Introduction
Head and neck cancer (HNC) can attack various parts of the body in the upper aerodigestive tract, such as the oral and nasal cavity, the salivary and thyroid glands, the pharynx, the larynx and the paranasal sinuses (1). The treatment options include radiotherapy and surgery, depending on the stage and locations of the tumors. However, radiotherapy is also a palliative treatment option for inoperable late-stage tumors (2). Between 42% and 84% of HNC patients receive radiotherapy with increased survival rates (3).
Decreased saliva due to salivary gland hypofunction (4), radiation caries and periodontal disease (5) are the foremost adverse impacts of radiotherapy. A recent systematic review concluded that 21% and 24% dental caries prevalence rates had been reported following HNC radiotherapy and chemo-radiotherapy, respectively (5). Thus, due to this high risk, the regimen of an HNC patient necessitates a multidisciplinary team working with dental and medical clinicians.
Radiotherapy alerts cellular destruction by deoxyribonucleic acid (DNA) damage, preventing cell replication (6). Although not targeted, the tooth structures are inevitably affected by ionizing radiation applied to the maxillofacial region, but the literature contains contradictory findings. Several in vitro studies have indicated that the changes in the structure of enamel, dentin and the dentino-enamel junction are mostly dose dependent, and high doses could impair stability (7,8). The potential side effects of radiotherapy involve a lack of enamel prism, collagen fiber degeneration, obliterated dentinal tubules, gap formation at the enamel-dentin junction and decrease in microhardness (9,10).
Due to the aforementioned changes in tooth structure, researchers focus on the adhesion mechanisms of restorative materials used on radiotherapy-treated teeth. Additionally, radiotherapy may also affect readily restored enamel and dentin structures. Therefore, it is critical for an HNC patient to organize a timely treatment plan, with the use of the most beneficial adhesive system to achieve optimized treatment. However, there are controversial results, which are attributed to the selection of adhesive systems (11,12,13). Thus, adhesive systems must be chosen according to the substrate, and the selection of the most appropriate restorative material may be important under irradiated circumstances (14).
The latest generation of adhesives is referred to as ''universal adhesives'' and has been extensively implemented due to their versatility. Universal adhesives offer advantages to clinicians because of their user-friendly, simplified application protocols and multi-mode applicability on various substrates with etch&rinse and self-etch modes (15). However, it is unclear how these adhesive systems act on radiotherapy-affected dental structures.
Thus, the aims of this in vitro study were to investigate the shear bond strength (SBS) of a universal adhesive system to enamel and dentin; 1) that had undergone radiotherapy and 2) that were readily restored and had undergone radiotherapy in etch&rinse and self-etch modes.
The study's null hypothesis was as follows:
Irradiation with different timings would not affect the SBS of a universal adhesive to enamel and dentin applied in self-etch and etch&rinse modes.
Materials and methods
The local ethics committee approved this in vitro study (Process no.11/265).
Sample size calculation
The sample size calculation was performed based on the estimated effect size between groups, according to the literature (16). In this study, 15 specimens were required for each group to obtain a medium effect size (d=0.50), using 95% power and a 5% type 1 error rate.
Specimen preparation and restorative procedure
The chemical compositions of restorative materials employed in this study are listed in Table 1. The independent variables tested are as follows:
Presence and timing of irradiation (RT0: no radiotherapy/control, RT1: radiotherapy before restoration and RT2: radiotherapy after restoration).
The type of application mode of adhesive system (etch&rinse and self-etch modes).
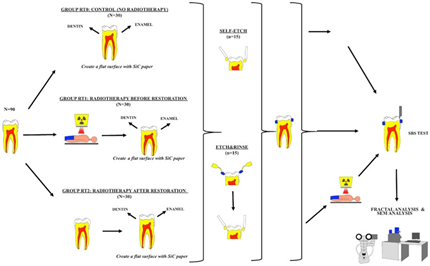
A total of 90 anonymized caries-free, intact human molars were used and kept in a saline solution until the experimental procedures. A schematic illus- tration of the experimental protocol is presented in Figure 1. The allocated groups are listed in Table 1. The teeth were randomly divided into six groups with respect to the presence and timing of irradiation and adhesive application types (n=15) (D.B.).
First, #120-grit silicon carbide (SiC) paper (Fuji Star Type DDC, Saitama, Japan) was used on the buccal and lingual surfaces of the teeth to create flat enamel and dentin surfaces under water cooling. Then, 600-grit SiC paper was applied with water cooling to obtain a standard smear layer using a metallographic polishing device (Minitech 233, Presi Grenoble, France). The dentin specimens were controlled for lack of enamel using a stereomicroscope (SMZ 1000, Nikon, Japan).
