Introduction
The pandemic of the coronavirus (SARS- CoV-2), a virus that causes COVID-19 (acronym derived from CO-rona VI-rus D-isease and the year of identification-19) (1,2,3), directly impacted the provision of oral health care, as the virus can be easily found in saliva droplets and aerosols (4,5,6,7,8). Thus, according to the US Department of Labor's Occupational Safety and Health Administration (OSHA), dental activity has been considered high risk for the transmission of SARS-CoV-2 (6,9). To prevent the risk of transmission of pathogens, in addition to the personal protective equipment (PPE) already routinely used in routine dental care (lab coat, cap, procedural gloves, and protective eyewear), new PPE has been recommended by the World Organization (WHO) for use in procedures involving the generation of aerosols (4,6,8,9,10), and as an alternative to surgical masks, the use of facial respirators (eg the N95 model, which has 95% efficiency in filtering microorganisms) (6,11,12,13). This recommendation is justified because surgical masks have a poor marginal fit and/or peripheral sealing (11,14,15), while respirators have a better seal with the professional-respirator skin interface allowing them to minimize the entry of aerosols (14,15,16,17).
To provide the proper fit on the face, the elastic of respirators is tighter when compared to surgical masks and may generate greater discomfort and resistance when used by professionals, especially during long working hours (16,17). It should be noted that another important feature that can interfere with the adjustment of respirators is related to individual anatomical variations, such as the shape of the nose due to ethnic differences or the size of the face, in which women have a smaller face than men (15,18,19). Marginal peripherical sealing can be improved, when using ASTM surgical/medical masks, by using a 3D-printed custom-frame (14). The individualized fitting of this frame helps to concourse the anatomical difference between subjects.
Another relevant piece of data regarding the use of respirators was generated by the difficulty of acquiring or securing replacement supply during the Covid-19 pandemic (11,14,15,18). Currently, there is no more shortage of facial respirators, but it was noted that the reusing can interfere both with the adjustment of the elastics, caused by loosening due to repeated use, as well as with increased risks of contamination (18). Also, we may need to look for future alternatives in case of a similar epidemic of any infectious disease.
To help professionals during the shortage of respirators in the COVID -19 pandemic, a previous study evaluated the use of a custom frame produced using three-dimensional (3D) printing technology, in order to provide peripheral sealing of the ASTM level 3 and level 2 surgical/medical face masks (14). This study suggests that the use of a 3D-printed custom frame was found to achieve an effective peripheral seal that was comparable to N95 respirators. To date, no studies have been evaluated the acceptance of 3D-printed custom frames or any other peripherical sealing that enhance the use of ASTM surgical/medical masks. Thus, this study aimed to assess the acceptance of a 3D-printed custom-frame associated with the ASTM surgical/medical masks and the use of a face shield.
Material and methods
The present study was approved by the local Institutional Review Board (IRB# 5200280) and all participants signed an informed consent form.
Sample characterization
Dental professionals (faculty, residents, and students) and staff of a US School of Dentistry participated in the study. The inclusion criteria were male or female subjects, above 18 years old. The exclusion criteria were employees with any facial deformity that can affect the performance of the 3D-printed custom frame.
For dentists, ASTM level 3 and level 2 medical face masks were made available, which have a filtration level less than but close to the N95 respirator (14). The ASTM level 1 medical face masks were offered to administration personnel, as although it does not have the same filtering efficiency as respirators (14), these subjects do not deal directly with procedures that generate aerosols. In addition, a face shield was also made available to all the subjects. The study was assessed during COVID-19 high-spread. During this time, the school established policies for the use of personal protective equipment (PPE) following the guidance of the CDC. To respond to the questionnaire, participants chose the most used PPE following the policies. Moreover, all subjects during this time were tested and screened for COVID symptoms. According to their response, participants were divided into 4 groups: mask only (M), mask and frame (MF), mask and face shield (MFS), and all 3 personal protective equipment (MFFS).
