Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Médica Costarricense
versão On-line ISSN 0001-6002versão impressa ISSN 0001-6012
Acta méd. costarric vol.58 no.2 San José Abr./Jun. 2016 Epub 01-Jun-2016
Articles
Clinical cases of uveitis, Hospital México, 2010-2013
1División de Inmunología, Servicio de Medicina Interna
2Servicio de Oftalmología, Hospital México, Caja Costarricense de Seguro Social.
The word “uvea” comes from the Latin and means grape according to the descriptions of the ancient anatomists since when the external tissue of the eye is taken away, what is left over is a structure which resembles a grape underneath its shell. The uvea is the middle layer of the eye whose anterior portion includes the iris and the ciliary body. The posterior portion of the uvea is highly vascularized and is known as the choroid. The concept of uveitis encompasses a wide and heterogeneous variety of acute, subacute and chronic inflammatory processes which affect any of the above-mentioned ocular structures.1,2
Nevertheless, the inflammatory reaction may compromise neighboring structures such as the vitreous body as well as the retina.3
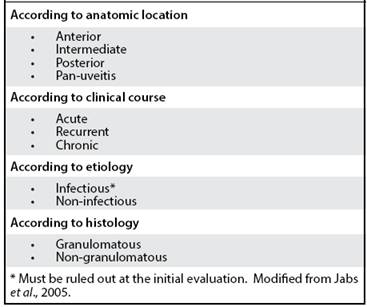
There are a variety of ways in which uveal disease may be classified, be it according to its anatomy, duration, presence or absence of granulomata, presence of infection or association with the expression of HLA B-27 alleles; the nomenclature that is used nowadays classifies uveitis according to the primary site of inflammation. The involvement of the anterior chamber of the eye is categorized as anterior uveitis and includes the different types of iritis and iridocyclitis. Involvement of the vitreous body is seen in intermediate uveitis and includes pars planitis. Posterior uveitis involves retinal or choroidal inflammation. Finally, the term panuveitis refers to a less-circumscribed inflammatory process.
According to the criteria of the SUN (which refers to the initials of the Standardization of Uveitis Nomenclature Study Group), the illness is also categorized according to the type of onset (abrupt or insidious), to the duration (limited or persistent) and finally, to its course (acute, recurrent or chronic; Table 1).4
The different etiologies of uveitis may be divided into four large groups: infectious causes, immunerelated systemic diseases, primary disorders of the eye and masked syndromes which may be associated with neoplasias such as B-cell lymphoma. Infectious causes include viruses (cytomegalovirus, herpesvirus), parasites (Toxoplasma gondii), bacteria (Mycobacterium tuberculosis, Treponema pallidum) and fungi (Aspergillus species, Candida species) and they each have distinctive clinical pictures and affect different populations.5
Uveitis may be part of the manifestations of systemic diseases such as ankylosing spondylitis, reactive arthritis, Behcet´s disease, Vogt-Koyanagi-Harada (VKH) syndrome, systemic lupus erythematosus, idiopathic juvenile arthritis or inflammatory bowel disease. In these cases, the uveitis is caused by auto-immune mechanisms which involve Th1 and Th17 lymphocytes as well as na increase in cytokine production, for example interferon gamma (IFN gamma), interleukin 17 (IL-17) and IL-23 all of which are related to the establishment of a type of dysregulation of the pathways that maintain immune tolerance such as, for example, regulatory T lymphocyes.
