Introduction
Abnormal vertebral morphology is caused by defects in vertebral segmentation and/or vertebral development (1, 2). Since most of these abnormalities are asymptomatic, they may only emerge with age or upon the incidence of a trauma (3,4,5).
The most common cervical vertebral anomalies include fusion and posterior arch deficiency (PAD) (3). Although it is possible to observe cervical vertebral anomalies in healthy individuals with normal occlusion and normal craniofacial morphology, some studies have found an association between upper cervical vertebral malformations and cleft lip and palate (6), condylar hypoplasia (7), skeletal deep bite (8), skeletal mandibular overjet, and skeletal open bite (9).
Sonnesen noted the relationship between cervical column morphology and head and neck posture and disclosed that fusion is associated with head and neck posture (10). Significant correlations have also been reported between fusion and a large cranial base angle, fusion and retrognathia, and fusion and inclination of the jaws in patients with severe skeletal malocclusion (11). These findings indicate a relationship between cervical spine fusion and craniofacial morphology, including the cranial base (10).
Lateral cephalometric imaging is the most common form of radiography used in orthodontic clinics (12). It is primarily used to evaluate growth, development, and morphometric craniofacial and maxillomandibular relationships, dental structures, and cervical vertebrae morphology in order to assess skeletal maturity; however, this imaging technique can also be used to study various anomalies of the cervical vertebrae (4,12).
Considering the relationship between the cervical spine and head position and the relationship between head and craniofacial morphology, including the mandibular rotation pattern, we may deduce a relationship between cervical morphology and the vertical dimensions of the face (6). Since the nature of this relationship is not well understood, and due to the inadequate studies on this subject and the significance of the issue. There- fore this study aimed to assess the morphology and common anomalies of the cervical vertebrae in different skeletal classes and facial types. The present study used lateral cephalometric images as the most common modality in orthodontics to investigate the relationship between fusion and PAD as common cervical anomalies as well as the relationship of cervical vertebral morphology and cranial base angle with different facial types and skeletal classes. If there is a relationship between these factors, a closer examination of the spine in lateral cephalometry can be recommended for individuals with occlusal deviations in orthodontic treatment.
Materials and methods
The current cross-sectional study was approved by the Research Ethics Committee of Guilan University of Medical Sciences (IR.GUMS. REC.1400.532) and was conducted on 137 lateral cephalometric images. Informed consent was taken from the patients with regard to the use of their cephalometric data. Individuals aged 18-55 years with permanent teeth and good-quality images recording their C1 to C3 vertebrae were included. Those with a history of trauma to or surgery on the cervical vertebrae, craniofacial abnormalities, or musculoskeletal defects were excluded.
The patients were divided into three facial types based on the SN-MP angle: Hypodivergent (<26°), normodivergent (26-34°), and hyperdivergent (>34°). Based on the Wits analysis and the ANB angle, they were also divided into three skeletal classes (13). The cranial base angle was deter- mined by measuring the angle between nasion sella and sella basion.
The morphology of the cervical spine was determined by measuring the external anterior posterior diameter of C1, the height of the posterior arch of the atlas, and the dense angle (between the axis of the dense and the occlusal plane) (Figure 1). As for cervical spine anomalies, the two common cases of fusion (merging of one cervical vertebra with another and the lack of radiolucency on these surfaces) and PAD (cases with a posterior atlas arch length of <4 mm) were examined (10, 13) (Figure 2).
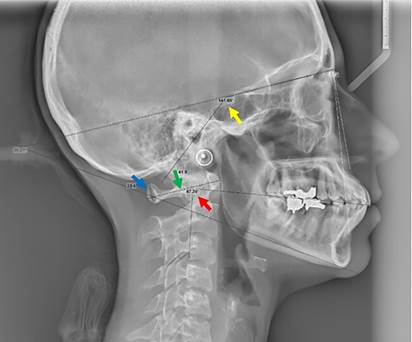
Figure 1 Analysis of the lateral cephalometric image and measurement of study parameters. Cranial base angle (yellow arrow), the height of the posterior arch of the atlas (blue arrow), the external anterior posterior diameter of the atlas (green arrow), the dense angle (red arrow).

Figure 2 A. Fusion of C2 and C3 vertebrae (white asterisk*). B. Posterior arch deficiency (PAD) (black asterisk*).
All lateral cephalometric images were taken by a calibrated Planmeca Scara III (Helsinki, Finland) with the patient's Frankfurt plane parallel to the ground. Exposure conditions differed according to each patient's condition. Observations and measurements were made in Scanora 5 on a 22-inch monitor by a maxillofacial radiologist. To ensure diagnosis reliability, ten samples were re-examined at a seven-day interval and agreement about the diagnosis was ensured based on Kappa’s coefficient (0.82). The minimum acceptable value was 70%.
