INTRODUCTION
Health promotion is crucial in the field of medicine (1,2,3), particularly dental medicine (4). Excellent oral health practice is propagated to dental patients through oral health promotion. Within the field of health promotion, patient education is a foundational concept that is important in the field of health care (5,6). Patient education is defined as an active, planned process of disseminating information that systematically modifies the knowledge and attitude of patients (7,8). Oral diseases are mostly preventable. Patients who attained knowledge related to oral diseases are amenable to preventive measures (9,10) Patient education in dental medicine is aimed at the prevention of oral diseases. The approach involves information sharing and actionable policies, making it a cost-effective way of improving quality of life (5,11,12). In a lifespan, oral diseases have a negative impact on the quality of life (13,14,15). One of the objectives of the health care provider is to improve the quality of life through oral health promotion. If a two-way communication between the health care provider and the dental patient is aimed for oral health, then the general health of the patient is also considered Oral health is an influencing factor in the general health of a person (16,17,18).
Technology has transformed the way systems, forms and materials for patient education evolved (19,20,21). One of the forms includes case presentations. Case presentation is a widely used by health care providers (22,23). The method is also used in the medical education curriculum as a teaching-learning strategy for health care providers. A fluent case presentation allows for efficient transitions between providers, students, and even patients (24). Case-based learning also serves as a useful proxy for assessing student competency in clinical reasoning and patient care (23,25,26,27).
The digital era, consisting of internet- based services and information technology, offers opportunities for patient education in dental medicine. Easy access to medical websites at any moment is available. Information for the patient’s benefits can be accessed immediately through these services (28). Health websites also include video-based instructions that are effective at developing short-term health literacy goals (29,30). A Video-based presentation is a tool for presenting practical data to patients who are seeking medical care (31). Patients retain more information when presented in video-based format which include video and audio technology (32). The universal access to health information on the internet emphasizes the significance of communication between the patient and the health care provider (33). However, the quality of health information in different websites vary widely and some of them may be inaccurate and potentially harmful.
The integration of video technology in case-based presentations are useful approaches in teaching real-world problems that ultimately improves an individual’s ability to reflect, analyze, and decide regarding any circumstance leading to change in behavior. Case-based presentations are also useful in non-health related topics for education (34). The informative features of a case-based learning approach express an empathetic socialization process that allows patients or learners to understand and relate with the example presented as a medical case. The process allows an active interaction with the health care providers that is useful in lifelong learnings (35). Documented advantages of case-based learning approaches emphasize the promotion of self-directed learning, clinical reasoning, and decision making. Inquiries regarding the cases will be developed through a deep learning experience that highlights cognitive and social constructivist theories of education (36). There are limited studies regarding the use of case-based learning approaches for dental patients. Anchored on the Theory of Planned Behavior, this study aims to determine the effectiveness of an online case-based video patient education tool on the adoption of oral health behaviors by patients in the dental setting.
MATERIALS AND METHODS
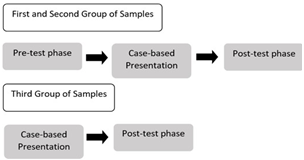
Approval for this quasi-experimental study was obtained from the University of Santo Tomas Graduate School. A purposive sampling method was utilized to choose three groups of patients to participate in this study. Group I (Control Group) consisted of patients who have experienced prior professional oral health care. Group II (Experimental Group) consisted of patients who have never experienced professional oral health care. The third group (Group III) consisted of health care professionals comprised of dentists, physicians, and nurses. Individuals who participated satisfied the following inclusion criteria: 1) patients who gave their consent. 2) 18 years old and above. 3) able to read the English or Filipino language. 4) of sound mind with no mental illness. Informed consent was gathered from participants. Informed consent was obtained from the participants in the study. The informed consent included a clear and detailed explanation of the purpose of the study; a description of the methods of the study; the patient’s voluntary participation, their right to refuse to join or withdraw from the study at any time, and the assurance that their privacy and the confidentiality of all information given. Sample size was calculated based on a margin of error of 5%, a confidence level of 90%, a population size of 100 and a response distribution of 50%. The recommended sample size was calculated as 74 participants in the patient groups.
CASE-BASED PRESENTATION
The video presentation of two clinical cases, which is anchored Case-based Learning Model, was presented to the three groups of participants. The clinical cases consisted of limited information regarding a patients’ condition. The online case-based presentation included a brief patient’s information, chief complaint, diagnosis, and treatment. The case-based presentation also included pre-operative and post-operative clinical photographs. The first clinical case was the case of a betel nut induced stains, while the second clinical case involves the case of generalized chronic periodontitis. The clinical cases included limited patient information to make the presentation brief and concise. The clinical cases serve as examples of what may happen before and after the treatment of their corresponding conditions. The video was also uploaded on Google Forms. The duration of the video is 4 minutes and 44 seconds duration. Professional oral cleaning has also been demonstrated in the video. The method shows how a dentist uses a low-speed handpiece for professional brushing to remove dental plaques or stains. The method also shows how a dentist uses an ultrasonic scaler for professional scaling to remove calcular deposits. Groups I and II underwent a pre-test and post-test scheme, while participant healthcare professionals in Group III underwent a post-test scheme.
