Introduction
In December 2019 an outbreak of pneumo- nia associated with a new virus, the severe acute respiratory syndrome (SARS) Coronavirus 2, began in Wuhan, Hubei province, China. On January 30, 2020, the World Health Organization (WHO) declared the outbreak a public health emergency of global importance (1). This situation triggered an imbalance in the activities of millions of people, inducing an abrupt change in the daily routine of the population in general, causing anxiety, anguish, and concern for various reasons such as fear of contracting the virus, the possibility of getting sick and/or infecting a family member, prolonged isolation, and fear of long-term effects on the global economy (2).
In response to the different changes that were generated in the forms of communication, work and study during the SARS-CoV2 pandemic, the population experienced higher levels of stress that predisposed them in a greater extent to bruxing (3).
Bruxism is the repetitive masticatory muscle activity, this behavior is manifested with rhythmic or arrhythmic movements at night (sleep bruxism) or during the day (awake bruxism) characterized by repetitive or sustained dental contact and reinforcement or thrust of the jaw (4), that induces clinical oral manifestations when they accumulate. This propitiates a negative effect on the dental structure of the patient who presents symptoms derived from the constant clenching and grinding of the teeth. This series of oral and motor behaviors can present to varying degrees of intensity and persistence over time, which on many occasions is usually unconscious (3). Opinions regarding the etiology of bruxism are constantly discussed, growing evidence suggests a combination of psychosocial, physiological, biological and exogenous factors (5,6). An increase in bruxism activity may be associated with several potential risk factors and concurrent conditions, depression, anxiety and stress playing an important role in promoting and perpetuating the habit (5,7). In the stomatognathic system the manifestations of bruxism has repercussions on dental, muscular and joint structures. Such repercussions as non-functional wear facets on anterior and posterior teeth, referred audible sounds, fractures of teeth and restorations, dental mobility in the first hours of the morning, hypertrophy of the masseter and temporalis masticatory muscles, pain in the temporomandibular joint (TMJ), limitation in occlusal opening (7).
Currently, both bruxism and stress are consistent contributors to medical problems in the world. Manfredini D. et al. and Hermesh et al. showed a prevalence between 22.1% and 31% and hypothesize 80% of the population will present signs of this behavior at some point in their lives (8,9). The knowledge of the reported epidemiological data refers to sleep bruxism (SB), using an objective diagnostic method that is polysomnography (PSG) (10), however, when self-reporting symptoms of bruxism, the prevalence of data obtained range from 5.5 % when confirmed by PSG and 7.4% when only self-reported. Through structured questionnaires and interviews self-reporting can be useful to collect information on awake bruxism, as well as perceived bruxism activity and possible associated factors (11).
It is unknown if the population of young adult between the ages of 18 and 24 perceived high levels of stress during the COVID-19 pandemic, it is unclear if signs and symptoms of bruxism may have been accentuated as a result of this. Due to the aforementioned, the objective of this study was to evaluate the self-perception of stress and symptoms of bruxism caused by isolation during the COVID-19 pandemic, as well as provide frequency to these variables based on gender and the academic areas of study among students belonging to the Institute of Health Sciences of the Autonomous University of State.
Materials and methods
A cross-sectional and descriptive study was approved by the Ethics Committee of the Autonomous University of the State of Hidalgo. This study included ICSa students from 18 to 24 years of age enrolled in the July-December 2021 term, who volunteered to answer the form in its entirety to participate in the study, the exclusion criteria excluded students who to their best recollection, used an occlusal guard as a treatment for disorder of the TMJ, those who stated that they did not have a restoration in their mouth such as resin, amalgam, inlay and crown, as well as fixed appliances, since this data was not clinically verified, lastly manifest not remembering having received dental treatment in the last 6 months. The survey was carried out in a single moment in October and November 2021, the students were invited to participate in the research through a shared link to the form sent to their institutional email. The objectives of the study were previously explained to them, providing them with information regarding bruxism so that they understood the intention of the form they were going to answer.
Data collection
A questionnaire was performed through Google Forms with 33 items, divided into 3 sections:
1ST. section. personal and academic data
General information about age, gender, study area, and semester of the students.