Questionnaire on the acceptance of comfort related to ppe for the face
The questionnaire in the present study was developed, after a literature review on the main adverse events related to the use of PPE (20,21,22,23). The questionnaire consisted of multiple-choice questions, with answer options based on the Likert scale (rated from 1 as very good to 5 as very poor), and was divided into three sections. The first section presented questions related to demographic data, and PPE use (age, gender, professional activity, kind of PPE used, hours dedicated to activities using the PPE, and use or re-use of face shield). The professional activity was recorded to make sure that faculty, resident, and students were classified into their respective programs and clinical duties were marked directly. When staff boxes were marked, the administrative duties were marked as well. The second section had questions with items related to the acceptance of comfort while using the PPE (comfort, ability to perform the normally assigned intervention, quality of visual comfort, musculoskeletal tolerance, movement restriction, sensitivity to smell, breathing). Finally, the third section, events related to pain with the use of PPE (earache, headache) (Appendix 1). It is observed that the items related to the potential for reduction in visual quality were answered only for the group that used the face shield.
The questionnaire was made available on the Qualtrics platform (Provo, UT, USA). Participants received an invitation through the institutio- nal email of the college with a link to access the questionnaire. During the study, two follow-ups were sent to all the subjects within two weeks of interval. Data were collected anonymously and the time to complete the questionnaire was approximately five minutes.
Information about 3d-printed custom-frame
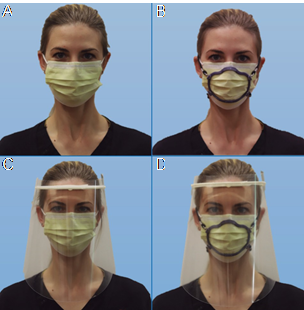
Initially, a scan of the participants' faces was performed using the software (Bellus3D FaceApp) on an iPad Pro (Apple) or iPhone11 or newer. The data acquired from the face of each participant generates a customized frame file using the Bellus Application design software and calculation generating a standard triangle language (STL) file and through RayWare software (version 2.7.0.13) transferred to the SprintRay Pro 95 3D printer, which uses digital light processing technology. 3D printing using resin materials Die and Model Gray, and Die and Model Tandall, at a wavelength of 405 nm (Ahmed et al., 2021) produces a customized 3D frame fitting only the scanned individual to overlay a medical mask. The frame consists of a single ring, which is adapted to the nasal and perioral region; featuring 4 side holes, 2 on each side, for placement of elastics to fit the users' head and neck. Details and specifications of the frame production are provided in a previous study (14). The printing time of each PPE was approximately 1.5 hours using the SprintRay Pro 95, at a cost of roughly $2.00 in resin material plus the cost of labor. Figure 1 illustrates the frame fitted to the commercial ASTM level 1, 2, 3 medical face mask (GCPYE, Crosstex) and the face shield used in the present study. The recommendation for cleaning/ disinfecting the frame and face shield followed the manufacturer's recommendation.
Results
A total of 1804 recipients got the questionnaire via email. From this, a total of 230 questionnaires were received, of which 24 were excluded for containing incomplete responses. Thus, the final analysis dataset included 206 questionnaires.
Most participants were 20 years old (33.5%), female (65.4%), mostly white (51%), followed by Asians (24.3%). It is observed that the proportion of participants was approximately equal to their functions, with the majority working in a clinical environment (77.2%) (Table 1).
Table 1 Demographic data of participants.
| Variables | - | N(%) |
|---|---|---|
| Age-Levels | 20-29 | 69 (33.5) |
| - | 30-39 | 41 (19.9) |
| - | 40-49 | 32 (15.5) |
| - | 50-59 | 25 (12.1) |
| - | 60-69 | 30 (14.6) |
| - | +70 | 9 (4.4) |
| Sex | Female | 134 (65.4) |
| - | Male | 72 (34.6) |
| Ethnicity | Asian | 50 (24.3) |
| - | Black or African American | 9 (4.4) |
| - | Hispanic or Latino | 41 (19.9) |
| - | Native Hawaiian or Other Pacific Islander | 1 (0.5) |
| - | White | 105 (51.0) |
| Position | Faculty | 53 (25.7) |
| - | Staff | 71 (34.5) |
| - | Student and Resident | 82 (39.8) |
| Primary area of duties | Administrative | 47 (22.8) |
| - | Clinical | 159 (77.2) |
Most participants used the ASTM Mask Level 2 type mask (54.9%) associated with the set: Mask+Frame+Face Shield (50.5%), with approximately similar frequency of use for Stock Face Shield (35.0%) and 3D Printed Custom Face Shield Frame (30.6%), working more than 4 hours a day (70.9%). Participants also reported reusing Face Shield (62.6%), more than 4 times (57.3%) (Table 2).