Table 1 The brand names/manufacturers, batch numbers and chemical composition of restorative materials used in this study.
Abbreviations: 10-MDP, 10-methacryloyloxydecyl dihydrogen phosphate; BIS-GMA, bisphenol A glycidyl methacrylate; HEMA, 2-hydro- xyethyl methacrylate; TEGDMA, triethylene glycol dimethacrylate; Bis-MPEPP, bis-methacryloxyethoxy phenyl propane; μm,micrometer; wt%, weight percentage; vol%, volume percentage; µm, micrometer; nm, nanometer.
Table 2 Allocation of the groups.
*Clearfil Universal Bond Quick in Etch&Rinse Mode; ** Clearfil Universal Bond Quick in Self-Etch Mode.
Group RT0+E&R (No Radiotherapy/Control with etch&rinse mode): This group did not receive radiotherapy. The enamel and dentin surfaces were created as mentioned above and etched with 37% phosphoric acid (Scothbond Universal Etchant, 3M ESPE, St Paul MN, USA) for 15s, rinsed with water for 10s and dried with cotton pellets. Universal adhesive (Clearfil Universal Bond Quick, Kuraray, Okayama, Japan) was used with a rubbing motion with a microbrush, gently air dried until the bond did not move and light cured for 10s (irradiance of 1,000 mW/cm², wavelength 385-515nm) with a third-generation polywave light-emitting diode (LED) light-curing unit (Valo, Ultradent, South Jordan, UT, USA). The light intensity was checked using a radiometer (Demetron LED Radiometer, Kerr Corp. CA, USA). In accordance with ISO 29022 (17), a cylinder-shaped Teflon mold (diameter: 2.4mm, height: 2mm) was placed on the adhesive surfaces of the enamel and dentin, and composite resin (Estelite Posterior Quick, Tokuyama Dental Corp., Tokyo, Japan) was inserted in a single increment and light cured with an LED light-curing unit for 10s. After removal of the molds, the composite resin was light cured again for 10s.
Group RT0+SE (No Radiotherapy/Control with self-etch mode): This group did not receive radiotherapy. The enamel and dentin surfaces were created as mentioned above. Universal adhesive was applied without acid etching, as described for the etch&rinse groups. The restoration procedures were applied as described for the etch&rinse group.
Group RT1+E&R (Radiotherapy before restoration with etch&rinse mode): The specimens enrolled in this group first received radiotherapy in distilled water in accordance with the primary and post-op definitive standard experimental radiotherapy protocol for treating HNC cancers whose details would be explained later in that section (30 fractions as daily 2 Gray per fraction, five days weekly for six weeks, and the total given dose, was 60 Gy).
Then, the enamel and dentin surfaces were created as mentioned above. The adhesive system with etch&rinse application and restorative proce- dures was applied as mentioned before.
Group RT1+SE (Radiotherapy before restoration with self-etch mode): The specimens enrolled in this group first received radiotherapy in distilled water in accordance with the primary and post-op definitive standard experimental radiotherapy protocol as mentioned above. Then, the enamel and dentin surfaces were created as described before. The adhesive system with self-etch application protocol and restorative procedures was applied.
Group RT2+E&R (Radiotherapy after restoration with etch&rinse mode): The enamel and dentin surfaces were created as described before. The adhesive system with etch&rinse application protocol and restorative procedures was applied. Then, the specimens received radiotherapy in distilled water according to the primary and post-op definitive standard experimental radiotherapy protocol as mentioned above.
Group RT2+SE (Radiotherapy after restoration with self-etch mode): The enamel and dentin surfaces were created as described before. The adhesive system with self-etch application and restorative procedures was applied. Then, the specimens received radiotherapy in distilled water according to the primary and post-op definitive standard experimental radiotherapy protocol as mentioned above.
All the restorative procedures were completed in accordance with the manufacturers' instructions. All restorative procedures were done by a single operator who was blinded to the presence and timing of irradiation (B.O.). Besides, all speci- mens were kept in non-irridiated distilled water between radiotherapy cycles until SBS test.