2ND section. symptomatological data of bruxism
This component describes if they wore an occlusal guard, perception of teeth clenched or gnashed, in what situations, time of day and since when symptoms started, before o during the isolation, which allowed the generation of a comparison between the periods. In addition, were considered symptoms such as pain or fatigue in the face, neck and shoulders pain, difficulty in opening the mouth widely, abnormal noises when opening and closing, if they perceived accelerated wear on their teeth, according to the participant's perception, as well as not remembering having received dental treatment in the last 6 months. Finally, they were asked if they felt tired regardless of how many hours they slept and if someone had mentioned to them that they snored.
3RD. section. perceived stress data
In the last section, different factors by which the student could have been affected by stress and anxiety were considered. This included being affected by an unexpected event, their ability to control the important things in their life, the management of small problems, such as coping with changes and the recent frequency with which they feel nervous, stressed and angry, among others factors. The PSS-14 perceived stress scale was used in consideration for the cut-off points observed in Table 1. The subjects of the study with "no stress" and "mild stress" were considered as subjects who had no stress, while the subjects with "moderate stress" and "severe stress" were considered as subjects with stress.
Table 1 Assessment instrument to measure perceived stress level.
| Values | Stress Level |
|---|---|
| 0-14 | No Stress |
| 15-28 | Mild Stress |
| 29-42 | Moderate Stress |
| 43-56 | Severe Stress |
To determine the presence or absence of stress associated with bruxism, the following parameters were considered:
Presence of high levels of stress without symptoms of bruxism.
Bruxism related to high levels of stress with less than 6 months of evolution.
Symptoms of bruxism with high levels of stress for more than 6 months of evolution.
Minimal stress levels without symptoms of bruxism.
A patient with bruxism was considered one who complied with at least three anamnestic signs, among which one must correspond to the principal type and at least two secondary, as shown in Table 2.
Table 2 Determination of signs and symptoms of bruxism according to its diagnostic classification.
| Bruxism Sign/Symptom | Anamnestic | - |
|---|---|---|
| - | Principal | Secondary |
| Tooth clenching/grinding | X | |
| Pain or fatigue of temple or face | X | |
| Neck and shoulder pain or fatigue | X | |
| Difficulty opening the mouth wide | X | |
| Perception of rapid tooth wear | X | |
| Abnormal noises when opening or closing the mouth | X | |
| Tiredness independent of hours of sleep | X | |
| Snore | X |
Processing and data analysis
The data obtained were recorded in Micro- soft Excel 2016 spreadsheets, percentages and frequencies of the qualitative variables were calculated. The Chi-square test was used for the comparison between variables and a p<0.005 value was considered significant. To find out the difference between symptoms before and during isolation, a 2-way Anova with Tukey's posthoc and Wicolxon was used to find out the difference between the frequency at both times. Statistical analysis was performed in the GraphPad Prism version 9.3.1 program.
Results
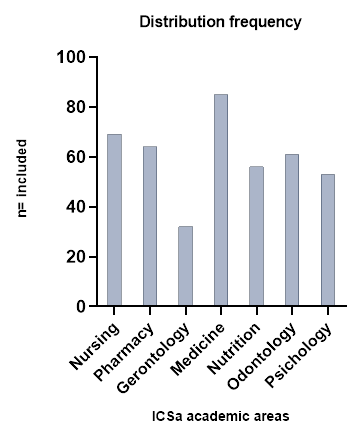
A total of 825 initial respondents, 405 participants who did not meet the inclusion criteria were eliminated, 81 students who did not meet the age range and 324 who were carriers of an occlusal guard and self-reported according to her knowledge, have a restorative treatment in their mouth and stated that they did not remember going to the went to the dentist in the last 6 months (Figure 1). The final sample of 420 students was obtained, made up of 297 (70.72%) women and 123 (29.28%) men, with an average age of 20±1.75 years, divided by academic area (Figure 1) from which the information on their perception of bruxism and the presence or absence of stress it was obtained.
