INTRODUCTION
The word “epulis” is a general term that refers to the hyperplasia occurring in the gingiva or in the alveolar mucosa. Epulis fissuratum is also referred to as denture granuloma, inflammatory fibrous hyperplasia, denture induced fibrous hyperplasia and denture-related hyperplasia (1,2,3). The epulis fissuratum is a pseudo tumor growth that represents 23% of benign maxillary tumors (3). Clinically, it is presented as a remarkable sessile lesion in the form of folds with a smooth surface and a normal or an erythematous overlying mucosa. The size of the lesion varies from localized hyperplasia of less than 1 cm to massive lesions covering most of the length of the vestibule. The presence of these lesions not only causes pain and discomfort but also affects the mastication, aesthetics and general well-being of the patient (4.5). Epulis fissuratum (EF) can be treated according to the lesion, in a conservative way with the tissue conditioning or surgical act. In addition to conventional techniques (classical surgery, electrocauterization), various types of lasers such as erbium, chromium: Garnet Yttrium Scandium-Gallium (er, CR: YSGG), CO2, neodyme: yttrium-aluminium-Garnet (ND: YAG), and diode lasers have become alternative techniques in the surgery of soft tissues (6). Adequate prosthetic rehabilitation is essential in both cases. The confection of an interim prosthesis or the rectification of the old prosthesis for the setting up of the tissue conditioner is necessary to improve healing and prevent the decrease of the vestibule depth and the formation of post-surgical exeresis scars. The purpose of this paper is to present an original technique for the modification of old prosthesis during the management of a clinical case presenting an epulis fissuratum.
CASE REPORT
A female patient aged about forty-five, in good health, attended the consultation at Rabat Dental Consultation and Treatment Center for the instability of her prosthesis, especially the mandibular one. During the interrogation, the patient stated that she had worn the prosthesis for five years without any prosthetic control, and that a mandibular tissue lesion appeared a year ago.
EXTRAORAL EXAMINATION
Revealed an ill-fitting denture with a reduced edge and a damaged porous biomaterial with braded prosthetic teeth which had a mandibular prognathism, a decrease of the vertical dimension of occlusion and a lack of labial support.
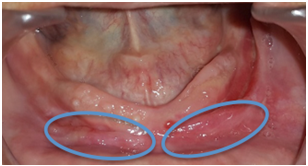
INTRAORAL EXAMINATION
It revealed the presence of prosthetic stomatitis in the maxilla, and an important hyperplasia with a size of 1cm x 6cm and sitting at the depth of the vestibule with an anterior floating ridge in the mandible. The hyperplasia was covered with an inflammatory mucosa, flexible on palpation and non-haemorrhagic (Fig.1). The examination of the old prosthesis showed the wear of the prosthetic teeth and the presence of the edges in under extension with respect to the hyperplasia. The reduced maxillary and mandibular prosthetic bases did not exploit the entire bearing surface. Examination of occlusion revealed a decrease in the vertical occlusal dimension, mandibular prognathism, and poorly distributed occlusal contacts.
THERAPEUTIC APPROACH
In front of this clinical situation, it was decided to start with the rectification of the old prosthesis before the surgery in order to put it in place the day of the surgery. This prosthesis will allow the setting up of a tissue conditioner to improve and guide the healing and also to avoid the introduction of a cicatricial flange. After optimal healing, adequate prosthetic rehabilitation was developed.
MODIFICATION OF OLD PROSTHESES
We started with the placement of a fluid alginate at the intaglio, next to the lesion and between the ridge and the lesion. Then, before the setting of the material, we took an alginate impression with a commercial tray with the prosthesis in place (Fig.2). The casting of the impression was carried out. On the model we eliminate the epulis fissuratum so as to simulate the final result obtained by the surgery. After the insulation of the model (Fig.3), we put the acrylic resin with a consistency neither too fluid nor harsh in the vestibule and the alveololingual groove and in the intaglio of the prosthesis after painting it with the monomer to improve the adhesion between the two resins (Fig.4). The areas of the intaglio that weren’t covered by the alginate during the impression, served as stops for the prosthesis and so facilitated its good repositioning on the model (Fig.5). After the polymerization, removal of excess and finishing of the prosthesis was performed (Fig.6).
SURGICAL PHASE
The excision of the epulis fissuratum was performed with conventional surgical excision. The depth of the vestibule was preserved. Healing was done by secondary intention (Fig.7).
PLACEMENT OF THE RECTIFIED PROSTHESIS
Immediately after the surgery, the mandibular prosthesis was filled with a tissue conditioner (FITT of Kerr®) and inserted into the mouth. The patient closed to the good vertical occlusal dimension and the good intermaxillary relationship which allowed the diminution of the mandibular prognathism, then she performed all functional movements. After polymerization, the mandibular prosthesis was removed, the prosthetic edge related to the site of the surgery was shaped manually in a normal form by adding tissue conditioning material, and the polymerization continued outside the oral cavity (Fig.8). This technique helps guide healing and promote a rounded vestibule bottom with a normal aspect.
POST-SURGICAL PROSTHETIC PHASE
After two months, the fibromucosa of the supporting surface has a physiological aspect (Fig.9).
So, the confection of the definitive complete denture was started according to the conventional sequences.
CONTROLS
A first control was scheduled one week later to assess the hygiene and healing of the wound, and to renew the tissue conditioning material and the prosthetic edge facing the epulis fissuratum is rounded by addition of tissue conditioning material, manually outside the patient's mouth. The second control at 15 days for the removal of the suture and to renew the tissue conditioning material. Then after 1 control every 15 days until complete healing was achieved. At two months after the surgery the healing is complete, the confection of the definitive complete denture was started according to the conventional sequences. One year after the patient has returned, no sign of inflammation or recurrence were noted (Fig.10,11).
DISCUSSION
The management of mucosal pathologies of prosthetic origin in complete denture cases varies according to the type of the lesion and its etiology. The epulis fissuratum is among the lesions most frequently encountered (7). It is in the form of a fibrous hyperplasia caused by the wearing of poorly adapted prosthesis. The persistence of the trauma at the level of this lesion can predispose the patient to carcinoma, and hence the interest of management. In addition to eliminating etiological factors, the treatment of epulis fissuratum involves either conservative treatment (tissue conditioning) or in most cases surgery associated with tissue conditioning (4,8,9). For our patient, a surgical treatment plan associated with tissue conditioning was proposed. We started with the rectification of her old prosthesis by our technique which allowed a fast management of the patient by avoiding the different stages of confection of an interim prosthesis. To guide and promote the healing we implemented a tissue conditioner type (FITT of Kerr®). After the surgery, the prosthesis was rebased in the mouth with tissue conditioning material. The prosthetic edge facing the epulis fissuratum was rounded by addition of tissue conditioning material, manually outside the patient's mouth. This technique helps guide healing and promote a rounded vestibule bottom with a physiological aspect. Also, the physicochemical properties of the tissue conditioner used ensure a harmonious distribution of the occlusal loads, improve the stability and the retention of the prosthesis by a maximum exploitation of the support surfaces. It also the establishment of the vertical occlusal dimension allow a neuro-musculo- articular conditioning, and easier integration of the new prosthesis (10,11). After healing, conventional prosthetic rehabilitation was established with a schedule for the control sessions.