INTRODUCTION
The physical and chemical properties of composite resins used in dental restorative treatments have been improved by manufacturers (1). Polymerization shrinkage observed in composite resins results in stress between the dental tissue and the restorative material. When this stress exceeds the bonding strength between the dental tissue and the composite resin, adhesion fails (2). Applying resin layers of 2mm thickness into the cavity is an option to reduce polymerization shrinkage but it is a difficult and time-consuming process which is likely to be contaminated by the saliva (3).
The adverse effects of the layering technique eventually led to the invention of bulk-fill composite resins.These composites contain new photoinitiators, more translucency filler, and new-resin monomer systems (4). These inorganic fillers reduce light radiation in the organic matrix interface, which enables high levels of light transmittance and polymerization depth. When applied as a single layer of 4-5mm thickness, bulk-fill composite resin exhibits less polymerization shrinkage compared with the conventional composite resin (3,5,6).
In order to improve the micromechanical bonding by which the composite resins bond to the dental tissue, the bonding area of the dental tissues must be extended as well. Today, the most common method to achieve this is phosphoric acid etching. However, acid application on dental surfaces may result in sensitivity depending on the proximity of the cavity surface to the pulp (7). The problems and risks of acid application led to the search for different surface preparation methods.
The removal of dental tissues with laser systems and etching of dental surfaces with laser are two recent innovations introduced in dentistry (8). Lasers provide several advantages to the clinician including selective caries removal with minimum tissue loss, less local anesthetic needed, lack of the vibrations and sound of a dental drill, improved patient comfort, and a cavity following laser preparation without a smear layer, which highlighted lasers as an alternative to traditional tooth preparation methods (9). Clinical research showed that pulp was not affected by these applications (10). Therefore, their application has gradually increased in clinics.
CO2 lasers, Nd: YAG lasers and Erbium lasers are used on dental hard tissues (11). There are two types of Erbium lasers used in dentistry: Er: YAG laser and Er, Cr: YSGG laser. Er, Cr: YSGG lasers are frequently used to modify the surface properties of dental hard tissues. The main advantage of these lasers is that they are absorbed by water molecules at the highest level, which in turn enables faster removal of dental hard tissues (12). The effect of laser beams on the dental surface differs with the wavelength and type of the laser (13).
In vitro tests play a crucial role in evaluating the properties of restorative materials (14). In dentistry, many in vitro tests such as shear, microshear, tensile and microtensile tests measure the physical properties of restorative materials (15,16).
The aim of this study was to evaluate the shear bond strength (SBS) of bulk-fill composite resins of high viscosity applied on dental tissues processed with different techniques.
The first null hypothesis of this study was that bulk-fill composite resins applied on dentin tissues would result in a difference in SBS compared with the conventional composite resin group. The second null hypothesis was that there would be no difference between the surface treatments tested with respect to SBS.
MATERIALS AND METHODS
Three different high-viscosity bulk-fill composite resins and one conventional microhybrid composite resin were used in this study. The materials used in this study are presented in Table 1.
SPECIMEN PREPERATION
This study was approved by Ordu University, Clinical Research Ethic Committee (2016/71). A total of 132 human molars were used in this study. Collected permanent molar teeth were freshly extracted due to orthodontic, prosthetic, or periodontal causes were included in the study. The teeth were free of caries, fractures, or restorations. After the extraction, soft and hard tissues remaining on the tooth surface were carefully removed. Following the procedure conducted by Ansari et al. (17) and Misilli et al. (18) the teeth were stored in 0.5% chloramines-T solution for a week. The teeth were then pumiced and washed. Afterwards, the teeth were stored in distilled water at 4°C for less than 3 months until they were used in the study.
