Introduction
A respiratory disease, also known as the COVID-19, has turned into a pandemic that has rapidly spread around the world.
The latest figures from early December 2021 show more than 270 million cases and over 5.32 million deaths officially reported worldwide (Hopkins, 2021; Worldometer, 2021). Infections with the COVID-19 virus have been detected in every human group or gender. However, men are more likely to be affected than women, being this more lethal for the elderly and those with previous health conditions, including obesity, hypertension, cancer, diabetes, or any other pulmonary or cardiac preconditions (Adams et al., 2020; Zhang et al., 2021; Jinjarak et al., 2020). The predominant transmission of the virus and its new variants is through exposure to respiratory droplets and aerosols that can be projected at different distances (Wang et al., 2021). Such aerosols and droplets appear with an estimated diameter of 5 to 10 micrometers (µm), and also through droplet nuclei, whose diameter is less than 5 micrometer (OMS, 2014; Smieszek et al., 2019). Social, cultural, or environmental circumstances have been responsible for the unusual higher spreading of the virus (Chakraborty et al., 2020; Sharifi et al., 2020; Roberto et al., 2020; Wolf et al., 2020; Lakshmi et al., 2020; Toulkeridis et al., 2020; Toulkeridis et al., 2021). Patient zero is still unknown, but the first appearance of the virus originated from China, either by an indirect contagion from a bat through an unknown mammal to a human or less likely by a laboratory leak presumably by the end of 2019 (Rothan et al., 2020; Zhang et al., 2020; Shahzad et al., 2020; Shi et al., 2021). As such circumstances are still unclear and, as not all infected persons show the mildest symptoms, therefore, the real count of infected and even deceased people has been a challenge for authorities, planning officials, the health sector, and response organizations (Galaitsi et al., 2021; Khan et al., 2021). Based on official accounts, South America represents only 5.5% of the world population but register 25.6% of the deceased and some 18.1% of the infected patients by the COVID-19 (Hopkins, 2021; Worldometer, 2021). Therefore, in the current study, we have chosen to approach to encounter the most real number of infected and deceased people in an area where, on the one hand, the original circumstances are already challenging, such as failing or unfunded health sector, social and political crisis prior to and during the pandemic and, on the other hand, a general long-lasting economic crisis is present, as occurring since several years in Ecuador (Ortiz-Prado & Fernández-Naranjo, 2020). We may be able to bring some transparency on the official rates of excess mortality based on the regular mortality rates, even if not labeled as demise by COVID-19 by a simple data analysis of the death rates.
Data and Methods
The official patient zero of COVID-19 appeared in Ecuador in February 2020. This first patient arrived from Italy and most likely has been responsible for contagions in the Province of Guayas, prior to several more outbreaks in the city of Guayaquil and a variety of further towns. As patient treatment within families and later in hospitals, as well as handling of health security, remained initially unknown to the corresponding treating personnel, the contagion and death rate rose, and based on similar worldwide circumstances, Ecuador´s governmental authorities closed its borders and declared a strict lockdown by March 16, 2020, which lasted some two months (Garzon-Chavez et al., 2021). Prior to such declaration, Ecuador had been already in a delicate economic situation due to a low oil price, fatal policies, as well as consequences of a variety of past natural disasters areas (Anderson et al., 2016; Jin et al., 2016; Toulkeridis et al., 2017; Toulkeridis et al., 2016; Toulkeridis et al., 2015; Toulkeridis et al., 2016; Rodriguez et al., 2017; Wolff et al., 2018; Hidrobo et al., 2019; Schodt et al., 2019; Beyers et al., 2020). Since, a variety of outbreaks created a first hot spot and rapid contamination of a high number of people with a corresponding high death rate in Guayaquil and the province of Guayas due to social and political circumstances.
All fatalities of all kinds of origins have been registered in Ecuador by its National Institute of Statistics and Census (INEC) for a few years on a daily basis (Instituto Nacional de Estadistica y Censo, 2021). Data of the ministry of health of all registered cases of COVID-19, either of contagion or deaths by the virus, are transmitted to the presidency, the press, and the official accountants of diseases such as the John Hopkins Research Center, besides several others. The data of all fatalities, including the official deceased patients of COVID-19, are listed in Table 1. Hereby, the average mortality for 26 months prior to the first case of COVID-19 (January 2018-February 2020) is about 6083.4±234.6 persons (Table 1).
Table 1 Ecuador’s total mortality rates between 2018 and 2021 based on Instituto Nacional de Estadística y Censos. 2021.
| 2018 | 2019 | 2020 | 2021 | |
| January | 6696 | 6706 | 6699 | 8454 |
| February | 5751 | 5930 | 6057 | 7652 |
| March | 6057 | 6570 | 10030 | 10241 |
| April | 5778 | 6159 | 20977 | 11976 |
| May | 5883 | 5960 | 10111 | 10340 |
| June | 5758 | 5891 | 8997 | 7660 |
| July | 5977 | 6078 | 10845 | 7301 |
| August | 6104 | 6245 | 10055 | 6560 |
| September | 5814 | 6194 | 7991 | 6124 |
| October | 5938 | 5976 | 7557 | 5971 |
| November | 5799 | 6010 | 7321 | 6137 |
| December | 6427 | 5712 | 7137 | T.B.D. |
| Total | 71982 | 73431 | 113777 | 76308 |
Note: derived from Instituto Nacional de Estadística y Censos. 2021.