Statistical analysis
Descriptive statistics including mean and standard deviation and frequency and percentage were used to describe the data. The normality of the data was assessed using the Shapiro-Wilk test, and the homogeneity of the variance in the study groups was evaluated using Levene's test. To analyze the data, if the assumptions were held, the independent t-test and analysis of variance (ANOVA) (with Tukey's pairwise comparisons) were used for the quantitative variables; if the assumptions were violated, the Kruskal-Wallis test and Spearman’s correlation test were used. As for the qualitative variables, the Chi-square test was used if the assumptions were held, and Fisher's exact test was performed if they were not held. These calculations were performed in SPSS 22 (SPSS, Inc., Chicago, IL, USA) at the significance level of P<0.05.
Results
The lateral cephalometric images of 137 patients with a mean age of 22.59±8.53 years were examined, including 99 (72.3%) female and 38 (27.7%) male patients.
Of the 137 patients studied, 33 had cervical vertebral anomalies, including 22 with fusion, ten with PAD, and one person with both. The mean values of cervical vertebral morphology were 7.73±1.94 and 43.69±3.47 mm for the posterior arch height of the atlas and the external anterior posterior diameter of C1, respectively, and the mean dense angle was 86.10±9.38°.
In the studied samples, 15 (10.9%) were hypodivergent, 60 (43.8%) normodivergent, and 62 (45.3%) hyperdivergent.
As for the distribution of skeletal class among the patients, 67 (48.9%) belonged to class I, 55 (40.1%) class II, and 15 (10.9%) class III.
The mean cranial base angle was 128.75±9.91, with a minimum and maximum of 83 and 188.50°.
Assessing the relationship of morphology with age and sex revealed a direct and significant relationship between the height of the posterior arch of the atlas and age (r=0.19, P=0.026); that is, the height of the posterior arch of the atlas increased with age. Moreover, a significant relationship was observed between the mean external anterior posterior diameter of C1 and sex (P<0.001), such that the mean value was higher in men (45.37±3.87) than in women (43.04±3.09). Nevertheless, there was no significant relations- hip between cervical vertebral anomalies and age (P=0.352) or sex (P=0.162).
Different facial skeletal classes did not show any significant relationship with age (P=0.863) or sex (P=0.277) either.
Table 1 presents the frequency of cervical vertebral anomalies for different facial types and skeletal classes, and no significant difference was observed in any of the cases (Table 1).
Table 2 presents the relationship between morphology, cranial base angle, and different facial types. As shown, the only significant difference was observed in the external anterior posterior diameter of C1; based on Tukey's pairwise comparisons, the hypodivergent group had a higher mean diameter than the other two groups (Table 2).
Table 3 demonstrates the relationship of morphology and cranial base angle with different facial skeletal classes, suggesting no significant relationships in any of the cases (Table 3).
Table 1 The relationship of cervical vertebral anomalies with different facial types and skeletal classes.
| Variable | - | - | Anomaly N (%) | - | - | P value* |
|---|---|---|---|---|---|---|
| - | - | No anomaly | Fusion | PAD | Fusion + PAD | - |
| Facial types | Hypodivergent | 14 (93.3) | 1 (6.7) | 0 (0) | 0 (0) | 0.100 |
| - | Normodivergent | 42 (70) | 15 (25) | 3 (5) | 0 (0) | - |
| - | Hyperdivergent | 48 (77.4) | 6 (9.7) | 7 (11.3) | 1 (1.6) | - |
| Skeletal classes | Cl I | 48 (71.6) | 13 (19.4) | 6 (9) | 0 (0) | 0.611 |
| - | Cl II | 45 (81.8) | 6 (10.9) | 3 (5.5) | 1 (1.8) | - |
| - | Cl III | 11 (73.3) | 3 (20) | 1 (6.7) | 0 (0) | - |
PAD: posterior arch deficiency; * Fisher's Exact Test.
Table 2 The relationship of cervical spine morphology and cranial base angle with different facial types.
| Variable | - | Hypodivergent Mean±SD | Normodivergent Mean±SD | Hyperdivergent Mean±SD | P value |
|---|---|---|---|---|---|
| Morphology | Height of post. arch of C1 (mm) | 8.19±2.16 | 7.99±1.90 | 7.36±1.90 | 0.129* |
| - | Lateral outer AP diameter of C1 (mm) | 46.83±3.46 | 43.37±2.91 | 43.23±3.63 | 0.001* |
| - | Dens angle (degree) | 82.98±6.55 | 84.83±8.56 | 88.09±10.37 | 0.062* |
| Cranial base angle | - | 121.93±16.82 | 129.41±9.95 | 129.76±6.74 | 0.133§ |
Post: posterior; AP: anterior posterior; SD: standard deviation; * ANOVA; § Kruslal Wallis.