The teeth were cut under water cooling to expose the superficial dentine in the mesio- distal direction with a diamond blade (Isomed, Buehler) on an automated sectioning device (Presi Metallography, Mecatoma T180, France). After the teeth were rinsed again, they were mounted in acrylic resin with their occlusal surfaces facing upwards, using cylindrical molds (2cm × 3cm × 5cm). Afterwards, the dentin surfaces were wet ground with 100 and 600-grit silicon carbide (SiC) paper (18,19,20,21).
The specimens were divided into three groups according to the surface preparation techniques applied: Acid Group, Laser Group and the Control Group. Each group was then divided into four subgroups (n=11) according to the type of composite resin to be applied (Table 2)
The dentin surfaces of the teeth in the Acid Group were etched with 32% phosphoric acid (Scotchbond™ Etchant 3 ml, 3M ESPE, St Paul, MN, USA) for 15s, as instructed by the manufacturer. After etching, surfaces were rinsed with tap water for 20s and were dried with air spray.
An Er,Cr:YSGG laser (Waterlase Iplus MD Turbo, Biolase Technology Inc., San Clemente, CA, USA) was used for surface etching of the teeth in the Laser Group. MX9 turbo tip was used for laser etching. The turbo tip was positioned perpendicular to the surface at a 4mm focal distance in non-contact mode (22). The following parametres were used in the “Bondprep” mode for etching: 2.78 μm wavelength (17) 50 Hz repetition frequency, 4.5 W output power (23), 550 PPS pulse frequency, 60% air pressure level and 40% water pressure level.
In order to reveal the difference between SBS resulting from laser and acid etching, the control group was subjected to polishing only with wet silicon carbide papers. This method was used by Yazıcı et al. (9) and Takada et al. (22), as well.
After the etching process was completed, bonding agent (AdperTM Single Bond 2, 3M ESPE, St Paul, USA) was applied, using disposable bonding brushes. It was light cured (EliparTM S10, 3M ESPE, Seefeld, Germany) for 10 s with a light intensity (between 400 and 515 nm) of 1200 mW/cm2.
Teflon molds of 4x4 mm were used to apply composite resins onto the specimens, as Flury et al. did (24). Bulk-fill resin was applied as a single layer of 4 mm thickness into the teflon mold and was light cured (EliparTM S10, 3M ESPE, Seefeld, Germany) according to the manufacturer’s instructions. On the other hand, conventional microhybrid composite resin (FiltekTM Z250) was incrementally fabricated in layers of 2 mm thickness. Prior to the SBS tests, the surfaces of the teeth were prepared before adhesive resin application. The teeth were then polymerized and stored in distilled water at 37 °C in an incubator.
SHEAR BOND STRENGTH TEST
The SBS test for the specimens was conducted with a universal testing machine (Autograph AGS-X, Shimadzu Co, Kyoto, Japan). The specimens were placed on the universal testing machine with a specially designed metal apparatus, which had a chisel, to fix the specimens in three dimensions. The crosshead speed was 0.5 mm/min as set by Ansari et al. (17). The machine was operated in non-contact mode at minimum focal distance from the surface. The SBS values, which were originally expressed in Newtons (N), were divided by bonding surface area and, were calculated in Megapascals (MPa).
Table 1 Composition of the materials used in the study.
