INTRODUCTION
Composite resins are restorative materials frequently used in restorative dentistry and have advantages such as improved esthetic-mechanical properties and controllable curing time. However, the volumetric shrinkage that occurs during polymerization is an important problem about these materials (1). Stress caused by shrinkage can cause marginal defects, enamel fractures, cuspal movements, and cusp fractures.These situations may subsequently cause microleakage, postoperative sensitivity, and secondary caries, respectively (2). Shrinkage stress can be affected by many factors such as cavity configuration (C-factor, cavity size, compliance of the cavity wall), material properties (polymerization shrinkage, matrix formulation, filler content, elastic modulus, the viscosity of the resin), and restoration technique (horizontal incremental pattern, oblique incremental pattern, bulk-fill) (3,4). Conventional resin composites should be placed in increments of up to 2mm to achieve aceptable resin properties and reduce shrinkage stress (5). However, this technique has some disadvantages, such as intermediate layer contamination, difficulty maintaining isolation, and increased operational time (6). Clinicians prefer simple approaches to save time and reduce the possibility of failure. Recently, bulk-fill composites have been manufactured to provide similar shrinkage stresses obtained with conventional incrementally placed composites but can be applied in thicker amounts, such as 4 to 5mm (7). Different photoinitiator ingredients and increased translucency of bulk-fill composites have provided a deeper cure and additional light penetration (8). Stress-relaxant polymerization modulators, prepolymer stress relievers, and high-molecular-weight base monomers have been incorporated in bulk-fill materials to minimize stress formation in restorations (9).
Material composition is as important as filling techniques to minimize polymerization shrinkage and its clinical effects (10). For this purpose, restorative materials with different compositions were produced. One of these is ormocer-based composite materials (Organic-Modified Ceramics), which have larger three-dimensional cross-linked ceramic polysiloxane monomer, and this structure provides less polymerization shrinkage (11). Another restorative material manufactured to reduce shrinkage stresses is short fiber-reinforced composites, which can be applied in bulk (4mm) with hardness close to dentin hardness (12). These materials containing less than 1wt% aluminoborosilicate glass are recommended as a base filling in large cavities and high-stress- bearing areas (13).
While some previously reported studies advocated that the bulk-fill resin composites exhibit lower contraction rates and polymerization contraction stress than conventional composite materials (14,15), others have demonstrated that in terms of shrinkage stress development, bulk fill has no advantage over conventional nanohybrid composites (16). Contraction stresses are influenced by many factors such as the composition and filler content of the resin composite, its ability to flow, and its elastic modulus (17). The fact that bulk-fill resin composites have different physical properties due to handling characteristics and varied composition, and conflicting results in the literature justifies further investigations on this matter. Therefore, this study was designed to determine the failure load of teeth restored using different resin composites in class II cavities. The null hypothesis is that; there will be no differences between the tested materials in terms of failure load.
MATERIAL AND METHODS
SAMPLE PREPARATION
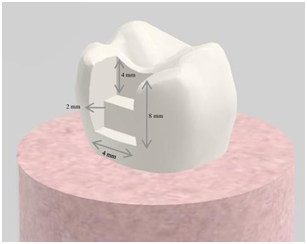
Fifty non-carious third molars with a buccolingual width of 10.5 (±0.5) mm were used for the study. The teeth were stored in 0.5% chloramine solution at + 4°C for no longer than one month until the study started. Dental surfaces were examined with a stereomicroscope (Nikon, Tokyo, Japan) at ×2 magnification to ensure no caries or intrinsic discoloration. Standard class II cavities were prepared using a flat-ended diamond fissure bur (6837-016) underwater cooling with a high-speed rotating tool. Cavity preparation was schematized in Figure 1. A new bur was used for each cavity. The inner edges of the cavities were rounded to reduce the C factor, and dimensions were confirmed with the aid of a periodontal probe. A single operator prepared all cavities, and another researcher confirmed the pre-restoration preparation parameters to ensure continuity and accuracy.
RESTORATIVE PROCEDURE
The properties and application steps of the materials used in the restoration procedure are given in Table 1. Before each restoration, 37% phosphoric acid etching gel (Total etch; Ivoclar, Vivadent AG, Schaan, Liechtenstein) was applied on enamel and subsequently on dentin; and allowed a reaction time of 15 seconds and then G-Premio Bond (GC, Tokyo, Japan) was applied to the cavity walls. After drying with low-pressure air spray, it was polymerized using a LED light source with 1000 mW/cm² standard power (Valo Cordless, Ultradent, South Jordan, UT, USA). A universal matrix band (Protect, Germany) was used to build up the proximal walls using the relevant composite resin of each group. The sample size was estimated based on a previous study conducted with Akbarian et al. (1). Samples were divided into 6 groups (n=10) according to the restorative material to be applied.