Table 3 The relationship of cervical spine morphology and cranial base angle with skeletal classes.
| Variable | - | Cl I | Cl II | Cl III | P value* |
|---|---|---|---|---|---|
| Morphology | Height of post. arch of C1 (mm) | 7.65±2.20 | 7.79±1.53 | 7.86±2.21 | 0.902 |
| - | Lateral outer AP diameter of C1 (mm) | 43.91±3.65 | 43.31±3.31 | 44.10±3.33 | 0.675 |
| - | Dens angle (degree) | 85.74±9.80 | 85.100±8.85 | 88.11±9.74 | 0.571 |
| Cranial base angle | 129.23±9.88 | 127.98±10.36 | 129.39±8.71 | 0.763 |
Post: posterior; AP: anterior posterior; *ANOVA.
Discussion
Abnormal vertebral morphology is due to defects in segmentation or the development of the vertebrae (1). Many of these developmental abnormalities may be associated with another systemic disease and, since they are often asymptomatic, they may emerge only with age or upon the incidence of a trauma (3,4). The most common cervical vertebral anomalies include fusion and PAD. In the current study, the prevalence of fusion was 16.1% and the prevalence of PAD 7.3%, and the prevalence of their comorbidity was 0.7%. Meanwhile, in the study by Adisen SR et al., the highest prevalence of anomalies was related to PAD (22.5%) and the lowest to fusion (20.3%) (14). The rates reported by Kamak H. et al. were 8.1% for fusion and 5% for PAD (3), and those reported by Anusuya V. et al. were 28% for fusion and 36% for PAD (15), which are lower and higher than the prevalence rates reported in the present study, respectively.
The present study found no significant difference between cervical vertebral anomalies and age and sex. Although these results are consistent with those reported by Kamak H. et al., who suggested the absence of a relationship between sex and anomalies (3), Anusuya et al. found a significant difference in the rate of different cervical spine anomalies in men and women in all three skeletal classes, such that the prevalence was higher in women and in older ages (15). This disparity could partly be due to the sample size, which was 293 in their study vs. 137 in the current study, and partly due to the studied population. Adisen SR et al. reported that, with age, the prevalence of fusion rises in women and the prevalence of PAD rises in men (14); this disparity in findings could be due to the differences in sample size, mean age, and studied population.
Among the studied factors, the height of the posterior arch of the atlas was directly and significantly associated with age and increased with it. Furthermore, the mean external anterior posterior diameter of the atlas was higher in men than women. No correlation was observed between the other morphological factors and age and sex.
The present study did not find any significant relationship between cervical spine anomalies and the different facial skeletal classes. The study by Kamak H. et al. (3) also found no relation- ship between these anomalies and dental malocclusion; however, Meibodi S.E. et al. (13) observed a significant difference in the prevalence of fusion between Cl I and Cl II as well as between Cl II and Cl III.
According to Watanabe M. et al. (16), the height of the posterior arch of the atlas was shorter in Cl II than in Cl III, while the present study did not find any relationship between cervical vertebral morphology and skeletal classes. This disparity can be attributed to the differences in measurement techniques (CBCT vs. lateral cephalometry) as well as differences in sample size (31 vs. 137). Furthermore, the study by Watanabe M. et al. was conducted only on women.
Similar to the present findings, Anusuya V. et al. (15) also found no association between cervical vertebral anomalies and different facial types.
In the present research, the mean external anterior posterior diameter of C1 was significantly higher in the hypodivergent group.
The mean skull base angle did not show any significant difference across the skeletal classes. Wilhelm B.M. et al. (17) also reported a similar cranial base growth in classes I and II.
Although in the study by Anshuka et al., hyperdivergent and hypodivergent individuals had larger and smaller cranial angles, respectively (6), the current study found no relationship between the cranial base angle and different facial types.
The discrepancies observed in the studies reveal the need for more detailed studies on this subject. The use of CBCT and the assessment of more anomalies in larger samples are recommended for ensuring more accurate results.
Limitation of this study was the lack of sufficient studies on the relationship between the morphology of the cervical spine and age, sex, and different facial types to assess the results this study with other race that this subject highlights the need for further studies on this subject.
Conclusions
Examining the morphology of the cervical spine showed that the height of the posterior arch of the atlas increases with age, and the external anterior posterior diameter of the atlas was larger in men and in hypodivergent individuals. Due to the inadequacy of studies on cervical anomalies in different skeletal classes and facial types, further research is recommended on this subject. If the relationship between cervical spine anomalies and morphology and different skeletal classes is confirmed on a large scale, the routine examination of the spine could be suggested for occlusal deviations in orthodontic treatments.
Author contribution statement
Conceptualization and design: F.O., M.F. and R.R.
Literature review: Z.Y.
Methodology and validation: F.O., M.F., Z.Y., M.T., F.P. and R.R.
Formal analysis: I.C. and L.T.
Investigation and data collection: Z.T., M.T. and F.P.
Resources: I.C.
Data analysis and interpretation: Z.T. and R.R.
Writing-original draft preparation: F.O., M.F., Z.Y., and R.R.
Writing-review & editing: Z.T., M.T. and F.P.
Supervision: L.T.
Project administration: L.T.















