surface.
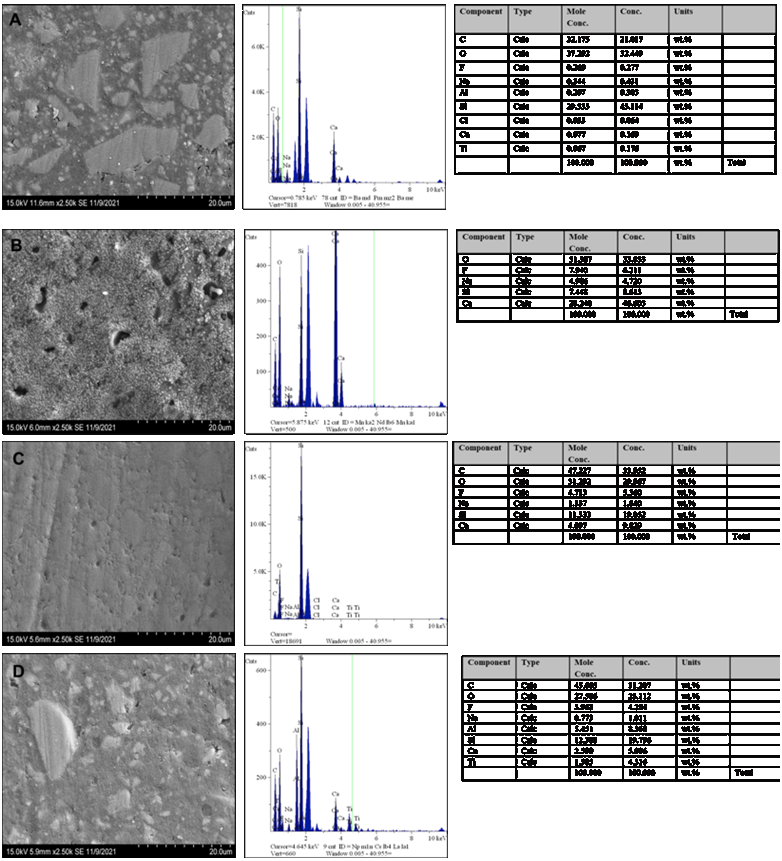
Figure 4 EDAX spectrum for (a) Filtek™ Z350 XT, (b) Biodentine™/ Filtek™ Z350 XT, (c) Cention N™, and (d) Activa™.
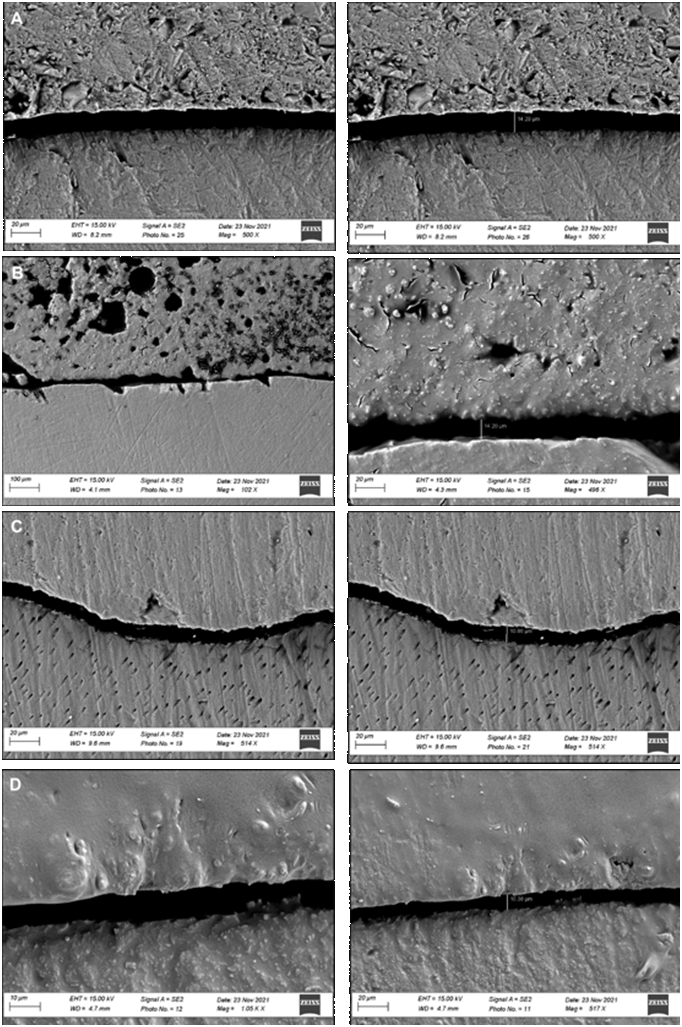
Figure 5 Representative SEM microphotograph of material-dentin interface. (A) Filtek™ Z350 XT, (B) Biodentine™/ Filtek™ Z350 XT, (C) Cention N™, and (D) Activa™.
Regarding the pH, all the bioactive materials showed a rapid initial rise from days 1-7 followed by a decline on day 30. Biodentine™ presented higher alkalizing activity than the other materials. Filtek™ Z350 XT remained near 7.2.