| Material | Composition | - | - | - | Manufacturer and Serial |
|---|---|---|---|---|---|
| - | Organic Matrix | Inorganic Filler | Filler Ratio wt.% | Colour | - |
| Tetric® N-Ceram Bulk Fill | Bis-GMA, Bis-EMA, UDMA | Barium glass, prepolymer, ytterbium trifluoride | 75-77 | IVB | Ivoclar Vivadent, Schaan, Liechtenstein V12515 |
| X-tra fil | Bis-GMA, UDMA, TEGDMA | Barium boron aluminum silicate glass. | 86-70 | U | VOCO, Cuxhaven, Germany 1601243 |
| FiltekTM Bulk Fill Posterior | AUDMA, AFM, UDMA, and 1,12-DDMA | Zirconia/silica cluster filler, ytterbium trifluoride filler. | 76.5 | A2 | ESPE, St Paul, MN, USA N753784 |
| Filtek™ Z250 | Bis-GMA, Bis-EMA, UDMA, TEGDMA | zirconia/silica, Non-agglomerated/ non-aggregated 20 nanometer surface-modified silica particles | 82 | A2 | ESPE, St Paul, MN, USA N612848 |
| Adper™ Single Bond | Ethyl alcohol 25-35%, bisphenol A diglcidyl ether dimethacrylate 10-20%, silanized silica (5 nm with nano-filler) 10-20%, HEMA 5-15%, glycerol 1.3- dimethacrylate 5-10%, acrylic and itaconic acid copolymer 5-10%, diurethane dimethacrylate 1-5%, water <5% | - | - | - | ESPE, St Paul, USA N750012 |
Bis-GMA), Ethoxylated bisphenol A glycol dimethacrylate (BIS-EMA), Urethane dimethacrylate (UDMA), Triethylene glycol dimethacrylate (TEGDMA), Aromatic dimethacrylate (AUDMA), Additional fragmentation molecules (AFM) Urethane dimethacrylate (UDMA), and 1, 12-dodecane-dimethacrylate (DDMA), 2hydroxyethyl methacrylate (HEMA).
Table 2 Study groups and surface treatment techniques.
| Group | Surface Treatment Technique | Number of Samples | Subgroups | Number of Samples(n) |
| Acid | Scotchbond™ Etchant 3 ml (Phosphoric Acid) (3M ESPE, St Paul, MN, USA) (Content: 32% Phosphoric Acid, Application Time: 15 sec) | N=44 | x-tra fil | n=11 |
| - | - | - | FiltekTM Bulk Fill Posterior | n=11 |
| - | - | - | Tetric® N-Ceram Bulk Fill | n=11 |
| - | - | - | FiltekTM Z250 | n=11 |
| Laser | Waterlase Iplus MD Turbo (Biolase Technology Inc., San Clemente, CA, USA) Er,Cr:YSGG Laser, MX9 Turbo Headpiece Bondprep Mode (Power: 4.50 W, Repetition Frequency: 50 Hz, Mode: H, Air Cooling: 60%, Water Cooling: 40 | N=44 | x-tra fil | n=11 |
| - | - | - | FiltekTM Bulk Fill Posterior | n=11 |
| - | - | - | Tetric® N-Ceram Bulk Fill | n=11 |
| - | - | - | FiltekTM Z250 | n=11 |
| Control | No surface treatment | N=44 | x-tra fil | n=11 |
| - | - | - | FiltekTM Bulk Fill Posterior | n=11 |
| - | - | - | Tetric® N-Ceram Bulk Fill | n=11 |
| - | - | - | FiltekTM Z250 | n=11 |
STATISTICAL ANALYSIS
The data obtained from the study were evaluated with Two-Way Analysis of Variance (ANOVA) for SBS. According to Power and Sample Size Test, the sample size was determined as five for each group according to the sample size (α =0.05) and 95% test power, similar to the in-vitro study by Usumez et al. (25). A total of 132 (12x11) specimens were included in the study for possible problems.
The data collected in this study were first evaluated for normality using Shapiro-Wilk normality test (SPSS version 15.0; SPSS, Inc., Chicago, IL, USA). The data were then evaluated with Two-Way Variance Analysis. Tukey’s HSD Multiple Comparison test was used to compare differences among the mean values of the groups.
RESULTS
The bond strength values had a normal distribution for the composite resin types and surface treatment methods used in the study (P>0.05) (Table 3). Table 4 and Table 5 show the mean bond strength values and standard deviations in MPa.
The variance analysis applied on the data showed statistically significant differences among the surface treatment methods for SBS values (P<0.001).