Radiotherapy protocol
The radiotherapy treatment of the specimens was performed at the Radiotherapy Center of the Oncology Clinic. Before the irradiation, the output dose of the device and deep dose tables were used. Manual planning was performed to mimic the clinical scenario of an adult patient with HNC. During the planning process, the analytical anisotropic algorithm dose calculation was employed to provide the same radiation dose to the specimens. Specimens were placed on wax plates extended to 2mm away from the cemento-enamel junction and positioned 0.5cm apart from each other to prevent scattering and allow for direct irradiation. The wax plates were fixed in a plastic container filled with distilled water, imitating the oral cavity (18).
Then 1.25 MeV gamma rays were delivered to the specimens through a direct field on the surface of each tooth, using a Cobalt60 device (CisBio International CIRUS model teletherapy device, 312TBq, Healvita GmBH, Vienna, Austria). Irradiation of non-radioactive cobalt 59 with neutron results in the radioactive element COBALT 60 and two gamma energies formed in the nuclear reactor. Because of the radioactive decay of the 27Co60 element, two gamma energies are formed, 1.1732 MeV and 1.3325 MeV. The 1.25 MeV used in the treatment is the arithmetic mean of both of these gamma energies. The distance of the material surface from the source was 80cm, and the surface area to be irradiated was 12 x 12 cm². The irradiation dose rate was 29.83 cGy/min. The irradiation room temperature was determined as 24Cº, the pressure was P=1019 (hpa), and the humidity was kept at 60%. The maximum dose depth of Cobalt 60 gamma rays is 0.5cm. Fixed irradiation was performed with a 98% deep dose. Irradiation was completed in 30 fractions as daily 2 Gray perfraction, five days weekly for six weeks, and the total given dose, separately in both groups, was 60 Gy (19). Quality control was performed using a dosimeter. The process of radiotherapy was carried out by a physician (A.H.E.).
Shear bond strength test
A notched-edge SBS test was performed using a universal test machine (AGS-X, Shimadzu Corp., Japan) (crosshead speed of 1mm/min) by a blinded investigator. The testing load was directly applied at the tooth-restoration interface until the fracture, with a notched-edge crosshead matching the diameter of the bonded cylinder (20). SBS values were calculated by dividing the maximum load (N) at the time of the fracture by the adhesion area (mm²), recorded as Newtons and converted to MPa.
Failure type analysis
Failure type analysis was performed using a stereomicroscope under 15x magnification to determine the failure modes. The failure mode was recorded as an ''adhesive'' failure if the fracture occurred along the junction of the resin composite and enamel/dentin, the failure mode was recorded as a ''cohesive'' failure if the fracture occurred in the resin composite or enamel/dentin, and the failure mode was recorded as a ''mixed'' failure if the fracture occurred in the resin composite or enamel/dentin.
Environmental scanning electron microscope analysis
For morphological analysis, one representative specimen from radiotherapy-treated and non-treated enamel and dentin surfaces were prepared and the adhesive system was applied as mentioned before. Then, they were stored in distilled water at 37°C for 24 h and then sectioned lengthwise with a low-speed diamond saw under water cooling. The sectioned surfaces were submerged in 6 N HCL for 30s to demineralize the dentin, then rinsed with water for 5min. Then they were submerged in 3% NaOCl for 10min and rinsed with water for 5min. A desiccator was used to dehydrate the specimens for 12h (21). They were fixed on aluminum stubs for platinum coating. The specimens were analyzed on sagittal plane under an environmental scanning electron microscope (E-SEM) (E-SEM; FEI QUANTA FEG 250, Oregon, USA) to evaluate the resin-enamel/ dentin interface in a secondary mode at an accelerating voltage of 10-30 kV. The micromorphology of representative surfaces was obtained at 1,000x and 2,500x magnification. An operator who was unaware of the presence and timing of irradiation or type of application mode performed all the E-SEM analyses.
Statistical analysis
Statistical analysis was conducted with SPSS 22.0 for Windows. The Shapiro-Wilk test was first used to indicate the normality of variables, and the data were then analyzed with Levene's test for homogeneity of variances. The data were normally distributed. A two-way analysis of variance (ANOVA) was performed to analyze if study factors were significant or not. All pairwise comparisons were done using the Bonferroni test. Statistical significance was considered at a confidence level of 0.05 for all analyses.