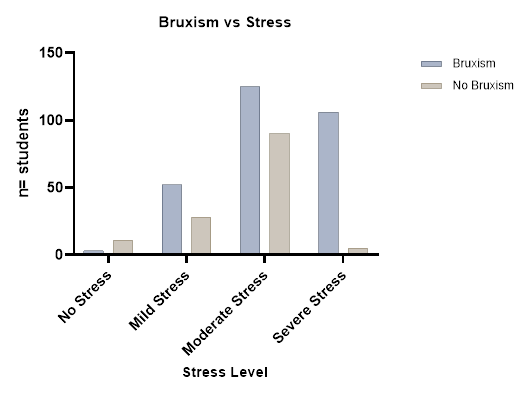
The frequency of bruxism and the level of stress that ICSa students manifested during isolation it was, 14 (3.35%) without stress, 80 (19.04%) with mild stress, 215 (51.19%) with moderate stress and 111 (26.42%) with severe stress, of these 286 (68.10%) with the perception of bruxism and 134 (31.90%) without bruxism, presenting a statistically significant difference between groups p<0.0001 (Figure 2). Observing a direct association of these variables, when stating that there is no stress, the presence of bruxism is not perceived, however as stress levels increase the perception of signs and symptoms of bruxism also increases.
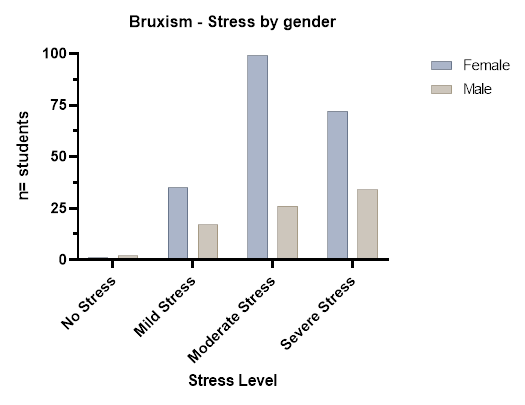
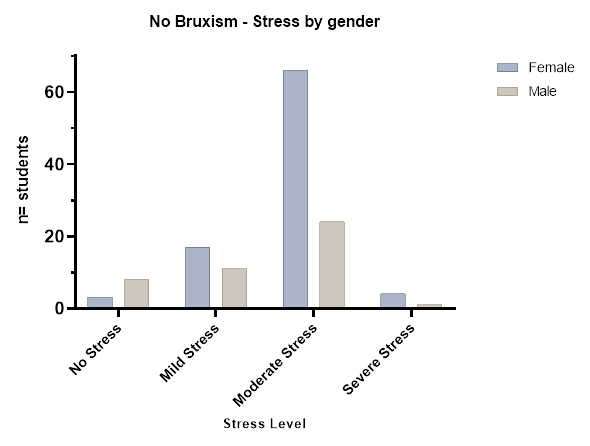
When comparing the frequency of bruxism associated with the level of stress among the students by gender (Figure 3), shows that there is no statistically significant difference (p<0.0746) however, in non-bruxist female students with stress compared with non-bruxist male students there is a statistically significant difference (p<0.0155) (Figure 4). Stating that men and women show signs and symptoms of bruxism when presenting high levels of stress equally, though, women perceive greater stress without showing signs and symptoms of bruxism.
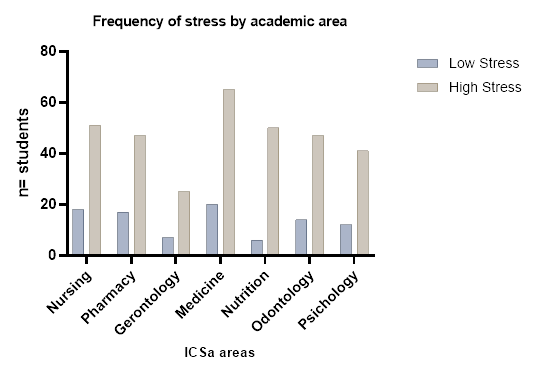
When analyzing differences in stress levels between students from all academic areas in the ICSa during the COVID-19 pandemic, we could not find a statistically significant difference p<0.4623. (Figure 5). Medical students have the highest levels of stress in comparison with the other academic areas.