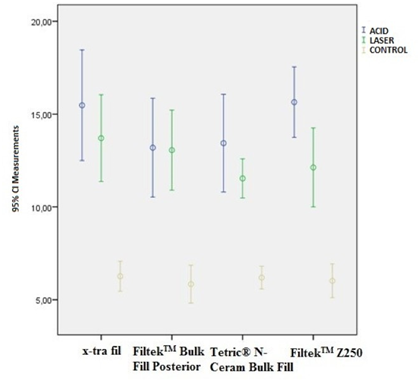
Figure 1 presents the SBS values of the composite resins for surface preparation methods. On the other hand, there was no statistically significant difference between the composite resin materials (P=0.199) and the K*U interaction groups (P=0.449) for SBS values. Figure 2 shows the comparison of different surface preparation methods applied for each composite resin material.
The highest SBS values were detected on acid-etched specimens. Of these, Filtek™ Z250 (3M ESPE, St Paul, MN, USA) had the highest SBS (15.64 ± 2.82 MPa). As for the bulk-fill composite resins, the highest SBS value (15.48 ± 4.44 MPa) was found in X-tra fil (VOCO, Cuxhaven, Germany). However, there were no statistically significant differences among the composite resin types with respect to SBS values (P=0.449).
The laser-etched specimens had statistically significant lower SBS values compared with those of the acid-etched specimens (P<0.001). Of all the laser-etched specimens, X-tra fil (VOCO, Cuxhaven, Germany) showed the highest SBS (13.70 ± 3.48 MPa). The laser-etched group had statistically significant higher SBS values compared with those of the control group which was not subjected to any surface preparation (P<0.001).
There were no statistically significant differences among the composite resin types with respect to the SBS values neither in the laser- etched group nor the control group (P=0.449).
Table 3 Shapiro-Wilk normality test results.
| - | Kolmogorov-Smirnovª | - | - | Shapiro-Wilk | - | - |
|---|---|---|---|---|---|---|
| Group | Statistic | df | Sig. | Statistic | df | Sig. |
| Tetric® N-Ceram Bulk Fill | .125 | 33 | .200* | .903 | 33 | .006 |
| X-tra fil | .117 | 33 | .200* | .936 | 33 | .053 |
| Filtek™ Bulk Fill Posterior | .107 | 33 | .200* | .968 | 33 | .429 |
| Filtek™ Z250 | .159 | 33 | .034 | .941 | 33 | .075 |
*. Lower bound for statistically significant difference. ª. Lilliefors Significance Correction.
Table 4 Tukey’s Multiple Comparison Test Results
| - | Surface Preparation Methods | - | - | - |
|---|---|---|---|---|
| Composite Resins | Acid | Laser | Control | General |
| X-tra fil | 15.48 ± 4.44 | 13.70 ± 3.48 | 6.27± 1.20 | 11.81 ± 5.18 |
| Filtek™ Bulk Fill Posterior | 13.19 ± 3.96 | 13.06 ± 3.21 | 5.84 ± 1.52 | 10.70 ± 4.58 |
| Tetric® N-Ceram Bulk Fill | 13.43 ± 3.92 | 11.54 ± 1.57 | 6.19 ± 0.92 | 10.39 ± 3.94 |
| Filtek™ Z250 | 15.64 ± 2.82 | 12.13 ± 3.16 | 6.02 ± 1.35 | 11.26 ± 4.74 |
| General | 14.44 ± 3.87 a | 12.61 ± 2.97 b | 6.08 ± 1.23 c | 11.04 ± 4.61 |
a,b,c show differences among application groups on the same line (P<0.05).