Results
Shear bond strength test
Tables 3 and Tables 4present the mean SBS values with standard deviations in MPa of the tested groups for enamel and dentin, respectively. For enamel, two-way ANOVA showed that the type of application mode of adhesive system (etch&rinse and self-etch modes) significantly influenced the SBS values (p<0.05), whereas the presence and timing of irradiation (RT0:no radiotherapy/ control, RT1: radiotherapy before restoration and RT2:radiotherapy after restoration) did not signifi- cantly (p>0.05). Besides, the interaction between these two study factors had no significant effect on the SBS values (p>0.05). Bonferroni test indicated that significantly higher SBS values were obtai- ned using etch&rinse mode than self-etch mode (p>0.05). For dentin, two-way ANOVA showed that either the presence or timing of irradiation or type of application mode of adhesive system did not significantly influence the SBS values. Besides, the study factors had no significant effect on the SBS values (p>0.05).
Failure type analysis
Table 4 presents the failure type analysis after the SBS test for all tested groups. Regarding enamel, the predominant failure mode was the mixed type for all tested groups. The second most frequently observed failure mode was the cohesive type with the etch&rinse application mode, while no cohesive failures were observed for the groups with the self-etch application mode. Group RT1+SE exhibited only the mixed type of failure. Regarding dentin, the predominant failure mode was the mixed type for all tested groups. The second most frequently observed failure mode was the adhesive type for all tested groups and it is the predominant failure mode in Group RT2+SE. Additionally, no cohesive failures were detected for most of the tested groups.
Environmental scanning electron microscope analysis
Representative SEM images of the resin- enamel/dentin are illustrated in Figure 2. Non-irradiated enamel specimens indicated regular healthy enamel with the regular presence of prisms (Figure 2.A and Figure 2.C) (white arrow). Irradiated enamel specimens indicated a shorter and rounded prism appearance, and loss of enamel prisms was detected in some areas (Figure 2.B and Figure 2.D) (white square). Non-irradiated dentin specimens exhibited regular and significant dentinal tubule structures (Figure 2.E and Figure 2.G), where as irradiated dentin specimens had irregular and obliterated dentinal tubules (Figure 2.F and Figure 2.H) (red arrow). Few resin tags were clearer in the irradiated enamel specimens treated with the etch-rinse approach (Figure 2.B) (black circle), while those treated via the self-etch approach (Figure 2.D). Additionally, non-irradiated dentin specimens treated with the self-etch mode indicated resin tag formations (black arrows) (Figure 2.G), whereas irradiated specimens had a thin hybrid layer appearance without resin tags (Figure 2.H).
Table 3 The mean shear bond strength values (SBS) and standard deviations (±SD) of all tested groups for enamel in MPa (n=15).
*A two-way analysis of variance (ANOVA) indicated that the study factors were significant or not. All pairwise comparisons were done using the Bonferroni test (p<0.05).
Table 4 The mean shear bond strength values (SBS) and standard deviations (±SD) of all tested groups for dentin in MPa (n=15).
*A two-way analysis of variance (ANOVA) indicated that the study factors were not significant (p>0.05).
Table 5 Failure type analysis after SBS test for all tested groups (%).
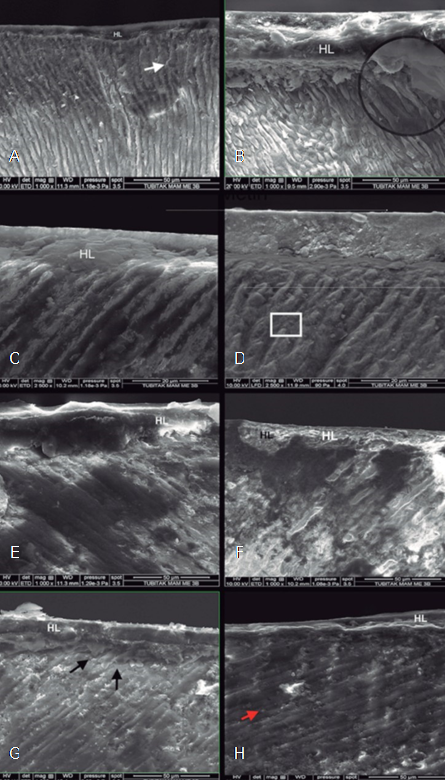
Figure 2 E-SEM micrographs of all tested groups at 1000x and 2500x magnification. A) non-irradiated enamel with ER mode, B) irradiated enamel with ER mode, C) non-irradiated enamel with SE mode, D) irradiated enamel with SE mode, E) non-irradiated dentin with ER mode, F) irradiated dentin with ER mode, G) non-irradiated dentin with SE mode, H) irradiated dentin with SE mode. HL: hybrid layer, black circle and black arrows: resin tags, white arrows: regular presence of prism, white square: loss of enamel prism, red arrow: obliterated dentinal tubules.