Regarding the acceptance of the PPEs on the MFFS group, the frequencies between the categories were grouped in ''very good''/''good'', ''neutral'' and ''poor''/''very poor'' (Table 3). The participants reported that ''comfort'' was ''poor''/''very poor'' (44.7%), but ''Ability to perform the assigned intervention as usual'' was ''very good''/''good'' (40.3%) (Table 3). ''Quality of visual comfort'' was ''poor''/''very poor'' (48.1%), with adequate tolerance, ''very good''/''good'' (38.8%) for ''ease of movement'' and ''very good''/''good'' (34.5%) for ''smell sensitivity'', but ''poor''/''very poor'' (44.7%) ''breathing'' (Table 3). ''Ear pain'' was reported as ''poor''/''very poor'' (38.9%), but ''headache'' was ''very good''/''good'' (48.1%) (Table 3).
The last table presents a comparison between the MFS and MFFS groups when used for more than 4 hours a day. The results showed a classification of ''neutral'' for all the effects of using the MFS, except for ''ease of movement'' and ''smell sensitivity'' which were classified as ''good to neutral'' and ''good'', respectively. Also, ''mild pain'' was registered on the ear and ''no pain'' on the head. When analyzing the effects of using the MFFS, it shows a classification of ''poor'' for all the items, except for ''Ability to perform the assigned intervention as usual'', ''Musculoskeletal tolerance, and ''smell sensitivity'' which were classified as ''neutral''. Finally, ''moderate pain'' was registered on the ear and head (Table 4).
Table 2 Personal protective equipment (PPE) used time of use and reuse of PPE, purpose of use of PPE.
| Questions | - | N(%) |
|---|---|---|
| Type of mask | ASTM Mask Level 1 | 45 (21.8) |
| - | ASTM Mask Level 2 | 113 (54.9) |
| - | ASTM Mask Level 3 | 34 (16.5) |
| - | N95 Mask | 14 (6.8) |
| Type of face protection equipment | Mask Only | 65 (31.1) |
| - | Mask + frame | 6 (2.9) |
| - | Mask + Face Shield | 32 (15.5) |
| - | Mask + Frame + Face Shield | 103 (50.5) |
| Time wearing facial PPE per day | 1hr | 1 (0.5) |
| - | 2hrs | 7 (3.4) |
| - | 3hrs | 24 (11.7) |
| - | 4hrs | 20 (9.6) |
| - | Less than 1 hr | 9 (4.5) |
| - | More than 4 hrs | 145 (70.4) |
| Face shield used | 3D Printed Custom Face Shield Frame | 63 (30.6) |
| - | No Face Shield | 71 (34.5) |
| - | Stock Face Shield | 72 (35.0) |
| Reuse your face shield | No | 77 (37.4) |
| Yes | 129 (62.6) | |
| Number of times reused face shield | 0 | 77 (36.9) |
| - | 1 | 2 (1.0) |
| - | 2 | 1 (0.5) |
| - | 3 | 5 (2.4) |
| - | 4 | 3 (1.5) |
| - | More than 4 | 118 (56.6) |
Table 3 Acceptance of the MMFS group.
| Questions | - | - | N (%) | - |
|---|---|---|---|---|
| Aspects of wearing your designated PPE | - | Very good/Good | Neutral | Poor/Very poor |
| - | Comfortable | 59 (28.6) | 54 (26.3) | 92 (44.7) |
| - | Ability to perform the assigned intervention as usual | 83 (40.3) | 59 (28.6) | 64 (31.1) |
| - | Quality of visual comfort | 56 (27.2) | 51 (24.8) | 99 (48.1) |
| - | Musculoskeletal tolerance | 69 (33.5) | 67 (32.5) | 70 (34.0) |
| - | Ease of movement | 80 (38.8) | 65 (31.6) | 61 (29.6) |
| - | Smell sensitivity | 71 (34.5) | 76 (36.9) | 59 (28.6) |
| - | Breathing | 56 (27.2) | 64 (31.1) | 86 (41.7) |
| - | - | No to minimal pain | Mild Pain | Moderate to Severe Pain |
| Effects experienced while wearing your designated PPE | Ear Pain | 78 (37.9) | 50 (24.3) | 78 (38.9) |
| - | Headache | 99 (48.1) | 50 (24.3) | 57 (27.7) |
Table 4 Effects related to the use of the PPE on the MFS and MFFS groups for more than 4 hours a day.