All of the above phenomena may be triggered by trauma, a cross-reaction against viral antigens or molecular mimicry and it all results in an increase in auto-reactivity.6
Certain manifestations of uveitis are characterized by the expression of specific human leukocyte antigens (HLA), among these HLA -B27 (in inflammatory bowel disease), HLA DR4 (in rheumatoid arthritis), HLA-DR1 (seen in VKH syndrome among the Hispanic population) and HLA B51 (in Behcet´s disease). Among the causes of uveitis which are limited to the eye we can mention pars planitis, sympathetic ophthalmia and chorioretinopathy in the form of pellets.7
Uveitis has an incidence of between 17 and 52 per 100,000 people in Europe and the United States of America even though a higher incidence is seen among persons of Chinese and Japanese ancestry.8 Uveitis is the fifth most common cause of visual disturbance and blindness in the United States and represents approximately 10 to 15% of the cases of blindness.9
Worldwide prevalence of uveitis may vary according to factors such as geographic location, age of the study population, academic center carrying out the study as well as time period of the study.10
The age group with the greatest incidence of this disease is that between 20 and 50 years with a predominance of anterior uveitis. Among the Japanese population, on the other hand, posterior uveitis predominates and this is associated with Behcet´s disease or VKH. Regarding the anatomic classification of the illness, anterior uveitis is responsible for, at least, half of the cases reported in Western countries, of which approximately 50% is of unknown origin. In the latter regions, the most common clinical associations are linked to HLA-B27 positivity such as ankylosing spondylitis and Fuchs´ heterochromic iridoyclitis. It is considered that more than 55% of Caucasian patients with acute anterior uveitis is HLA-B27 positive.8,11
Intermediate uveitis is the less common form of this illness in all regions and has an important relationship with type I human lymphotrophic virus as well as with multiple sclerosis.12 Posterior uveitis encompasses 15% to 30% of the diagnoses and the most frequent cause at a worldwide level is toxoplasmosis followed by idiopathic disease.11 The posterior location is most frequent in developing countries.13 Behcet´s disease and the VKH syndrome are rare entities but they are relevant in posterior uveitis mainly in Asiatic populations; uveitis in Behcet´s disease is common in the Middle East since it follows the course of the historic Silk Route.14,15
The prevalence of panuveitis is extremely variable and depends largely on geographic location; the most common cause in the developed world is the idiopathic one and in the developing world, that of infectious causes.3
General clinical manifestations of uveitis are: nonspecific ocular symptoms, reduction in visual acuity, photophobia, red-eye, ocular pain and the presence of “floaters” (myodesopsia).
Anterior uveitis, one of the most frequent types, has some characteristics which help to distinguish it from other causes of red eye, such as the absence of secretion and of pruritus, erythema predominantly in the junction of the cornea with the sclera (limbus) as well as a slow and painful pupillary reactivity and, finally, a family history of uveitis.
Visual impediment is a common symptom that affects between 2.8% and 10% of the patients and may result directly from the lesion of the uveal structures or may occur as a result of secondary effects on neighboring tissues: for example, accelerated formation of cataracts, glaucoma and macular edema.3
The differential diagnosis of the uveitides has changed over time. Syphilis and tuberculosis, which constituted in the past the main causes of uveitis, are diagnosed at the present time, in only 2.4% of the patients; nevertheless, a re-emergence of these pathologies has been noticed by some.16,17 Among the factors which have participated in the change in pattern of the uveitides, are: the increase in auto-immune diseases, the emergence of more infectious entities, the description of new pathologies, the advances in diagnostic methods and the improvement in the definition of the cases.18 Such differential diagnosis includes other causes of red eye: keratitis, conjunctivitis, episcleritis, scleritis as well as acute open-angle glaucoma.5
The management of uveitis depends on the origin of the pathologic process responsible as well as on the degree of ocular compromise. The majority of the uveitides diagnosed in Western countries are of a noninfectious nature and appear to have an auto-immune or auto-inflammatory origin, so that they require an anti-inflammatory or immunosuppressive treatment.3
When there is a clinical suspicion of uveitis, the patient should be referred on an emergency basis to a specialist in ophthalmology. In the majority of cases, topical anti-inflammatory treatment in the form of specific eye drops with steroidal and non-steroidal drugs may be used but in many patients, a more aggressive pharmacological intervention is needed such as systemic immuno-suppressants like glucocorticoids.
Among the immuno-modulatory drugs that may be used in uveitis, we have: anti-metabolites such as methotrexate, azathioprine and mycophenolate mofetil; calcineurin inhibitors such as cyclosporine and tacrolimus; alkylating agents such as cyclophosphamide and chlorambucil and biological agents which modify the immune response such as specific monoclonal antibodies and gamma-globulin.20-22
Even though the treatment of choice for the acute crises and the exacerbations of uveitis is that of corticosteroids, the therapeutic goal is to be able to attain as well as to maintain a steroid-free remission, a situation which can be reached with some of the chemotherapeutic agents mentioned above.23 The steroid-sparing immunosuppressive agents should be initiated as soon as the acute episode has been controlled. Chronic administration of corticosteroids is not an acceptable plan for the long-term treatment of the uveitides, unless all other pharmacological options have failed.2,24
The therapies that are available are effective in the treatment of a large spectrum of uveitides, but they are frequently associated with serious side effects. Current research is centered on promising immuno-modulatory strategies based on the blockade of effector pathways, co-stimulatory molecules as well as cytokines and their receptors.25
In the Hospital Mexico of the Costa Rican Social Security System, a Uveitis Clinic was established in 2009 where an ophthalmolgist and an immunologist participate in patient evaluation. This Clinic receives the referrals of patients with recurrent or severe uveitis which are sent by other specialists in the Ophtalmology Service.