Discussion
In this study, the SBS of a universal adhesive system to enamel and dentin; 1) that had undergone radiotherapy and 2) that were readily restored and had undergone radiotherapy in etch&rinse and self-etch modes was investigated. Based on the results, the null hypothesis, that irradiation with different timings would not affect the SBS of a universal adhesive to enamel and dentin applied in self-etch and etch&rinse modes, was partially rejected.
HNC affects more than 550,000 people worldwide every year (22). Parallel to the increasing lifespan of populations, the incidence of neoplastic diseases has increased, and people use their teeth for longer periods. Thus, dentists should be aware of the adverse effects of radiotherapy to treat HNC patients, both before and after the radiation protocol (18). Despite the benefits of radiotherapy, the harmful effect of radiotherapy on hard dental tissues is pronounced, with increasing doses, resulting in morphological changes on both enamel and dentin, decreases in microhardness and gap formation at the enamel-dentin junction (9,10,23). Additionally, it has also been reported that the tooth-restoration interface could be negatively affected by the degenerated collagen network and obliterated dentin tubules in the hybrid layer (24). It is also important to emphasize that radiotherapy could also influence the properties of restorative materials in terms of surface roughness, flexural strength, microhardness and water sorption (25).
The radiotherapy protocol used in this study used in the previous study and actual clinical scenarios and consisted of cumulative fractioned doses of 2 Gy daily on weekdays, until the final dose of 60 Gy (26). The design of the methodology included the usage of molar teeth, since molar teeth have received the highest dose of radiation during radiotherapy (27). During the radiotherapy protocol, the specimens were kept in distilled water since submersion in artificial saliva could hamper proper delivery of the irradiation because of its viscosity and high concentration of ions (18).
Ionizing radiation induces the action of reactive oxygen species (ROS), such as hydroxyl radicals, superoxide anion and hydrogen peroxide (28). The formation of free radicals and the radiolysis of water molecules could lead to cell necrosis (29). Reactive oxygen species could be produced in dental tissues with higher water content levels such as dentin, but also on the storage media of teeth subjected to in vitro radiotherapy. Additionally, although water constitutes an insignificant portion of enamel, its involvement affects the mechanical properties of the structure when it is dehydrated (30). In this respect, ROS could behave as a polymerization inhibitor of the adhesive system, influencing its immediate bond strength to dentin or enamel (31). In this study, no significant differences in SBS were observed for the enamel and dentin specimens treated with the etch&rinse and self-etch modes, irrespective of the radiation protocol. This finding agrees with Da Cuncha et al., (24) who reported that radiotherapy did not influence the bond strength of a universal adhesive to enamel and dentin. Additionally, Gernhardt et al. (32) reported that no significant differences in dentin bond strength were observed between the irradiated and non-irradiated groups. However, previous studies (31,33) have indicated that radiotherapy before restoration group exhibit lower dentin bond strength values compared to the no-radiotherapy group. Arid et al., (26) who evaluated the SBS values of enamel and dentin specimens with different radiotherapy scenarios after application of the self-etch and etch&rinse adhesive systems, reported that radiotherapy after restoration groups had significantly lower SBS than the no-radiotherapy groups for both enamel and dentin. Biscaro et al. (34) reported that a radiotherapy after restoration had lower dentin bond strength values than a no-radiotherapy group with the application of the etch&rinse and self-etch adhesive systems. The divergence in outcomes can be attributed to the differences in types of adhesive systems and methodologies. Ozan et al., (12) who evaluated the dentin bond strength of universal adhesives, reported that their radiotherapy before restoration group had lower bond strength values than their no-radiotherapy group with the application of the etch&rinse mode. The divergence in outcomes can be related to the differences in the types of specimens they used (extracted radiotherapy-treated teeth).