Groups I and II in the pre-test phase were asked to complete a “Dental Neglect Scale” questionnaire on Google Forms (37) using a computer provided by the researcher. Google Forms is an online application of teaching materials that may include videos, photos, and questions.
DENTAL NEGLECT SCALE
The Dental Neglect Scale is a validated research instrument that is utilized in assessing the degree of dental neglect or of disregard of oral health among dental patients. The Dental Neglect Scale (DNS) assesses the extent to which an individual cares for his/her teeth, receive professional dental care, and believes oral health to be important. The Dental Neglect Scale is 6-item questionnaire consisting of a 5-point Likert scale system from Point 1 equivalent to “Definitely No” while point 5 is equivalent to “Definitely Yes”. The scoring system consists of obtaining a minimum score of 6 points and a maximum score of 30 points. The 6-item questionnaire was developed in consideration of the short duration of time that a participant must answer. The measure is aimed towards contributing to the theories and principles of assessing dental neglect in the dental community and academic community (38,39,40).
PATIENT EDUCATION MATERIALS ASSESSMENT TOOL (PEMAT)
In the post-test phase, participants in Group III were asked to complete a “Patient Education Materials Assessment Tool (PEMAT)” questionnaire on Google Forms using a hyperlink sent by the researcher. The patient education materials assessment tool (PEMAT) is a validated research instrument that is utilized in the evaluation of the understandability and actionability aspect of patient education materials. In this study, the case-based learning presentation is the patient material that was assessed by the health care professionals through the PEMAT. The patient education materials assessment tool consisted of two forms, namely PEMAT-P and PEMAT-A/V. The separated forms are specifically designed questionnaires. The PEMAT-P is designed for printed patient education materials while the PEMAT-A/V is designed for audiovisual patient education materials. The form of the patient education materials assessment tool that was used in this study was the PEMAT-A/V. The PEMAT-A/V consists of 13 items that are related in measuring understandability, while 4 items are designed to measure actionability. The guidelines for usage of the PEMAT-A/V required the researcher to review applicable questions to the case-based learning model. Some questions in the PEMAT-A/V were considered “Not Applicable” and were removed from the final list of questions that were presented to the health care professionals. The final number of items that were presented to the health care professionals was 14 questions. Each item can be answered by the health care professionals through the response of “Agree” or “Disagree”. The PEMAT provides two scores for each patient material. The two scores include an understandability score and an actionability score (41,42,43,44). Interventions for the Group III patients did not include a Pre-test and the case-based presentation was immediately presented to the them. After completing the Dental Neglect Scale in the pre-test phase, the case-based video presentation was presented among the participants in Groups I and II.
After watching the video-based presentation, participants in Groups I and II were asked to accomplish the post-test phase which again involved the completion of a Dental Neglect Scale questionnaire and the PEMAT A/V. Data were analyzed using SPSS Statistics 26 software (IBM Corp. Released 2019. IBM SPSS Statistics for Windows, Version 2.0. Armonk, NY: IBM Corp.). A paired t-test was used for the before and after data and the independent t-test was used to assess significant differences between groups. Understandability and actionability scores for the Group III patients were likewise obtained and analyzed.
RESULTS
A total of 37 participants per group in Groups I and II (N= 74) responded to the pre-test phase and the post-test phase. A total of 15 participants in Group III completed the post-test phase.
Table 1 shows the breakdown of the responses by Groups I and II in the pre-test and post-test phases. The pre-test mean scores of Groups I and II were 11.43 and 15.05, respectively. The post-test mean score of Groups I and II were 10.81 and 12.76, respectively. There is no statistical significance seen in the pre-test mean score and the post-test mean score of the patients who experienced professional oral health care (Group I) (p=0.113). However, there is a statistical significance seen in the pre-test mean score and the post-test mean score of the patients who never experienced professional oral health care (Group II) (p=0.032). There is also a statistical significance seen in the post-test mean scores of the patients who experienced professional oral health care (Group I) and the patients who never experienced professional oral health care (Group II) (p=0.05).
Out of the 15 participants in Group III, 11 (73.3%) have a graduate or post-graduate degree. 9 (60%) participants reported that they are currently a member of an educational institution. Out of the 15 participants, 6 (40%) were dentists, 6 (40%) were physicians, and 4 (26.7%) are nurses. Table 2 shows the breakdown of those who answered “Agree” in the health professional group (Group III). The mean understandability score in Group III is 94.54%, while the mean actionability score is 97.78%.