The main objective of this paper was to characterize the referrals to the Uveitis Clinic in a sample of Costa Rican patients as well as to analyze their presentation, the types of inflammation (granulomatous or nongranulomatous) that they had as well as to observe the relationship between uveitis and systemic disease.
Methods
This retrospective study consisted of the registration and analysis of all cases referred to the Uveitis Clinic of the Hospital México during the period comprised between January the 1st., 2010 and September the 30th., 2013. This included information about a total of 58 patients. There were no cases excluded among all those that were referred to the Clinic.
The study had the approval of the Ethics Committee of the Center for Strategic Information and Development in Health and Social Security of the C.C.S.S. Patient data were obtained from the respective clinical charts and the cases were classified in accordance with the criteria of the Standardization of Uveitis Nomenclature Study Group. 4 The following information was recorded: age, sex, nationality or citizenship, place of origin including province in Costa Rica, date of initiation of symptoms, date of first consultation to the Uveitis Clinic, initial manifestations of the illness, classification of the pathology according to affected eye, anatomical location of the lesions, clinical course and presence or absence of granulomata, most likely presumptive diagnosis according to the clinical findings, type of treatment as well as co-morbidities.
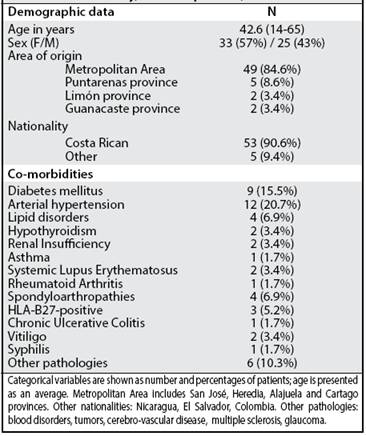
Table 2 Characteristics of the patients and concomitant illnesses. Uveitis Clinic, Hospital México, January, 2010 - September, 2013
Even though the description of the ophthalmologic findings documented in each case is beyond the scope of this report, we indicate herein the most important details of the ocular exam carried out in a systematic manner in each patient, during the consultation at the Uveitis Clinic. The criteria for activity and progress of the illness that were taken into account in the diagnoses, were: presence of the “flare” effect, cells as well as corneal and vitreous precipitates. Besides, the characteristics of the cornea were documented as well as those of the anterior chamber of the eye, the vitreous body and the retina (fundoscopy) all of the above by using a slitlamp.
The intraocular pressure was determined with Schlotz indentation tonometry and the visual acuity was determined objectively by means of the Snellen chart. Statistical calculations were performed using the PRISM GraphPad software (GraphPad Software Inc., San Diego, U.S.A.
Results
Table 2 summarizes the basic traits of the patients included in the study and their associated illnesses.
On average, 14 new cases were referred per year to the Uveitis Clinic of the Hospital Mexico and these cases mainly came from the Metropolitan Area of the capital city (84.6%). There were more female patients than male patients (57 percent versus 43 percent, male to female ratio of 1:1.32
The median age of the patients was 42.6 years and the range went from 14 to 65. Most frequent co-morbidities found in the patients were: arterial hypertension, diabetes mellitus and lipid disorders.