All the materials showed the ability to release calcium ions. Biodentine™ released the highest cumulative amount of calcium (576±36mg/L). Cention N™ and Activa™ displayed 10±1mg/L and 12±1mg/L, respectively. Filtek™ Z350 XT showed a lower cumulative amount of calcium ions (4±1mg/L).
Discussions
Increasing demand for esthetics and enduring restorations has led dental researchers to focus on the development of novel materials that can display optimal physical, mechanical, and biological properties. Our study was designed to assess the performance in Class II MOD restorations, alkalinity potential, and calcium ion release of some bioactive materials. It was possible to observe a significant difference in all tests between the materials, leading to the rejection of the null hypothesis.
Several studies have investigated the fracture resistance of Class II MOD restorations because of their clinical relevance (1,2,22,23,24). However, to our knowledge, this is the first study that correlates the performance of these bioactive materials in class II restorations and their ion release capacity.
Materials incorporating agents that possess bioactivity and promote remineralization of the tooth by releasing calcium, phosphate, and fluoride ions are examples of the trend to develop aesthetic restoratives with the ability to inhibit secondary caries (4). Previous studies reported that bioactive materials release some components in the medium and trigger mineral deposition, which leads to the formation of an interfacial layer with tag-like structures in the intratubular dentin, suggesting that this biomineralization process could minimize leakage (7) and positively influence the bond strength of the materials (25,26). This micromechanical interaction induced by calcium silicate biomaterials improves the adhesion between materials and dentin (18,25,26,27). Our results demonstrated that the alkalinization potential and calcium ion release of Biodentine™ (576±36 mg/L) were much higher than the other materials tested. Cention N™ (10±1mg/L) and Activa™ (12±1mg/L) displayed unsatisfactory results, considering both materials' marketing. The ability of bioactive materials to promote the biomineralization process in their interface with dentin was previously correlated to the rate of calcium ion release (25,28). Thus, we suggest that the higher amounts of calcium ions released by Biodentine™, due to the major calcium content as noted by SEM-EDAX, imply greater biomineralization potential in the dentin- material interface.
Class II restorations have always provided a restorative dilemma due to the presence of recurrent caries, tooth/restoration fractures, discoloration, polymerization shrinkage, and post-operative sensitivity (16). Therefore, this study reveals new alternatives for the restoration of posterior teeth. Our results demonstrated that class II MOD restorations filled with Filtek™ Z350 XT showed the higher fracture resistance of all materials tested. Cention N™ displayed higher numerical fracture resistance than Activa™; however, no significant differences were observed. The lowest fracture resistance values were displayed by Group 2, in which Biodentine™ was used as a liner or pulp capping material, and then, Filtek™ Z350 XT was used to restore enamel (Group 2).
Regarding the performance of new materials, Van Dijken et al. demonstrated, in a randomized controlled prospective clinical trial, that the annual failure rate of Activa™ was 24.1% versus 2.5% for a resin composite (4). The authors stated that the main reasons for failure were fractured restorations, postoperative symptoms, and secondary caries. Moreover, this clinical study was stopped due to the unacceptable, very high one-year failure frequency, and no further evaluation was performed. Thus, the authors concluded that the use of Activa™ in Class II cavities, applied as instructed by the manufacturer after a short phosphoric acid pretreatment but without adhesive system, resulted in a non-acceptable, very high failure frequency after one year (4). In contrast, Cention N™ showed, ex vivo, adequate but lesser strength, and flexural values than composite resins (20,29), but with minor microleakage (20).
Composite resins with a higher elastic modulus produce more rigid restorations, which may transmit a higher load to the underlying tooth structure (22,30). Cention N™(31,32,33), Activa™(34), and Biodentine™(35) presented lower elastic modulus and shrinkage stress than resin composite-based materials. Class II restorations are often associated with clinical failure due to the high shrinkage stress at the restorative composite/adhesive interface (22). In this sense, group 1 restorations presented a higher fracture resistance and a greater incidence of root and crown failure, probably because of the higher elastic modulus of the resin composite material, and shrinkage stress values at the cavity walls (16,22,36). Consequently, after axial compressive loading, the cohesive fracture in the composite occurred concurrently to the root and crown (22). Therefore, the highest elastic modulus of a material, due to a higher filling load, has led to the need for higher compressive loading until the restoration fracture, which causes force propagation to the tooth and higher catastrophic cohesive crown/root fractures (16,22,36). Considering the failure mode results of this study, we can conclude that samples of group 2 displayed, from a clinical perspective, the most favorable failure mode. It is assumed that the material with higher resistance to fracture could obtain better clinical performance. However, based on our results, we can extrapolate that the use of a bioactive liner/pulp capping material with composite resin can be the ideal mode of restoration to approach the benefits of this bioactivity potential, marginal adaptation and the bond strength of composites resins. Furthermore, a more beneficial mode of failure can permit tooth rehabilitation and survival. Suitable physicochemical properties have been described for all the bioactive materials; however, additional research to assess the biological interaction and bond strength in a simulated oral environment may provide information to improve the clinical performance of Class II MOD restorations.
Conclusions
Within the limitations of this in vitro study, it can be concluded that higher resistance to fracture of Class II MOD restorations was obtained when an incremental filling technique with composite resin was used; however, it was highly associated with catastrophic failure. Conversely, Biodentine™ presented a more significant bioactivity potential, and its use as a liner, in addition to composite resin, promoted the most favorable failure mode.