Table 1 Responses to the Dental Neglect Scale categorized according to Groups.
| Dental Neglect Questions | - | Group 1 n=37 | - | Group 2 n=37 | - |
|---|---|---|---|---|---|
| Category | Answer | Pre-test | Post-test | Pre-test | Post-test |
| 1. I keep up my home dental care | 1 | 43.2% (16) | 43.2% (16) | 21.6% (8) | 37.8 (14) |
| - | 2 | 27% (10) | 40.5% (15) | 24.3% (9) | 24.3% (9) |
| - | 3 | 24.3% (9) | 16.2% (6) | 43.2% (16) | 29.7% (11) |
| - | 4 | 2.7% (1) | 0% | 8.1% (3) | 5.4% (2) |
| - | 5 | 2.7% (1) | 0% | 2.7% (1) | 2.7% (1) |
| 2. I receive the dental care I should | 1 | 45.9% (17 | 40.5% (15) | 18.9% (7) | 27% (10) |
| - | 2 | 32.4% (12) | 37.8% (14) | 18.9% (7) | 24.3% (9 |
| - | 3 | 21.6% (8) | 21.6% (8) | 45.9% (17) | 32.4% (12) |
| - | 4 | 0% | 0% | 8.1% (3) | 10.8% (4) |
| - | 5 | 0% | 0% | 8.1% (3) | 5.4% (2) |
| 3. I need dental care, so I do not out if off | 1 | 37.8% (14) | 45.9% (17) | 16.2% (6) | 35.1% (13) |
| - | 2 | 24.3% (9) | 32.4% (12) | 21.6% (8) | 29.7% (11) |
| - | 3 | 37.8 (14) | 21.6% (8) | 35.1% (13) | 21.6% (8) |
| - | 4 | 0% | 0% | 21.6% (8) | 8.1% (3) |
| - | 5 | 0% | 0% | 5.4% (2) | 5.4% (2) |
| 4. I brush as well as I should | 1 | 70.3% (26) | 67.6% (25) | 40.5% (15) | 45.9% (17) |
| - | 2 | 21.6% (8) | 29.7% (11) | 29.7% (11) | 40.5% (15) |
| - | 3 | 5.4% (2) | 2.7% (1) | 18.9% (7) | 8.1% (3) |
| - | 4 | 2.7% (1) | 0% | 8.1% (3) | 0% |
| - | 5 | 0% | 0% | 2.7% (1) | 5.4% (2) |
| 5. I control snacking between meals as well as I should | 1 | 13.5% (5) | 10.8% (4) | 13.5% (5) | 24.3% (9) |
| - | 2 | 18.9% (7) | 21.6% (8) | 10.8% (4) | 21.6% (8) |
| - | 3 | 43.2% (16) | 43.2% (16) | 37.8 (14) | 35.1% (13) |
| - | 4 | 16.2% (6) | 16.2% (6) | 18.9% (7) | 8.1% (3) |
| - | 5 | 8.1% (3) | 8.1% (3) | 18.9% (7) | 10.8% (4) |
| 6. I consider my dental health to be important | 1 | 67.6% (25) | 81.1% (30) | 51.4% (19) | 64.9% (24) |
| - | 2 | 21.6% (8) | 10.8% (4) | 21.6% (8) | 18.9% (7) |
| - | 3 | 8.1% (3) | 8.1% (3) | 13.5% (5) | 8.1% (3) |
| - | 4 | 2.7% (1) | 0% | 10.8% (4) | 2.7% (1) |
| - | 5 | 0% | 0% | 2.7% (1) | 5.4% (2) |
Table 2 Responses to the PEMAT questionnaire among participants in Group III.
| PEMAT Questions | Group 3 n=15 |
|---|---|
| Understandability | - |
| 1. The material makes its purpose completely evident | 100% (15) |
| 2. The material uses common, everyday language | 86.7% (13) |
| 3. Medical terms are used only to familiarize audience with the terms. When used, medical terms are defined | 86.7% (13) |
| 4. The material uses the active voice. (The active voice is when the subject performs the action it expresses e.g., The doctor will give you the prescribed medication) | 93.3% (14) |
| 5. The material breaks or "chunks" information into short sections. | 100% (15) |
| 6. The material’s sections have informative headers | 93.3% (14) |
| 7. The material presents information in a logical sequence. | 100% (15) |
| 8. The material provides a summary | 100% (15) |
| 9. The material uses visual cues (e.g., arrows, boxes, bullets, bold, larger font, highlighting) to draw attention to key points. | 86.7% (13) |
| 10. Text on the screen is easy to read. | 100% (15) |
| 11. The material uses illustrations and photographs that are clear and uncluttered. Actionability | 93.3% (14) |
| 12. The material clearly identifies at least one action the user can take. | 100% (15) |
| 13. The material addresses the user directly when describing actions | 93.3% (14) |
| 14. The material breaks down any action into manageable, explicit steps. | 100% (15) |
The study demonstrated an approach to patient education using a video-based case presentations that was presented to patient groups and a health professional group.