Group Control: intact teeth.
Group FI: Bis-GMA based nano filled composite ((Filtek Ultimate, 3M Oral Care, St Paul, MN, USA), (oblique layering incremental technique)) was incrementally applied with 2mm increments in each placement and light-cured for 20s to each layer.
Group EX: Fiber-reinforced composite (EverX Posterior, GC, Tokyo, Japan) was applied in bulk (4 mm) and light-cured for 10s. Then it was applied in 2mm more until for covering dentin and light- cured for 5 seconds. The remaining 2mm cavity was restored with Bis-GMA based nano filled composite as in group FI.
Group FB: Bulk-fill Bis-GMA based composite (Filtek Bulk Fill Posterior, 3M Oral Care, St Paul, MN, USA) was used for restoration in bulk (4mm), and the occlusal, buccal, and lingual surfaces of the material were light-cured for 10 seconds each. The increments were applied in two layers.
Group AB: Bulk-fill Ormocer based composite (AdmiraXtra Fusion, VOCO, Cuxhaven, Germany) was used for restoration in bulks (4mm) and light- cured 20 seconds each layer.
Group TB: A glass containing resin-based composite (TetricEvoCeram® Bulk Fill, Ivoclar, Vivadent AG, Schaan, Liechtenstein) was used for restoration in bulks (4mm) and light-cured 10 seconds to each layer. Finishing and polishing procedures of all restorations were performed 10 minutes after placing the composite resins.
PERIODONTAL LIGAMENT AND ALVEOLAR BONE SIMULATION
The root surface of each tooth was immersed into molten wax up to 2.0mm below the enamel- cement connection to obtain a 0.2 to 0.3mm thick wax layer to simulate the alveolar bone and periodontal ligament. The teeth were embedded in self-curing acrylic resin (Imicryl SC, Konya, Turkey) through cylindrical teflon molds. After resin polymerization, the teeth were removed, roots were cleaned and replaced using polyether impression material (Impregum Soft; 3M Oral Care, St Paul, MN, USA) (7,18).
MECHANICAL TESTING AND FRACTURE ANALYSIS
All samples were stored in distilled water at 37 °C for 24 hours. Fracture testing was immediately performed with a Universal Testing Machine (Shimadzu, Tokyo, Japan) after the teeth were removed from the distilled water. A stainless- steel ball-shaped tip (6 mm diameter) was placed on the central to the restoration's occlusal surface, applied parallel to the long axis of the teeth. Load was applied with a crosshead of 1 mm/min, and the maximum load was recorded in Newton until failure occurred.
FAILURE MODE
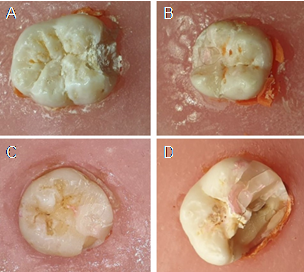
All specimens were evaluated to determine failure mode, and this failure was classified as mode I (fracture in restorative material), mode II (fracture in tooth and restoration), mode III (fracture of one cusp, intact restoration), and mode IV (longitudinal fracture, unrestorable), (Figure 2).
Table 1 Restorative materials used in the study.
| Material | Type | Composition/ resin matrix | Filler | Manufacturer instructions | Filler load Wt% | Manufacturers |
| Total etch | Etching system | %37 Phosphoric acid gel | - | Application 10-15s Wash 5s Dry 5s | - | Ivoclar, Vivadent AG, Schaan, Liechtenstein |
| G-Premio Bond | Adhesive system | 4-MET, 10-MDP, MDTP, phosphoric acid ester monomer, | - | Application 10sDry 5 s light cured 10s | - | GC, Tokyo, Japan |
| Filtek Ultimate (FI) | Nanofill composite | Bis-GMA, UDMA, TEGDMA, bis-EMA, PEGDMA, | silica/zirconia cluster filler, (0.6-10 μm), zirconia particles (4-11nm) | 2mm layers, light cured 20s | %78.5 | 3M Oral Care, St Paul, MN, USA |