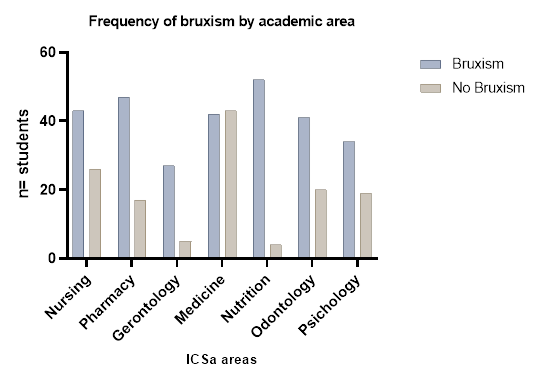
We found a statistically significant difference p<0.0001 between the presence and absence of bruxism in students from the different ICSa areas (Figure 6). The Nutrition area has the highest prevalence of bruxism when compared to other areas.
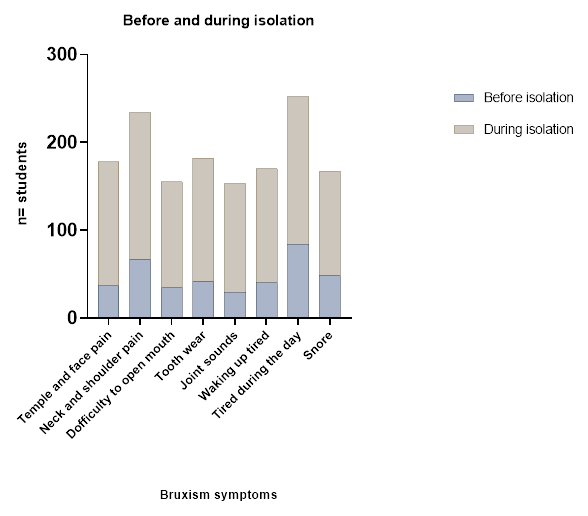
We observed a higher proportion in the perception of bruxism signs and symptoms in the students during isolation due to the COVID-19 pandemic than before p<0.005 (Figure 7). The most common associated symptom was feeling tired during the day followed by neck and shoulder pain.
Discussion
Stress is one of the most widespread health problems in society, it results from the relationship between the person and the events in their environment (12). It is able to cause bruxism, characterized by a series of oral and motor behaviors manifesting with teeth grinding. The result can have an important impact on the aesthetics and quality of life of the person who presents with it (13,14). Sleep disorders (15,16,17), smoking, alcohol and drug use (18), systemic diseases, anxiety, trauma and heredity, all can play an important role in its onset, persistence, as well as frequency and severity (3,13,17).
This report shows an association between a high level of stress and the bruxism, with a prevalence of 68.10%, which agrees with the reporting of 60.80% by Estrada on bruxism in Peruvian dental students (19), observed based on the presence of symptoms such as pain in head and neck muscles and feeling of tiredness during the day. Although the study population was young, we can recognize that a large number of students between 18 and 24 years at ICSa perceived symptoms of bruxism and high levels of stress during the pandemic, which may have been caused by the change of routine that triggered the isolation. The students of the health area self-reported bruxism with high levels of stress, this was specifically observed in the academic area of medicine where a higher frequency of perceived stress was reported. The main factor of increased stress appears to be inadequate coping patterns in their daily lives, which causes symptoms such as grinding, accelerating the wear of their teeth and potential pain in the temple, neck or elsewhere. Similarly, Barbosa reports a high prevalence of bruxism in medical students (100%) (20), however, a higher frequency of bruxism is observed in this report in the academic area of nutrition.
In regards to gender, the results show that there is no significant difference between the frequency of bruxism and stress of men and women, indicating that all students regardless of gender are equally stressed, which has an impact on the increase in signs and symptoms of bruxism. This coincides with the results of Stanton et al. (18), in the same way, Ordoñez and Hernández found no differences between genders in latinamerican students prior to the pandemic (21,22), however, a greater participation of female students answered the form for this report which could have influenced this data. Both Flores and Barbosa report the highest levels of bruxism in the female gender (14,17), which impacts our results with regards to the isolation factor that was generated during the pandemic, causing both genders to become equally stressed. On the other hand, it is important to highlight that when analyzing the group of non-bruxists but with high levels of stress, female students were significantly predominated, coinciding with the results of some reports where the female gender is more affected by psychological distress (depression, anxiety, stress) (23,24,25), being more prone to developing TMJ disorders (26,27).