Table 3 Classification by anatomic site and clinical course of the uveitides. Uveitis Clinic, Hospital México; January, 2010 - September, 2013
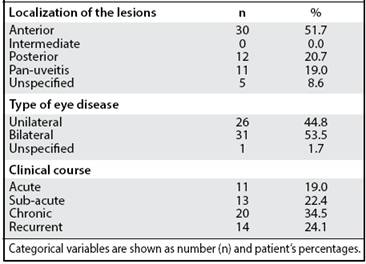
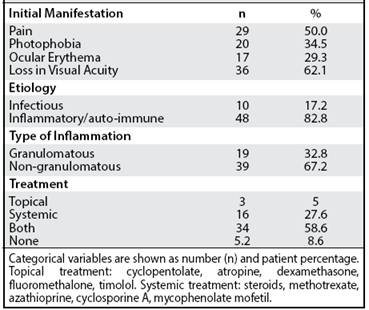
Table 4 Initial Clinical Manifestion of the uveitides, etiologies and treatments administered. Uveitis Clinic, Hospital México; January, 2010 - September, 2013
Greater than half of the cases had a bilateral eye disorder (53.5%) and in the majority of the patients (51.7%), the relevant diagnosis was anterior uveitis.
During the whole period of study, there were no cases documented of intermediate uveitis. A full 20.7% of the patients had posterior uveitis and, on the other hand, 19% had panuveitis (Table 3). The illness showed, predominantly, a chronic course of greater than 6 weeks (34.5%). The most frequent symptom at initial presentation was loss of visual acuity followed by ocular pain (Table 4).
In the majority of cases, it was not possible to establish an etiologic diagnosis. Regarding the type of inflammation, only 19 (32.8%) of the cases had a granulomatous uveitis, usually a likely VKH syndrome seen in 15 cases. One of the cases of granulomatous uveitis had sarcoidosis. Four cases were spondyloarthropaties and all were attributed to a systemic, auto-immune inflammatory process: three of these had HLA-B27 positivity, two cases were in association with systemic lupus erythematosus, one case had rheumatoid arthritis and one case was linked to inflammatory bowel disease.
Regarding infectious causes, the diagnosis was done according to each case, on the basis of serologies showing the presence of an early humoral response (presence of any titre of specific IgM) for toxoplasma or virus or a detectable viral load in the context of a contrasting ocular clinical pattern or, finally, a VDRL greater than 1:4 dilutions as well as a positive FTA. Practically, all of the infectious origin cases were attributable to ocular toxoplasmosis (8 patients, 13.8%) and they typically showed posterior or pan-ocular disease. As a specific detail, three of the patients with uveitis due to toxoplasma presented at the same time with infection with cytomegalovirus; two of these cases were in immunosuppressive treatment after , respectively, hematopoietic stem-cell transplantation and renal transplant; one of the cases, in addition, showed an association with multiple sclerosis. Only in one case was syphilitic uveitis detected.
A total of 50 patients (86.2%) required some type of systemic immuno-suppressive therapy, usually oral prednisone (47 patients or 81.0%). Systemic steroid therapy was given for the most part in combination with other immuno-modulatory and topical treatments (Table 4). Other immuno-suppressive drugs that were used were: azathioprine (17 patients or 29.3%), cyclosporine A (15 patients or 25.9%), methotrexate (7 patients, 12.1%) and mycophenolate mofetil (one patient, 1.7%). The five patients who did not receive treatment were asymptomatic cases without an active uveitis at the moment of ophthalmologic evaluation in the Uveitis Clinic.
Discussion
The majority of the research into uveitis is done in tertiary-care, referral centers with very little data coming from clinical, community practice so that what is primarily reported is severe illness with only a statistically small representation of those cases which are not severe.26 Besides, given the heterogenetiy in the uveal entities plus their extensive geographic variation regarding clinical manifestations as well as etiology, it is very difficult to carry out a comparison among regions. As a result of the rarity of this condition, it is frequently seen that uveitides are under-diagnosed and the associations between uveitis and extra-ocular manifestations of the illness are not well-understood.18
In Costa Rica, we do not know the incidence of this pathology and the present report is the first one of its type to be published.
The results of this study allowed us to confirm that, indeed, the most-affected group in this series of cases was that of young adults with an average age of presentation at the time of diagnosis of 42.6 years. In other words, uveitis primarily affects the economicallyactive population.