| EverX Posterior (EX) | Short Fiber-reinforced bulk-fill composite | BisGMA, PMMA, TEGDMA, Short E-glass fiber filler, barium glass | Silicon dioxide (max. 5 wt%), Barium glass (max. 70 wt%) E-glass fiber (max. 15 wt%) | 4mm layers, light cured 10s | Average filler load 67.7 Average glass fiber load 8.6 | GC, Tokyo, Japan |
| Filtek Bulk Fill Posterior (FB) | Nanofill bulk-fill composite | UDMA, BISGMA, EBPADMA, DDDMA procrylate resin, : Silane-treated ceramic and YbF filler | Zirconia/silica: 0.01-3.5 μm Ytterbium trifluoride: 0.1-5.0 μm | 4mm layers, light cured 30 s (whole time divide by three faces) | 64.5 | 3M Oral Care, St Paul, MN, USA |
| Admira Xtra Fusion (AB) | Nano-hybrid ormocer based bulk-fill composite | Ormocer resin | Fillers and resin matrix based purely on silicon oxide,(no content of classic monomers) | 4mm layers, light cured 20 s | %84 | VOCO, Cuxhaven, Germany |
| Tetric EvoCeram® Bulk Fill (TB) | Nano-hybrid bulk-fill composite | BisGMA, UDMA | Barium-alumino-silica, spherical mixed oxide, prepolymer filler (ytterbium trifluoride, glass filler, and monomer 17 wt%) | 4mm layers,light cured 10 s | %80 (with 17% prepolymers) | Ivoclar, Vivadent AG, Schaan, Liechtenstein |
4-MET: 4-(2-(methacryloyloxy)ethoxycarbonyl) phthalic acid, MDTP: 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine, 10-MDP: 10-methacryloyloxydecyl dihydrogen phosphate, Bis-GMA: bisphenol A glycol dimethacrylate, UDMA: urethane dimethacrylate, TEGDMA: triethyleneglycol dimethacrylate, bis-EMA: bisphenol A ethoxylate dimethacrylate, PEGDMA: polyethylene glycol dimethacrylate, PMMA: Polymethyl methacrylate, EBPADMA: ethoxylate bisphenol A dimethacrylate, DDDMA:1,12-dodecane dimethacrylate.
STATISTICAL ANALYSIS
All analyses were performed using a statistical software package (SPSS, version 22.0, SPSS, Inc., Chicago, IL, USA). Data represented normal distribution according to both Kolmogorov- Smirnov and Shapiro-Wilk tests. Also, it was observed that the variances were homogeneous according to Levene Statistic (p=0,599 for based on mean). Therefore, one-way ANOVA and Post Hoc Tukey’s tests were used to determine the differences between the groups. Significance was set to <0.05.
RESULTS
The mean load and standard deviations of the specimens were presented in Table 2. According to the results, the fracture resistance of the FI group was significantly lower compared to the other groups (p<0.05), and the EX group showed the highest fracture resistance; however, there were no statistically significant differences between control, EX, FB, and TB groups (p>0.05). Furthermore, FB, AB, and TB groups were statistically similar (p>0.05).
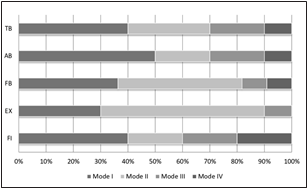
The percentage of failure modes were presented in Figure 3. Mode I and mode II failure types were predominant in all groups. Additionally, mode IV failure had never seen in the EX group.
Table 2 Fracture resistance of experimental groups.
| Group | N | Mean (std) (N) | Min/ Max(N) | Confidence interval (%95) | Group |
|---|---|---|---|---|---|
| - | - | - | - | Lower bound | Upper bound |
| Control | 10 | 2124.90 (248.69)ᵃᵇ | 1838.00/2650.00 | 1946.99 | 2302.80 |
| FI | 10 | 1117.20 (360.03)ᵈ | 711.00/1901.00 | 859.64 | 1374.75 |
| EX | 10 | 2223.40 (451.88)ᵃᵇ | 1477.00/3104.00 | 1900.13 | 2546.66 |
| FB | 10 | 2024.70 (285.01)ᵃᵇᶜ | 1664.00/2426.00 | 1820.81 | 2228.58 |
| AB | 10 | 1621.90 (244.82)ᶜ | 1257.00/1996.00 | 1446.76 | 1797.03 |
| TB | 10 | 1764.50 (277.79)ᵇᶜ | 1443.00/2183.00 | 1565.77 | 1963.22 |
Different letters mean a statistically significant difference (p≤0.05).