The academic demands of the university nowadays, specifically in the area of health, affects the coping mechanisms of students in their daily activities responding inadequately to stress triggers. Stress that is generated by the rigor of studying online, which is exacerbated because the student has not been able to carry out their clinical practices in person and with the frequency that they once had previously. According to Winocur E. et al.; having poor coping skills is a possible personality trait that has been associated with an increase in bruxism (6). Kardes et al., report that at the beginning of the year 2020, dental grinding presented an increase in public interest and demand worldwide, however, it was not significant until the period from May to October, where in the US and the rest of the world the number of reports of bruxism increased, along with grinding and clenching (28). This finding indicates that the COVID-19 pandemic had a negative impact on bruxism and its symptoms (29,30,31), consistent with our results.
It is interesting that 68.10% of the students surveyed who present bruxism with high levels of stress have not received dental treatment. Since the elimination criteria included not having had a dental consultation in the last few months, having some restorative treatment or of appliances in the mouth to rule out those that would other influences in triggering this behavior of grinding or clenching the teeth, as well as any other confusing symptom of local origin of the stomatognathic system. However, currently local factors are of lesser etiological importance for this behavior (11,32,33). On the other hand, although students have the opportunity to receive psychological attention either through their institution or in a private practice, the number of students who request psychological channeling at ICSa is very low, these do not agree with the report of the frequency of self-perception of bruxism and student stress during the pandemic isolation. This information makes it necessary to highlight the number of referrals to the psychology area so that high levels of stress do not have repercussions on the dental and psychological health of the student (34), as well as on the development and of decisions of the various activities during their professional training.
At the same time, it was shown the number of cases of bruxism in young adults has been increasing, since the inability to control emotions, unexpected changes, personal problems, accumulation of work, coupled with the lack of social contact (15) have favored an increase in stress and anxiety that has a direct impact on the dental structure and in turn could trigger symptoms associated with problems of the TMJ (35,36), manifesting itself with dental clenching, wear, pain and tiredness when waking up, however, a poor quality of sleep could also be causing some of these symptoms. A possible cause of sleep disorders during the pandemic could be greater use of social networks, sleep being an important factor in the regulation of behavior and emotions, even having an impact on the decrease of the immune system and greater predisposition to any type of infection, as mentioned by some authors (15,17,37,38,39). However, this variable was not taken into account in this report as it focused mainly on signs and symptoms of bruxism and events generating stress during the pandemic and not its consequences, such as quality of sleep.
It is important to mention that bruxism increases in the presence of conditions and disorders that could be present in the young adult population, such as Attention Deficit Hyperactivity Disorder (ADHD), epilepsy, and gastroesophageal reflux (11), so an early diagnosis of bruxism will have a less negative impact on the stomatognathic system, preventing pain in the jaw muscles, complications in prosthetic restorations and mechanical wear of the teeth that results in high dental sensitivity and changes in the condylar position (40,41); in this way, less invasive treatment alternatives can be offered to this group of vulnerable patients. An area of opportunity for future clinical studies on the subject would be to rule out students with a previous diagnosis that could be influencing the presence of symptoms of bruxism, as well as a pre-existing psychological condition, since in healthy individuals, bruxism is not considered a disorder, but as a behavior that can be a risk factor but also a protective factor for certain clinical consequences (4). On this occasion the ICSa student population who were enrolled in their semester were included, which translated generally to healthy students, since those who presented some comorbidity during the pandemic used to be less active. All of them were contextualized on the subject so that they could identify variations from the normal in regards to symptoms of bruxism and carry out their self-report of the symptomatology of this behavior, identifying if they had already suffered from it for more than a year or less than a year, thus associating it with the level of stress that they reported during the period of isolation caused by the COVID-19 pandemic.
Stanton et al. mention that during the pandemic, young single people, unlike those with another marital status, presented higher levels of depression, anxiety, and stress, and these in turn, than elderly people (18). It has been reported that stress and anxiety, as well as emotional overload, are predictors of a high risk for triggering bruxism in healthy people (34,42). These factors were considered in the form applied to ICSa students, which agrees with previous studies (15,43,44,45) that demonstrate the relationship between bruxism and psychosocial factors. Therefore, specific factors may have different relationships with the different types of bruxism (day/night) (11). In this case, the self-perceived bruxism by students is that of wakefulness, mainly related to psychosocial factors (5).