In the past decade, manufacturers have introduced universal adhesives with a ''quick bonding'' protocol on different substrates. The universal adhesive system used in this study, contains 10-methacryloyloxydecyl dihydrogen phosphate (10-MDP) and a newly developed hydrophilic amide monomer and features a mild acidic pH. In past research, 10-MDP establishes an intensive and stable chemical interaction with hydroxyapatite. The MDP-Ca water-insoluble salts promote the preservation of collagen fibers (35). The hydrophilic amide monomer would have a higher setting ability; hence, the formed polymer would be robust to hydrolysis. Additionally, as the monomer has a higher hydrophilic potential than 2-hydroxyethyl methacrylate, it has good wettability to dental tissues (36). In this study, concerning the application mode of universal adhesive systems, the etch&rinse mode caused significantly higher enamel SBS values than the self-etch mode for all radiation protocols. This finding is in contrast with the results of Arid et al., (26) who reported that etch&rinse adhesive systems produced lower SBS than self-etch adhesive systems after radiothe- rapy since radiotherapy could make enamel more porous. The divergence in outcomes can be attributed to the differences in types of adhesive systems they used. Besides, in this study, according to the application modes, for the no radiotherapy group, no significant differences were found for enamel and dentin. Similar to this study, Hanabusa et al. (15) stated that the dentin bond strength of the application of the etch&rinse mode was similar to the strength of the self-etch mode. This finding is in contrast with Sai et al., (37) who reported that etch&rinse application caused higher SBS values than the self-etch approach. This divergence in outcomes can be attributed to the different type of specimen they used (bovine incisors).
In this study, stereomicroscope observations highlighted that the predominant mode of failure was the mixed type. Irradiated enamel specimens treated with the self-etch mode for the radiotherapy before restoration exhibited the highest frequency of mixed type failures, which may contribute to the high bond strength values. This indicated that the quality of the bond strength at the interface is such that it exceeds both the cohesive strength of dental tissues or restorative materials and the adhesive strength between the interfacial layers, providing an adhesive interfacial bonding that presents greater strength when acting as a single structure (38). What is more, the frequency of cohesive failure, in addition to mixed failures, tended to increase for the etch-rinse mode with irradiated enamel specimens. Therefore, failure type analysis of the specimens suggested that phosphoric acid pre-etching can contribute to the adhesion of irradiated enamel by establishing micromechanical interlocking. An increase in adhesive failures and a decrease in mixed failures were observed for the dentin specimens treated with the self-etch mode in the radiotherapy after the restoration group compared to the no-radiotherapy group, implying that the weak link was the bond between the resin and the dentin. No cohesive failures were observed for the enamel and dentin specimens with the self-etch mode, regardless of the irradiation protocol.
In this study, SEM observations of irradiated and non-irradiated specimens indicated significant structural differences originating from the radiotherapy (Figure 2). Loss of the enamel prism structure and obliterated irregular dentinal tubules were found for the radiotherapy-treated specimens (Figure 2.B, Figure 2.D, Figure 2.F, and Figure 2.H). This finding agrees with Gonçalves et al., (30) who reported that radiotherapy causes a more porous enamel surface. However, the tested irradiated and non-irradiated specimens did not differ in SBS values. Additionally, the morphological properties at the resin-enamel interface differed regarding the application modes. Resin tags were more visible in the irradiated enamel specimens treated with the etch-rinse mode compared to those treated with the self-etch mode (Figure 2.B and Figure 2.D), consistent with the increased cohesive failures for the radiotherapy before restoration group with the etch-rinse mode. Additionally, non-irradiated dentin specimens treated with the self-etch mode featured resin tag formations (Figure 2.G), whereas irradiated specimens had a thin hybrid layer appearance without resin tags (Figure 2.H). Amide monomers could penetrate deep into the demineralized dentin and polymerize to develop a stable polymer network, providing strong microme- chanical interlocking (39). Thus, this finding could be attributed to the negative effects of radiotherapy on the collagen network (33).
Employing only superficial dentin surfaces along with enamel without any aging procedures may be considered a limitation of the current study. Thus, further studies are needed to focus on the effect of radiotherapy on the different properties of deep dentin, allowing for aging.
Conclusion
Despite the limitations of this study, the following conclusions can be drawn:
Irradiation with different timings did not influence the bond strength of the universal adhesive to enamel and dentin, negatively.
The etch&rinse mode caused higher bond strength to enamel than self-etch mode with both radiation protocols.
The predominant mode of failure was the mixed type for both substrates, regardless of the application modes and radiation protocol.
The SEM analysis indicated that the loss of the enamel prism structure and obliterated irregular dentinal tubules were found for the radiotherapy-treated specimens. Additionally, resin tags were clearer in the irradiated enamel specimens treated with the etch-rinse mode compared to the specimens treated with the self-etch mode.
Author contribution statement
Conceptualization and design: B.O., A.H.E., A.M., N.A., D.B.
Literature review: B.O., N.A.
Methodology and validation: B.O., N.A. Formal analysis: B.O., N.A.
Investigation and data collection: B.O., D.B. Data analysis and interpretation: B.O., N.A. Writing: B.O., N.A.
Review & editting: B.O., N.A., A.M., D.B.