Results and Discussion
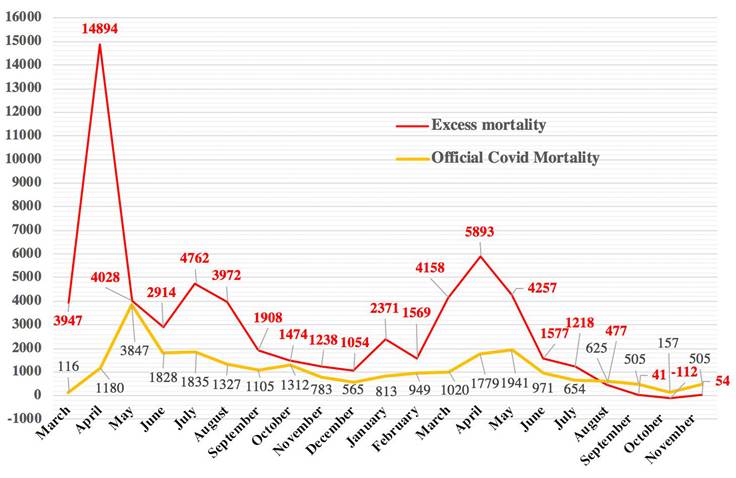
There has been a clear and long-lasting excess mortality in Ecuador since the beginning of the pandemic, which ends by the mid-end of 2021 (Table 1). The COVID-19 pandemic has started to alter the regular mortality rates, and an end is just recently observed, certainly due to vaccination that has begun in February of 2021. The occurrence of excess mortality frequently appears during usually short periods of time, such as in the aftermath of a strong earthquake, an outbreak of seasonal diseases, or other unusual but given circumstances like armed conflicts (Ansart et al., 2009; Vandoros et al., 2020; Luy., 2003; Wheatcroft et al., 1984; Walsh et al., 2017; De Waal et al., 1989). Although clear excess mortality has existed in Ecuador since the declaration of the pandemic, however, when calculating the average mortality rates prior to the pandemic and adding the official death rate by the COVID-19 virus, a high discrepancy exists (Table 2). When observing the reported fatalities of April 2020, the non-reported mortality numbers are eleven times higher than those of the official provided by the ministry of health. On average, during the entire period of the pandemic, there are some 300% excess mortality compared to the official COVID-19 mortality rate. There are exceptional months where excess mortality combined with the death toll by COVID-19 is within the average mortality rate, like for May and October of 2020, while mortality rates below the mentioned combined death toll are below average since August 2021, also interpreted as the end of the excess mortality in Ecuador.
Based on an average death toll of around 9,020 monthly (March 2020-November 2021), the excess mortality toll exceeds
Table 2 Excess mortality rates of Ecuador Data of February to November corresponding to 2020 and 2021 based on Hopkins, 2021; Worldometer, 2021; Instituto Nacional de Estadistica y Censo, 2021.
| Excess Mortality (EM) | Off. Covid Mortality (OCM) | EM and OCM (DEO) | ||||
| 2020 | 2021 | 2020 | 2021 | 2020 | 2021 | |
| January | N.A. | 2371 | N.A | 813 | N.A. | 1558 |
| February | N.A. | 1569 | N.A. | 949 | N.A. | 620 |
| March | 3947 | 4158 | 116 | 1020 | 3831 | 3138 |
| April | 14894 | 5893 | 1180 | 1779 | 13714 | 4114 |
| May | 4028 | 4257 | 3847 | 1941 | 181 | 2316 |
| June | 2914 | 1577 | 1828 | 971 | 1086 | 606 |
| July | 4762 | 1218 | 1835 | 654 | 2927 | 564 |
| August | 3972 | 477 | 1327 | 625 | 2645 | -148 |
| September | 1908 | 41 | 1105 | 505 | 803 | -464 |
| October | 1474 | -112 | 1312 | 157 | 162 | -269 |
| November | 1238 | 54 | 783 | 295 | 455 | -241 |
| December | 1054 | T.B.D. | 565 | T.B.D. | 489 | T.B.D. |
| Total | 61694 | 23607 | 38087 | |||
Note: derived from research.