The relative frequencies of the uveitides, according to the anatomical location of the lesions, are comparable to data published in Central European tertiary-referral centers in which anterior uveitis has been reported in greater than half of the patients; on the other hand, our results differ from the registry in Nordic countries where the same condition is reported as causing almost the totality of the cases.28,29
In general, the largest diagnostic group was comprised of patients with ocular syndromes of unknown etiology followed by granulomatous pathologies, infections and, finally, non-infectious systemic illnesses all of which is consistent with large series of clinical cases from the Western world.18,27
Even though the Uveitis Clinic of Hospital México has as its goal the detection and treatment, exclusively, of uveal pathologies with an immunologic origin, during the study period some patients were referred to us that had an uveitis which was incorrectly diagnosed at the beginning of its evolution, as of unknown origin but in which, later, an infectious etiology was confirmed. In the group of patients analyzed in this study, the incidence of an infectious origin was similar to that in industrialized countries (17.2%) and the most-common infectious cause was toxoplasmosis, in concordance with international registries. Infectious uveitides are relatively rare in developed countries and are responsible for between 13 and 21 % of cases, mainly of a herpetic origin. 11On the contrary, in developing countries, it is estimated that more than 50% of uveitides are of an infectious nature.
In these populations, the most-common infectious causes are: toxoplasmosis, tuberculosis, onchocercosis, cysticercosis, leprosy and leptospirosis.13
Looking at the totality of the patients, the most important specific entities that were diagnosed are: VKH illness, ocular toxoplasmosis, and the presence of HLA-B27 positivity with or without systemic manifestations. Other publications have previously reported an elevated prevalence of the VKH syndrome in Latin America.30 This pathology consists of a sytemic, auto-immune disorder which leads to a T-cell-mediated granulomatous uveitis. The disorder affects organs with large concentrations of melanocytes, including the eye, the central nervous system, the internal ear and the skin.31 Recent studies have identified multiple genetic factors which may be associated with its pathogenesis including genes which express HLA, complement factor H, interleukins, NK cell receptors (killer cell immunoglobulin-like receptors, KIR) and molecules which inhibit T lymphocytes (for example, cytotoxic T-lymphocyte antigen 4, CTLA-4 and programmed cell death I, PD1) among many other factors.32 The illness is classically of a greater prevalence among women while in male patients there is an elevated risk of chorio-retinal degeneration and a worse prognosis. In women, the cyclical changes in estrogen and progesterone as well as the elevated levels of transforming growth factor beta (TGF), exert a protective role. The potential causes of the predilection of this illness for the female sex are related to HLA-DR and HLA-DQ alleles.33,34 In Costa Rica, this pathology is diagnosed on the basis of a high clinical suspicion since there doesn´t exist the possibility of performing specialized studies in this respect.
The high percentage of uveitis in the context of systemic and infectious illness emphasizes the need for an inter-disciplinary type of management. Global statistics reveal that infectious agents are involved in the origin of the uveitides in a high percentage of cases.
These numbers imply that a correct classification may have a decisive impact on the success or failure of the treatment and that immuno-suppressive therapies should not be initiated before an infectious entity is excluded. Nevertheless, the diagnosis of certain etiologies cannot be applied in a generalized manner and requires intensive research which may generate unnecessary costs. For these reasons, the recommended diagnostic path consists of the early involvement on the part of ophthalmologists, immunologists, rheumatologists and specialists in infectious disease all with experience in uveitis, a path which may help to reinforce local as well as international management guidelines and also may influence in a positive manner, the course as well as the prognosis of the illness.
The treatment of uveitis represents a medical challenge of considerable difficulty. The large majority of patients in the study required pharmacological immunosuppression, principally with systemic steroids. Singledrug therapy with corticosteroids, in general, is considered inappropriate due to its unfavorable risk-profile as well as the poor benefit in the long-term prognosis. Steroidsparing therapy offers less complications and secondary effects and should be begun as soon as possible in the management of the uveitides.24
It is clear that the retrospective nature of this study and the reduced number of patients involved, limit to a large extent, its clinical and epidemiologic implications. Nevertheless, the results of this research offer a valid perspective regarding the main causes of uveitis in Costa Rica. We realize, in any case, that the clinical course of the patients as well as the impact of the therapy established in the Uveitis Clinic must be analyzed in greater depth, for example, in a prospective study.
More of this type of analysis is required in Costa Rica so as to establish the national casuistry and to guide our physicians in the early recognition of the semiologic aspects of this pathology.
Conflicts of interest: the authors have no conflicts of interest to report.
Acknowledgments: Our thanks to the Department of Medical Records of the Hospital México for their cooperation with the lending of the clinical charts of the patients and also to the Ophthalmology and Immunology Services of Hospital Mexico for their assistance during the conduction of this study.
