Nowadays, more dentists are aware about painful orofacial conditions; turning an old taboo into a daily clinical concern. It seems that our current sociocultural context favors in many patients’ emotional stress that in many cases will be somatized as oral and facial pain. Besides, the free access to web information (or unfortunately misinformation) leads to an increase demand of diagnostic skills and treatment options in this field by those who suffer orofacial pain. For these reasons, it is mandatory for dental practitioners to update their knowledge in this subject, specially when confronted to a clinical situation which demands an explanation of WHAT IS PAIN, and WHAT IS MY TYPE OF PAIN.
What’s new the new definition of pain?
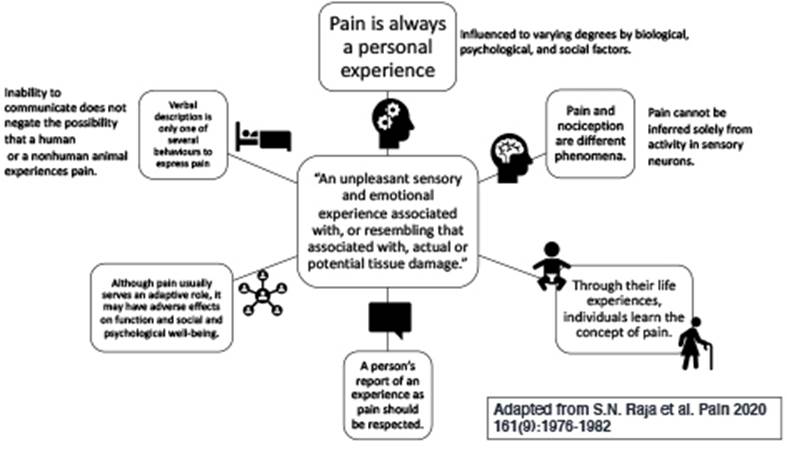
Over four decades ago, the International Association for the Study of Pain (IASP) promulgated a definition of pain, recognizing the world’s need for a verbal expression of this complex sensorial experience. But coming up with the correct wording which could contain all the known different aspects surrounding this concept was not an easy task. The process for adopting this definition took over 2 years of deliberations and a subcommittee including representatives from different specialties was formed, until finally in 1979 the IASP published the definition and it was globally adopted by international organizations and entities including the World Health Organization. Pain was defined as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage” (1). In recent years, the case for a reevaluation of this definition was proposed by many (2,3,4,5) and a IASP Task Force was formed to evaluate the current definition of pain and to recommend if, based on current evidence-based knowledge, a new definition was in order. In 2020, the Task Force recommendations were accepted by the IASP Council and a revised definition was published. Pain is now defined as “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage” (6). Figure 1 presents the recently published definition and its complementary note.
Before analyzing the updated version of the definition in the context of oral health and dental pain, lets discuss why a definition is needed and who should be using it. Pain can be described in a great variety of variables such as intensity, quality, and duration but also could derive from diverse pathophysiologic mechanisms. Hence, defining the concept of pain in a single concise and precise manner presents a challenge (4). The pragmatic characteristic of a single definition for pain consists in its simplicity and brevity while recognizing the multidimensional aspects surrounding this term. The word PAIN then, may be accompanied of several “last names” which will lead to a certain classification or an specific contextualization. In terms of temporary behavior, we have heard the words chronic or acute pain; or when referring to localization we use to clarify if it is a local or generalized pain conditions. The same happens when we consider etiology (the cause of pain) or the involved mechanisms; but at the end, we will be facing the same concept with different approaches and clinical implications. With this in mind, the definition provides people with pain, caregivers, researchers, politicians, and all other involved parties, with a comprehensible term, with global application to understand the concept of pain and with the intention to promote pain research, policy, advocacy, and most important, adequate clinical care.
Since pain is a personal experience and a very complex one to fully understand, only by enduring pain an individual can truly be cognizant of the various degrees of its biological, psychological, and social factors, as the first note of the new definition proposes. Accordingly, a single definition will not possibly address the range of strategies that span self-care, social, psychological, pharmacological and interventional approaches required (and for most people a combination of these) to treat pain (7).
A quick comparison between the previous and the new definition of pain could trick the reader into believing that the proposed changes are too subtle to even worth the effort of revising the definition and modifying and publishing the new definition. But let’s revise the underlined added text of the new definition: “pain is an unpleasant sensory and emotiona lexperience associated with, or resembling that associated with, actual or potential tissue damage.” This addition is a reflection of the contemporary und erstanding that pain, particularly some forms of chronic pain, could be perceived as an ongoing tissue damage, although, it is not directly associated with tissue damage but with some type of nervous system dysfunction (8). Such could be the case of the diagnostic criteria still defined as Persistent Idiopathic Facial Pain, where pain cannot be attributed to any pathological process but deemed uncertain (9). We will discuss this and similar situations later in the article as these are probably the earnests challenges clinicians must confront when dealing with pain in the dental setting.