DISCUSSION
The posterior teeth are the most affected by the occlusal loads. Restorative procedures cause deterioration of enamel continuity and decrease the resistance of teeth to fracture. In particular, restorations involving more than one-third of the intercuspal distance are even more susceptible to cusp fracture (19). Therefore, the fracture resistance of restorative materials is clinically very important. Composite resins which are routinely used for tooth restoration have the disadvantages of polymerization shrinkage (20). Shrinkage stress' development depends on the stiffness of the composite at the time of shrinkage and the volumetric shrinkage strain. To reduce the net effect of polymerization shrinkage and to ensure a full depth of cure, it is usually recommended to apply the composite in 2mm increments and polymerize each increment independently (21). However, our results revealed that despite the use of incremental technique, the lowest failure load was obtained from the teeth restored with conventional Bis-GMA resins. Thus, it can be assumed that using advanced materials seems to have priority rather than placement technique. Therefore, composites having novel photoinitiators, different matrix formulations, and filler contents have been introduced to improve physical properties (22). Several materials have been manufactured for this purpose. One of these materials is fiber-reinforced composites, consisting of short glass fibers (1-2mm) and barium glass filler (23). Previous studies revealed that these materials show higher compressive strength (24), flexural strength, flexural modulus (24,25), fracture resistance (26), lower polymerization shrinkage (27), and microleakage (28) compared to other resin materials. In the present study, teeth restored with fiber-reinforced composite showed the similar fracture resistance to the level of intact teeth. This indicates the modulus of elasticity homogeneity between restorative material and tooth. Because modulus of elasticity is responsible for how a material would manage the internal tensions produced by forces received externally. It has been reported that direct composite restoration applications, especially in large cavities, showed high fracture resistance but caused non-reparable fractures in teeth (29). This phenomenon occurs mainly because of the remaining tissue in large cavities, which may be mostly enamel. Although the enamel is more resistant than most resin composites, it is more brittle than dentin and resin composites because of its higher elasticity modulus. A recent study, using the EverX posterior to the restoration of molars, regardless of whether they were endodontically treated or not, showed improving fracture resistance and fracture manner (30). These results can be attributed to the physical properties of fiber-reinforced resins mentioned above. This was also verified by the study of Garoushi et al. (31), who stated that glass fibers might increase the material's hardness and its resistance to flexural forces, which enables the material to be used in high-pressure posterior areas and large cavities. Vallittu et al. (32) reported that fiber- reinforced composites avoid propagation of cracks, which subsequently lead to fractures. According to our results, placing fiber-reinforced composites as a bulk under composite restoration seems more advantageous than bulk-fill composites. We assume that short glass fibers dispersed in EverX posterior provided more resistance than increased filler content of bulk-fill ones.
Bulk-fill composites have been produced to facilitate application and shorten the application time due to not requiring incremental placement. These monoblock resins were classified as a single layer (full body) and two layers (base) (33). So-called two layers (base) are the ones constructed by resin materials covering fiber-reinforced composites, which corresponds to our EX group, which was discussed in the previous section. FB, TB, and AB groups are full-body bulk-fill composites with high ratio inorganic filler leading to increased viscosity (34). Clinical and laboratory studies report that bulk-fill resin composites can be applied successfully in large restorations (2,35,36,37,38). In the present study, all of the bulk-fill composites improved the failure load of teeth compared to conventional Bis-GMA based one, presumably resulting from their increased filler volume content and reduced polymerization shrinkage (39).
Differences in the type of resin composite and matrix resin, molecular mobility, size of filler particles, and surface treatment of fillers may affect the mechanical properties of the material (26). It has been advocated that Ormocer-matrix (AB in the present study) may exhibit lower polymerization shrinkage, wear, and monomer leakage due to larger monomer molecules (40). Although AB and TB groups have high filler loading materials used in this present study, fracture resistance values of the groups are relatively lower than the other bulk-fill resin composites. The use of pre-polymerized filler particles, such as in the TB group, has been reported previously to result in lower mechanical properties (41). Besides, Shimokawa et al. (42), Tetric EvoCeram, and AdmiraFusion Xtra (TB and AB groups of the present study) showed more wear compared to Filtek Bulk Fill Posterior (FB in the present study). Although the present study does not evaluate the wear resistance of the tested materials, improvements in the physical properties of materials include a decrease in wear resistance and polymerization shrinkage and an increase in strength. In other words, one of the physical behaviors can be considered as an indicator for others. Although FB seems to be more disadvantageous in terms of filler volume content than AB and TB groups, it shows similar fracture resistance to the EX group in the present study. It may be explained by; contains zirconium (43), to the dispersion of load stress because of the interaction between the resin matrix and fillers through silane coupling or presence of 1,12-dodecane dimethacrylate (DDDMA) which increases molecular mobility, and by this way provides a fast cure, flexibility and improved surface characteristics to the polymer matrix (44).
According to the present study results, the failure load of teeth restored with fiber-reinforced and bulk-fill composites was higher than the restored with conventional one. Thus, the null hypothesis was rejected. Previous studies discuss the importance of simulated periodontal ligament to more closely simulate clinical conditions and establish the absorption of masticatory forces by periodontal ligaments and alveolar bone in vitro (7, 45). Moreover, in our knowledge, this is the first study comparing different restorative materials with the periodontal simulation method.
CONCLUSION
Within the limitations of the present study, the failure load of teeth restored with fiber-reinforced and bulk-fill composites were higher than the restored with conventional one. Therefore, the use of bulk-fill composites may be recommended for the restoration of class II cavities of posterior teeth. However, there is a need for extensive clinical studies evaluating different parameters.