Research done in the Immunology Division, Internal Medicine Service and the Ophthalmology Service, Hospital México, Costa Rican Social Security System (C.C.S.S.) Author´s affiliations: 1Division of Immunology, Internal Medicine Service; 2Ophthalmology Service, Hospital México, Costa Rican Social Security System; 3University of Costa Rica. rosasur@gmail.com
Referencias
1. Jabs DA, Busingye J. Approach to the diagnosis of the uveitides. Am J Ophthalmol. 2013;156:228-236. [ Links ]
2. Lee FF, Foster CS. Pharmacotherapy of uveitis. Expert Opin Pharmacother. 2010;11:1135-46. [ Links ]
3. Barry RJ, Nguyen QD, Lee RW, Murray PI, Denniston AK. Pharmacotherapy for uveitis: current management and emerging therapy. Clin Ophthalmol. 2014;8:1891-1911. [ Links ]
4. Jabs DA, Nussenblatt RB, Rosenbaum JT. Standardization of uveitis nomenclature for reporting clinical data. Results of the first International workshop. Standardization of Uveitis Nomenclature (SUN) Working Group. Am J Ophthalmol. 2005;140:509-16. [ Links ]
5. Hajj-Ali R, Lowder C, Mandell BF. Uveitis in the internist’s office: Are a patient’s eye symptoms serious? Cleveland Clin J Med. 2005;72:329-39. [ Links ]
6. Forrester JV, Klaska IP, Yu T, Kuffova L. Uveitis in Mouse and Man. Int Rev Immunol. 2013;32:76-96. [ Links ]
7. Wertheim MS, Mathers WD, Planck SJ, Martin TM, Suhler EB, Smith JR, et al. In vivo confocal microscopy of keratic precipitates. Arch Ophthalmol. 2004;122:1773-81. [ Links ]
8. Wakefiled D, Chang J. Epidemiology of uveitis. Int Ophthalmol Clin. 2005; 45:1-13. [ Links ]
9. Pan J, Kapur M, McCallun R. Noninfectious Immune-Mediated Uveitis and Ocular Inflamation. Curr Allergy Asthma Rep. 2014;14:409-17. [ Links ]
10. Clinical Approach to Uveitis. En: Moorthy RS, Rao PK, Read RW, Van Gelder RN , Vitale AT, Bodaghi B, Parrish CM (eds). Intraocular inflammation and uveítis 2011-2012, section 9. San Francisco (CA): American Academy of Ophthalmology. 2011:77-116. [ Links ]
11. Miserocchi E, Fogliato G, Modorati G, Bandello F. Review on the Worldwide epidemiology of uveitis. Eur J Ophthalmol. 2013;23:705-17. [ Links ]
12. Allegri P, Rissotto R, Herbort CP, Murialdo U. CNS diseases and uveitis. J Ophthalmic Vis Res. 2011;6:284-308. [ Links ]
13. London NJ, Rathinam SR, Cunningham ET Jr. The epidemiology of uveitis in developing countries. Int Ophthalmol Clin. 2010;50:1-17. [ Links ]
14. Ohguro N, Sonoda KH, Takeuchi M, Matsumura M, Mochizuki M. The 2009 prospective multi-center epidemiologic survey of uveitis in Japan. Jpn J Ophthalmol. 2012;56:432-35. [ Links ]
15. Tugal-Tutkun I. Behçet disease in the developing world. Int Ophthalmol Clin. 2010;50:87-98. [ Links ]
16. Chao JR, Khurana RN, Fawzi AA, Reddy HS, Rao NA. Syphilis: reemergence of an old adversary. Ophthalmology. 2006;113:2074-9. [ Links ]
17. Cimino L, Herbort CP, Aldiferi R, Salvarani C, Boiardi L. Tuberculous uveitis, a resurgent and underdiagnosed disease. Int Ophthalmol. 2009;29:67-74. [ Links ]
18. Barisani-Asenbauer T, Maca SM, Mejdoubi L, Emminger W, Machold K, Auer H. Uveitis- a rare disease often associated with systemic diseases and infectionsa systematic review of 2619 patients. Orphanet J Rare Dis. 2012;7:57. [ Links ]
19. Castiblanco C, Foster CS. Review of Systemic Immunosuppression for Autoimmune Uveitis. Ophthalmol Ther. 2014;3:17-36. [ Links ]