Most of the changes between the previous and the new definition are evident in the notes that follow the definition (Figure 1). Many concepts were updated to the new understanding of pain and its many factors. A clear example of this is the inclusion of a note stating that “verbal description is only one of several behaviors to express pain; inability to communicate does not negate the possibility that a human or a nonhuman animal experiences pain”. This statement is especially relevant in the research context where much of the preclinical studies use animal models to evaluate analgesia protocols and/or molecules. Moreover, this note resolves the complaints that the previous definition relied mainly on self-report ability of the individual, thus potentially marginalizing nonverbal groups such as neonates, people with intellectual disabilities, degenerative brain disease, linguistic disorders, and all nonhuman animals (4). It also widens the possible approaches to further investigate the high prevalence of pain (especially chronic pain) in some populations with psychiatric conditions and how one modifies the risk of the other (10).
A different analytical angle is to discuss the aspects that remained unedited from the first definition of pain, after all, for more than 40 years it suited the needs for all the parties involved. Undoubtfully, he most relevant aspect was the recognition back then that pain is a sensory and emotional experience. Acknowledging the fact that pain is not solely a sensory experience but that also emotional, cognitive and social components may induce the experience of pain (3,5,11), is what probably sustained the previous definition current for all those many years without the need for a revision.
How this new definition may impact future approaches in healthcare, policy making, and research (both preclinical and clinical), we will see in the next years. It certainly provides a useful tool to assure the relevant aspects encircling the concept of pain will be considered in the different possible settings. As research in pain develops, more studies are needed to explore pain neural pathways and the mechanisms of the perception of pain, neuropathic pain, inflammatory pain, and the transition from acute to chronic pain. More funding is required to study and develop new and more effective therapies for pain, especially chronic pain, in consequence reducing the potential for addiction and abuse of pain medication, such the case of the opioid pandemic sustained by some populations. Combined efforts to recognize the global burden of pain and how it affects quality of life, sleep, work, decreases socialization, increases health care costs, and mortality (12), are much needed.
The new international classification of orofacial pain and its impact for dental practice
There is no simple way of classifying pain just as there is no simple way of defining pain. But as Pigg et al. (13) stated “to ensure understanding between health care practitioners and researchers, a widely accepted orofacial pain classification would be helpful”, the International Classification of Orofacial Pain (ICOP) was timely published in 2020. This effort contributes as a tool which purpose is to enhance research and management of orofacial pain through active collaboration between related specialties of head and neck medicine. The World Dental Federation (FDI) recognized the importance of stablishing a common language when talking of orofacial pain and the policy statement on Odontogenic Pain Management which purpose was to address the world national dental associations, dental academic groups, and clinicians to improve proper management of odontogenic pain, was adopted in 2017 (15).
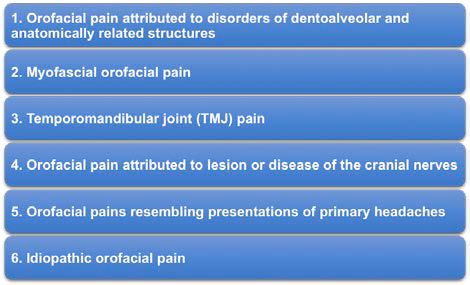
ICOP adopts and adapts the well stablished Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) (16) and the International Classification of Diseases 11th Revision (ICD-11)/ International Association for the Study of Pain (IASP) criteria for orofacial pains and headaches. This helped in stablishing clear terminology and allowing a better communication and data sharing between groups. The classification design is hierarchical and uses the coding style of the International Classification of Headache Disorders (3rd edition, ICHD-3) for ease of use. In order to be a comprehensive tool, the ICOP is divided in 6 chapters, making the classification of all pain conditions affecting the orofacial regions more functional (Figure 2). It differentiates between primary pain when it is not explicable by other disorder and secondary pain when it is caused by another condition such a swelling due to infection.
Additionally, pain is sometimes subcategorized in acute and chronic types and stablishes chronic pain as lasting more than 3 months. Finally, the coding for pain classification uses a maximum of 7 digits, but the number of digits used for a diagnose may vary depending on the amount of known information about the case and most important in the level of detail needed by the user of the tool. For example, a general dentist may need to use 1-3 digits after a diagnostic appointment and to refer the patient to a specialist. A specialist may need to use the third through fifth digits after confirming the first diagnose and running further diagnoses or interventions. And lastly a researcher my require the fifth through seventh digit if a further description of the case is needed. Following the recommendations by Pigg et.al. (13), the clinician responsible of diagnosing and treating dental pain, will need to play an special role in determining if the condition fits to the first category, emphasizing in the participation of pulpal and/or periodontal tissue; to decide the best treatment for the patient. If not, then the referral note must contain all the available information to guide the correct diagnosis into the other categories. Finally, interconsultation and open communication channels between the patient, the dentist and specialist collaborators will be crucial.
By unifying a new pain definition and to adopt a new clinical classification of pain, the first expected effect will be open minds within the clinicians. Everybody will be more careful when trying to explain what pain is, as well as when the patient was what is the source and name of his/ her painful condition.