With these results, it is determined that the presence of bruxism in this population group is alarming, because this behavior was not characteristic at this age in young people without associa- ted comorbidities, since the prevalence rates in adults range between 22% and 30% for awake bruxism and between 8% and 16% for sleep bruxism, while in children and adolescents they rise to 40% (35,46). The changes caused by the current COVID-19 pandemic, also induced a renewal in the systematization of multidisciplinary management, which is necessary to reduce the sequelae of isolation stress that has led to an increase in bruxopathic patients. On the other hand, the presence of bruxism specifically associated with stress could be a biomarker (47) with the ability to predict or provide additional information in the diagnosis of emotional illness in students who have sought out psychological counselling. Due to bruxism's association with psychiatric and neurological problems, sleep disorders and drug administration, since the effectiveness of follow-up and support strategies depends on timely suspicion as well as on the accuracy of the diagnosis.
The impact of social isolation is wide-ranging and can be long-lasting. Long-term physical and emotional consequences, leading to a higher risk of developing and perpetuating bruxism and TMJ disorders (16), which could manifest as harmless or even protective behavior. However, when it is associated with one or more harmful health effects in healthy people this manifestation can be considered a risk factor (4). These risk factor can present as damage to the dental structure, restorations present in the mouth, severe chronic pain in the facial and jaw muscles, chewing, speaking and swallowing problems, tension headache, TMJ disorders, irradiated ear pain, as well as hypertrophy of the masseter muscle, among others (48). Currently, non-instrumental approaches to evaluate bruxism include self-reporting, which may be useful to collect information on perceived bruxism activities and possible associated factors (4,11). It is worth mentioning that it is not effective in reporting the intensity and duration of the chewing or muscle activity, since this cannot be easily quantified, these variables were therefore not taken into account in this study. The intention is to make dental professionals aware of the impact that the pandemic had on the perception of high levels of stress, as well as the onset and/or increase in symptoms associated with bruxism in the young adult population (6), in order to provide better treatment options and strategies to control stress in an effort to reduce orofacial pain. The intervention and control of the psychosocial factor is the first step in the management of bruxism, making changes in lifestyle, as well as the use of alternatives to reduce stress such as hypnotherapy, acupuncture, yoga, meditation or some physical activity (44). Based on these results with a high frequency in the self-perception of bruxism and its association with severe stress in ICSa students, it is recommended to carry out clinical and longitu- dinal studies that corroborate the perception data of the students, a limitation that this study had due to the circumstances inherent to the same contingency generated by the COVID-19 pandemic.
Conclusion
A high frequency of symptoms of bruxism in ICSa-UAEH students is associated with severe levels of stress, generated during the social isolation of the COVID-19 pandemic. This is without distinction in gender, but with a higher self-perception of severe stress more prevalent in the area of medicine. Also noted was a high frequency in the perception of symptoms of bruxism in the area of nutrition, which gives us preliminary data on the prevalence of the main signs and symptoms of bruxism that will need to be clinically corroborated to adopt therapeutic measures together with psychological support, that channels stress levels for better student performance when returning to face-to-face activities.
Author contribution statement
Conceptualization and design: M.M.M.H., R.G.A. and J.E.G.S.
Literature Review: M.M.M.H., R.G.A., J.E.G.S. and A.J.M.A.
Methodology and validation: A.J.M.A., C.E.C.S. and C.U.M.A.
Formal Analysis: A.J.M.A., C.E.C.S. and C.U.M.A.
Investigation and data collection: M.M.M.H., R.G.A. and J.E.G.S.
Resources: M.M.M.H., R.G.A., J.E.G.S., A.J.M.A.,
C.E.C.S. and C.U.M.A.
Data analysis and interpretation: C.E.C.S. and C.U.M.A.
Writing-original draft preparation: M.M.M.H. and A.J.M.A.
Writing-review & editing: A.J.M.A., C.E.C.S. and C.U.M.A.
Supervision: A.J.M.A.
Project Administration: A.J.M.A.
Funding Acquisition: -