20. Larson T, Nussenblatt RB, Sen HN. Emerging drugs for uveitis. Expert Opin Emerg Drugs. 2011;16:309-22. [ Links ]
21. Leung TG, Thorne JE. Emerging drugs for the treatment of uveitis. Expert Opin Emerg Drugs. 2013;18:513-21. [ Links ]
22. Sánchez-Cano S, Callejas-Rubio JL, Ruiz-Villaverde R, Ríos-Fernández R, Ortego-Centeno N. Review article: Off-label uses of anti-TNF therapy in three frequent disorders: Behçet’s disease, sarcoidosis, and noninfectious uveitis. Mediators Inflamm. 2013;2013. 11 páginas. Recuperado el 6 de febrero de 2015. En En http://www.hindawi.com/journals/mi/2013/286857/ [ Links ]
23. LeHoang P. The gold standard of noninfectious uveitis: corticosteroids. Dev Ophthalmol. 2012;51:7-28. [ Links ]
24. Lee K, Bajwa A, Freitas-Neto CA, Metzinger JL, Wentworth BA, Foster CS . A comprehensive review and update on the non-biologic treatment of adult noninfectious uveitis: part I. Expert Opin Pharmacother. 2014;15:2141-54. [ Links ]
25. Papotto PH, Marengo EB, Sardinha LR, Goldberg AC, Rizzo LV. Immunotherapeutic strategies in autoimmune uveitis. Autoimmun Rev. 2014; 13:909-16. [ Links ]
26. McCannel CA, Holland GN, Helm CJ, Cornell PJ, Winston JV, Rimmer TG. Causes of uveitis in the general practice of ophthalmology. UCLA Community- Based Uveitis Study Group. Am J Ophthalmol. 1996;121:35-46. [ Links ]
27. Bodaghi B, Cassoux N, Wechsler B, Hannouche D, Fardeau C, Papo T, et al. Chronic severe uveitis: etiology and visual outcome in 927 patients from a single center. Medicine (Baltimore). 2001; 80:263-270. [ Links ]
28. Päivönsalo-Hietanen T, Tuominen J, Vaahtoranta-Lehtonen H, Saari KM. Incidence and prevalence of different uveitis entities in Finland. Acta Ophthalmol Scand. 1997;75:76-81. [ Links ]
29. Jakob E, Reuland MS, Mackensen F, Harsch N, Fleckenstein M, Lorenz HM, et al. Uveitis subtypes in a German interdisciplinary uveitis center - analysis of 1916 patients. J Rheumatol. 2009;36:127-36. [ Links ]
30. Liberman P, Gauro F, Berger O, Urzua CA. Causes of uveitis in a tertiary center in Chile: A cross-sectional retrospective review. Ocul Immunol Inflamm. 2014;1:1-7. [ Links ]
31. Sheriff F, Narayanan NS, Huttner AJ, Baehring JM. Vogt-Koyanagi- Harada syndrome: A novel case and brief review of focal neurologic presentations. Neurol Neuroimmunol Neuroinflamm. 2014;1:e49. 4 páginas. Recuperado el 6 de febrero de 2015. En En http://nn.neurology.org/content/1/4/e49.full.pdf+html [ Links ]
32. Ng JY, Luk FO, Lai TY, Pang CP. Influence of molecular genetics in Vogt- Koyanagi- Harada disease. J Ophthalmic Inflamm Infect. 2014;4:20. 12 páginas. Recuperado el 6 de febrero de 2015. En En http://www.joii-journal.com/content/pdf/s12348-014-0020-1.pdf [ Links ]
33. Read RW, Holland GN, Rao NA, Tabbara KF, Ohno S, Arellanes-Garcia L, et al. Revised diagnostic criteria for Vogt-Koyanagi-Harada disease: report of an international committee on nomenclature. Am J Ophthalmol. 2001;131(5):647-652. [ Links ]
34. Wang Y, Chan CC. Gender Differences in Vogt-Koyanagi-Harada disease and sympathetic ophthalmia. J Ophthalmol. 2014;2014:157803. 8 páginas. Recuperado el 6 de febrero de 2015. En En http://www.hindawi.com/journals/joph/2014/157803/ [ Links ]
Received: October 15, 2015; Accepted: February 18, 2016











 texto em
texto em