| Questions | - | More Than 4 hrs On The Group MFS N(%) | - | - | - | - | More Than 4 hrs On The Group MFFS N(%) | - | - | - | - |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Aspects of wearing your designated PPE | - | Very | Good | Neutral | Poor | Very poor | Very | Good | Neutral | Poor | Very poor |
| - | Comfortable | 3 (9.4) | 7 (21.7) | 9 (28.1) | 10 (31.3) | 3 (9.4) | 1 (0.9) | 15 (14.5) | 21 (20.9) | 42 (40.8) | 24 (22.6) |
| - | Ability to perform the assigned intervention as usual | 4 (12.5) | 9 (28.1) | 10 (31.3) | 5 (15.6) | 4 (12.5) | 0 (0) | 24 (22.6) | 29 (26.1) | 31 (27.9) | 18 (16.2) |
| - | Quality of visual comfort | 3 (9.4) | 8 (25) | 9 (28.1) | 7 (21.7) | 4 (12.5) | 0 | 10 (9) | 13 (11.7) | 53 (47.7) | 26 (23.4) |
| - | Musculoskeletal tolerance | 3 (9.4) | 7 (21.7) | 12 (37.5) | 5 (15.6) | 3 (9.4) | 4 (3.9) | 18 (16.2) | 29 (26.1) | 32 (28.8) | 18 (16.2) |
| - | Ease of movement | 3 (9.4) | 11 (34.4) | 11 (34.4) | 5 (15.6) | 2 (6.3) | 3 (2.7) | 25 (22.5) | 26 (23.4) | 34 (30.6) | 15 (14.5) |
| - | Smell sensitivity | 2 (6.3) | 10 (31.3) | 15 (46.9) | 4 (12.5) | 1 (3.1) | 6 (5.4) | 22 (19.8) | 35 (31.5) | 25 (22.5) | 15 (13.5) |
| - | Breathing | 1 (3.1) | 6 (18.8) | 14 (43.6) | 9 (28.1) | 2 (6.3) | 2 (1.8) | 17 (15.3) | 31 (27.9) | 34 (30.6) | 15 (13.5) |
| Effects experienced while wearing your designated PPE | - | No Pain | Minimal Pain | Mild Pain | Moderate Pain | Severe Pain | No Pain | Minimal Pain | Mild Pain | Moderate Pain | Severe Pain |
| - | Ear Pain | 6 (18.8) | 5 (15.6) | 11 (34.4) | 9 (28.1) | 1 (3.1) | 8 (7.2) | 13 (11.7) | 26 (23.4) | 36 (32.4) | 19 (17.1) |
| - | Headache | 10 (31.3) | 5 (15.6) | 8 (25.0) | 8 (25.0) | 1 (3.1) | 19 (17.1) | 15 (13.5) | 27 (24.3) | 31 (27.9) | 9 (8.1) |
Discussion
In the Covid-19 pandemic, the use of facial respirators has been advocated by health professionals in all aerosol-generating procedures (12,17). To ensure effective protection against respiratory viruses, such as the cause of Covid- 19, respirators must be well-fitted to the face, thus providing adequate sealing against aerosols (11,16,17,24). In this sense, the present study aimed to evaluate the acceptance of customized frames adapted to overlay readily available medical/surgical masks, which are more easily available among professionals (11,15), especially in moments of pandemic in which there was greater demand for respirators and lack of supply (11,14,15,18). Although supplies are not scarce anymore for N95's, peripheral seals could maybe be used by the general public.
The questions regarding the aspects and effects of the use of PPE were anteriorly used in similar studies (20,21,22,23). During the collection of the data, all the subjects were able to contact the researchers if there was any doubt in any of the questions of the questionnaire.
The results showed that the professionals had reasonable tolerance to the use of masks with the frame, as well as to the face shield set. Noted concerns of ear pain and headache ranging in degree, during prolonged use (>4 hours) not at the other times. It is important to highlight that the ASTM level 2 mask was the most used, as the participating professionals were involved with aerosol-generating procedures, which together with the ASTM level 3 are the surgical masks that are efficient in filtering close to the N95 respirator (14). In this sense, proper mask fit is essential to ensure adequate filtering and protection effectiveness (1,8,16). However, as in mouth breathers, the adjustment is achieved through more resistant elastics than the elastics of surgical masks, these mechanical and physical factors have resulted in pain and/or ear discomfort and headache among professionals. This is due to the pressure exerted by elastics on the soft tissues of the pericranial regions by prolonged use, exacerbating the nociceptive response transmitted to the superficial sensory nerves of the face, head, and cervical regions, especially the trigeminal or occipital nerve branches (16,24,25,26).