The findings revealed that pre-test mean score and post-test mean score did not differ significantly among patients who have experienced prior professional oral health care (Group I) (p=0.113). However, implementation of video- based case presentations resulted in a statistically significant difference seen in the pre-test mean score and the post-test mean score of the patients who never experienced prior professional oral health care (Group II) (p=0.032). Unpaired t-test also revealed a statistical significant difference in the post-test mean scores of the patients who experienced prior professional oral health care (Group I) versus the patients who never experienced prior professional oral health care (Group II) (p=0.05) after implementation of video-based case presentation patient educational materials.
The findings support the use of video-based case presentations to the patient communities who have minimal access to professional oral health care. The lack of a significant difference in the group of patients who experienced professional oral health care shows that the video-based case presentations has no significant impact on patient communities who have excellent access to professional oral health care. The statistical significance reported on the post-test phase of Group I patients who have experienced professional oral health care and the Group II patients who never have experienced professional oral health care. This confirms that the greater change in planned behavior after the video-based case presentation intervention affected the no prior professional oral health care. The modification of a behavior towards oral hygiene is evident. The modification led to a significant reduction in dental neglect. A study regarding oral health literacy, self-efficacy, and dental neglect, shows that lower self-efficacy is strongly correlated to dental neglect (45). In the context of self-efficacy, autonomy allows the patient to choose from the health care provider’s recommendations (46,47). The motivational aspect of the video-based case presentations has limited details, but it may have an impact on the modification of behavior (48). The impact of dental neglect is considerably significant to oral health (49). The importance of an effective patient education material that aims to reduce dental neglect is evident in this study. The use of a dental neglect related scale is strongly considered in the study of dental patient education.
The understandability score and actionability score reported by the health professional group (Group III) are relatively high (94.54% and 97.78%, respectively). In another study done by Vishnevetsky et al. (44), 30 patient education materials have undergone evaluation using the PEMAT-A/V tool. The result shows a median and interquartile range (IQR) of an understandability score of 83.1% and an actionability score of 100%. The understandability score of the video-based case presentations reported by the third group shows that a higher score is seen when compared to the understandability score of the 30 patient education material. However, the actionability score of the d se, when compared to the actionability score of the 30 patient education material, shows a lower score but is still relatively high. In another study done by Wang et al. (50), 54 patients underwent a pre-test and post-test study regarding video- based patient educational tools regarding common prostate health terminologies. The video-based tool included an explanation of medical terms in a clinical context. They have recorded a significant difference with patients who have low-literacy comprehension. This study recorded significant improvement regarding patients who never went to oral health care professionals. In comparison to this study and the mentioned study done by Wang et al. (50), a video-based educational tool with clinical information is an effective educational tool. The difficulties encountered during the implementation of research instruments include an unfavorable schedule of the patients, uncooperative patients, and unfavorable schedules of the health care professionals. Some patients who have busy schedules did not participate because they have either work, school, or personal affair priorities. The health professionals did have busy work schedules that resulted in multiple appointments that eventually made the experts participate in the study. This study proposes to dental practitioners to use and utilize a video-based case presentations as a patient education tool to their patients who never have experienced professional oral health care. The model, as presented by this study, shows support in reducing dental neglect. The study recommends further study regarding the video-based case presentations and experienced professional oral health care. Patients deserve excellent quality dental care. Pre-operative orientation must always be considered to deliver an excellent dental practice. The potential of the dental neglect scale as a diagnostic tool is considerable. This study proposes to dental educators and researchers to use and utilize a video-based case presentations as an educational medium because it is effective in the dissemination of information to patients. Video-based case presentations shows that alternative option in patient education methods gives practitioners in dental medicine more modified options for patients who never experienced professional oral health care. This study may be used by other educators and researchers for further studies and development of educational learning medium, specifically patient educational tools.
CONCLUSION
The study showed that the video-based case presentations is an effective patient education strategy for dental patients who have never experienced prior professional oral health care. Furthermore, the findings of the study suggest that the inclusion of case presentations in a video format patient education to significantly reduce the degree of dental neglect. The Dental Neglect Scale is an appropriate tool to determine change in patient behavior of dental neglect among dental patients exposed to dental education interventions. The need for professional evaluation of patient education materials is also important in the development of effective patient education materials.