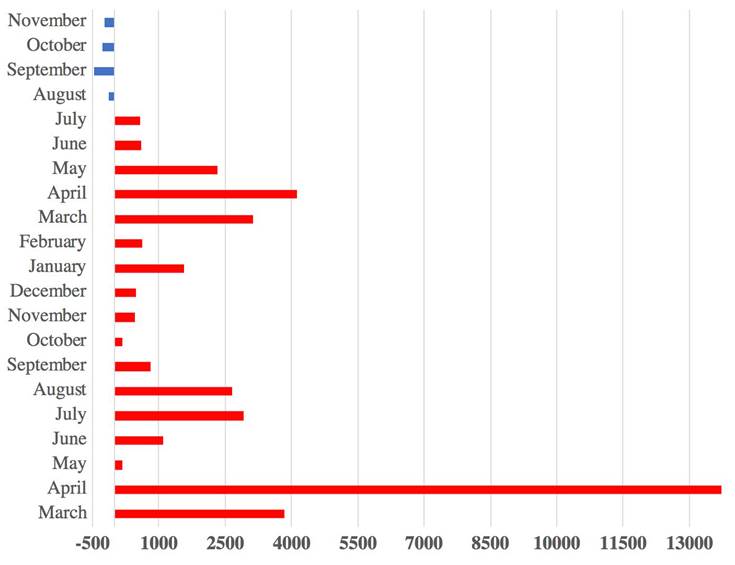
almost 62,000 persons, although the official numbers of deceased people by COVID-19 realized by the national ministry of health do not reach more than 23,607 victims. Therefore, we have observed that we lack an explanation of some 38,087 deceased who are not registered as COVID-19 victims until the end of September of 2021. The first explanations given by the ministry of health have been the lack of access of cancer patients to hospitals during the lockdown who died at home. But at the same time, fatal traffic accidents and work-related fatalities were not registered due to the same circumstances. Nonetheless, the most plausible explanation for such a high death toll is that most of the almost 62,000 deceased people, above the average death toll, have been victims by COVID-19.
If the excess mortality has reached almost 62,000 citizens from March 2020 to November 2021, while the official mortality by COVID-19 has been slightly more than 23,000 by the end of November 2021, then we assume that the contagion is also much higher than the officially stated, i.e., around 511,000 for the same period of time. When considering that in all official worldwide statistics there has been a contagion/mortality rate of 2.16% (by June 30, 2021), then, the calculated number of infected people in Ecuador will be of at least 2,833,000 citizens by the end of November 2021. This corresponds to more than 15.75% of the total population of the country. Additionally, based on these calculations of the excess mortality, the deaths per 1 million citizens would reach a rate of about 3434: this is just worldwide lower only to one country being Peru with 5950 (Fig. 1) (Hopkins, 2021; Worldometer, 2021). Based on such calculations and the aforementioned circumstances of different ways of contagion, it is a matter of simple arithmetic prior to a successful nationwide vaccination to preview that the health of the entire country’s population will be compromised in a variety of degrees.
Note: derived from research.
Figure 1 Comparison of official COVID Mortality (OCM) and excess mortality (EM) in Ecuador from February 2020 up to November 2021.
As it seems, South America is a hot spot of deaths by the COVID-19, based on fatal interpretations, premature, late or not given political decisions, lack of governmental leadership, a long-lasting economic crisis, corruption in high social-economic levels, in combination to unfunded health services, late and slow vaccination, as well as predominantly undisciplined public during the pandemic (Patiño et al., 2020; Burki et al., 2020; Herrera et al., 2021; Ortega et al., 2020; Fonseca et al., 2020; Joathan et al., 2021; Cardona-Ospina et al., 2021). Based even on official statistics about contagion and fatalities of the COVID-19 pandemic, which, as demonstrated for the Ecuadorian case, are highly underrated, still, the outcoming numbers are of great concern. South America has a population of some 434 million people, which corresponds to only 5.5% of the world population, but the whole continent registers 25.6% of the deceased because of Covid, more than a fourth of the world fatalities. The contagion is reflected by an amount of almost 3.4 million which represents some 18.1% of the worldwide infected by the COVID-19 (Hopkins, 2021; Worldometer, 2021). It seems that Ecuador is passing the end of the third wave of contagion and corresponding fatalities (Fig. 1).
Based on the aforementioned, the most plausible recommendation to the authorities and the corresponding public would be an accelerated vaccination process, a strong and lasting lockdown, as well as an improvement of health facilities and services, prior to the impact of a fourth even deadlier wave due to new mutants such as the delta variation (Knack et al., 2020; Harvey et al., 2021;
Note: derived from research.
Figure 2 Unreported COVID-19 fatalities in Ecuador from February 2020 (lower part of the graphic) up to November 2021 (upper part of the graphic) based on table 2.
Sahoo et al., 2020). Such activities certainly need political leadership and strict control of the implementation, which may also have some more indirect benefits for the society and the environment (Pacheco et al., 2020; Ortiz-Prado et al., 2021; Zalakeviciute et al., 2020). Unfortunately, the recent political decisions point out contrarily towards more openings of businesses and academic institutions rather to a needed strong lockdown.
Conclusions
COVID-19, which is transmitted in a variety of forms, is a deadly virus with a death rate of some 2.16% in respect to the infected number of people.
Ecuador has been so far the second-strongest affected country worldwide by the global COVID-19 pandemic when counting deaths per million citizens based on the calculated excess mortality rates.
Based on the high impact of the COVID-19 in Ecuador, an accelerated vaccination process is needed with a simultaneous strong lockdown, rather than further openings of state institutions and private businesses.