Thus, the discomfort caused by facial breathers can lead to a decrease in the professionals' ability to concentrate and perform during the consultations (16,19,24, 26), interference with adherence, especially for prolonged periods (16,17), need for adjustments during care or inappropriate use, generating risks of contamination (19).
In the present study, the frame's elastics were used to keep it positioned on the participants' faces, while the greatest adjustment occurred near the peri-oral and nasal region (Figure 1). It is important to highlight that in the region of greater adjustment, the adaptation was personalized, considering the individual facial characteristics of each professional, which may be one of the factors associated with the least discomfort reported by the professionals. An important characteristic of the sample in the present study was the greater participation of women and also professionals of different ethnicities, indicating that the proper fit of the mask provided comfort according to the different facial morphologies.
Thus, the results of this study are encouraging, as the enhanced PPE provided greater comfort to professionals in long working hours, with more than 4 hours. Allied to this, once the face of professionals is scanned, the data is stored allowing for quick replacement in case of breakage. Similarly, a previous study (15) also developed a frame for adaptation to surgical masks, obtaining good fit and sealing results. The differential of this study was the participation of a sample of dentists, collecting information about their perception of comfort in real care conditions during their clinical routine.
Another adverse event caused by the use of respirators reported in the literature refers to difficulty breathing (12,16,26), caused by CO2 inhalation inside the respirator (24). However, in the present study, participants reported good breathing capacity when using the PPE set to include ASTM level 1-3 masks.
Other types of PPE-related injuries can be caused by the combined effects of the use of multiple devices (19, 25), such as the pressure exerted on the frontal region by face shields (19). Face shields or visors are a protective barrier for the facial region, preventing the inoculation of droplets through the ocular conjunctiva, the contact of professionals' hands with eyes and face, as well as protecting the external part of the masks, which have their protective efficacy reduced when moistened (10,27). In the present study, professionals reported worsening visual acuity with the use of shields, probably due to blurring caused by inspiration and expiration inside the mask (16). In addition, face shields reflect and refract light, which can cause eye fatigue (25). Added to this, the composition of the material of the protectors can infer their transparency, as well as the dirt that can become impregnated during the procedures. In this sense, it is important that the face shield material has adequate transparency and allows for cleaning/disinfection, as it can be reused. It was observed that the use of the stock face shield and the 3D printed custom face shield frame was approximately similar, although the individualized 3D face shield can provide better adaptation, the stock face shield also had a good acceptance by the professionals in the present study.
A limitation of the current study is the small sample size, as well as a limitation of studies with questionnaires, as participation depends on the willingness of the participants to answer the questions (7). Moreover, there is non-randomization of the use of the different PPEs which results in absence of individual comparison. Finally, we have disproportion at the different categories mainly because of the sample size. Some ways to reduce the presented bias will be to do a decentralized study with more participants.
Thus, as conventional PPE prioritizes the adequacy of fit over comfort, in addition to the designs of the respirators not meeting all facial biotypes (17,24), the use of the present device associated with surgical masks may be a viable strategy in the short and long term in cases of emerging infectious diseases, favoring the comfort and occupational safety of professionals.
Conclusion
The 3D-printed custom frame adapted to ASTM surgical/medical face masks associated with the use of face shield showed reasonable tolerance among dental professionals and may be a viable alternative for the protection, comfort, and safety of health professionals who deal directly with aerosols in their clinical routine, especially during long hours of work. Further research is indicated to evaluate safety, comfort, compliance, side effects, and occupational hazards of longterm use of enhanced PPE recommendations.
Conflicts Of Interest
The authors declare no conflict of interest and has received no grants or funding for this project.
Author Contribution Statement
Conceptualization and design: G.D.R.T., J.K., U.O. Literature review: G.D.R.T., J.K., E.D.C., U.O.
Methodology and validation: G.D.R.T., J.K., and U.O. Formal analysis: U.O.
Investigation and data collection: G.D.R.T., J.K.
Resources: G.D.R.T., J.K., E.D.C., U.O.
Data analysis and interpretation: G.D.R.T., U.O.
Writing-original draft preparation: G.D.R.T., J.K., E.D.C., U.O.
Writing-review & editing: G.D.R.T., J.K., E.D.C., U.O.
Supervision: G.D.R.T.
Project Administration: G.D.R.T.