Table 5 Two-Way Analysis of Variance Test.
| Sources of Variation | - | - | - |
|---|---|---|---|
| - | Composite Resin (K) | Application (U) | K*U |
| P-values | 0.199 | <0.001 | 0.449 |
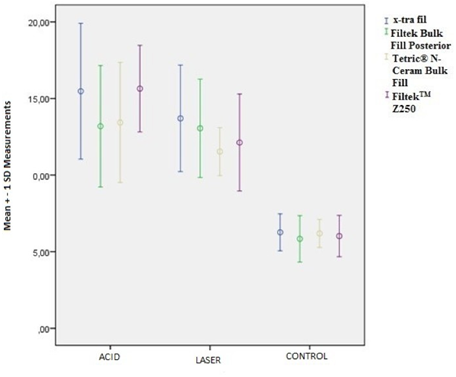
Figure 1. Graphics for composite resins according to surface preparation techniques (Mean ± standard deviation)
DISCUSSION
The variance analysis conducted showed that there was a statistically significant difference between surface preparation techniques with respect to SBS. Of all the composites used in the study, the highest SBS values were found in acid-etched teeth while the lowest SBS values were measured in the control group. Although the laser-applied teeth did not have SBS as high as those of the acid-etched teeth, they still had significantly higher SBS values compared with the control group.
There is no consensus in literature as to the effectiveness of using only laser in surface etching. It was showed that Er,Cr:YSGG laser and Er:YAG laser had similar effects as acid application on teeth tissues, causing no apparent thermal damage and that they formed rough surfaces which might enhance the bond strength of resin-based materials and adhesive restorations (26, 27).
Olivi et al. (28) reported that widening the application surface with a turbo handpiece produced exclusively for Er,Cr:YSGG laser could facilitate the clinical use of Er,Cr:YSGG laser (28).
In this study, a two-step etch-and-rinse adhesive system was used to observe the effect of laser etching of dental surfaces on bonding, as used by Carvalho et al. (29).
A study of the literature revealed that the number of studies evaluating the resin bond strength of dentin-bulk fill composites applied with Er,Cr:YSGG laser including a turbo handpiece is limited.
Takada et al. (22) compared the effectiveness of several bonds on dentin surfaces prepared with laser with a turbo handpiece (MX5). They used only silicone carbide sandpaper in the control group. They found that pretreating the dentin surfaces with phosphoric acid or phosphoric acid and sodium hypochlorite combination prior to Er,Cr:YSGG laser application increased the bond strengths of composite resins (22). This result complies with our findings.
Ansari et al. (17) recommended the use of Er,Cr:YSGG laser in combination with phosphoric acid for cavity preparation or surface etching. Jeevarathan et al. (30) reported that mean SBS of Acid etching Group was significantly higher than the mean SBS of Laser etching Group. The study conducted by Carvalho et al. (29) reported similar results. These findings support our findings.
In a study conducted by Lee et al. (31), it was found out that Er,Cr:YSGG laser irradiation followed by acid-etching increased tensile bond strength as much as bur cut / acid-etched dentine.
Lee et al. (31) also reported that the peritubular dentin which protruded from the surrounding intertubular dentin resulted from the high mineral content and low water content of peritubular dentin. On the other hand, Er,Cr:YSGG laser application followed by acid-etching removed the mineral content of dentin and widened dentinal tubule orifices. After acid-etching, surfaces seemed significantly smooth (31).
Lee et al. (31) found that the bond strength of laser-ablated human dentin was statistically lower than those of other groups. They reported that this might result from the fact that Er,Cr:YSGG laser was not able to selectively remove hydroxyapatite crystallites without any harmful effect on the collagen fiber network. When acid-etching was not applied after laser application on dentin, collagen fiber was not totaly exposed. Therefore, the quality of the hybrid layer was not adequate in laser- ablated dentin (31).
Demineralization occurs during the application of acid on dentin tissues and, removal of hydroxyapatite from intertubular collagen results in orifices within the tissue. Thus, with increased microporosity, the bonding of the adhesive to be applied increases. In addition, it was reported that acid applied on dentin tissue removed the smear layer, ultimately increasing the bond strength (32).
Similar to our study, these studies showed that acid application resulted in better bonding compared with laser etching and that laser application, which can not be an alternative for acid, should be used in combination with acid. However, there are studies (Sung et al. (33)) in literature with different results compared with our study.
As reported by Ansari et al. (17), these discrepancies among the studies may result from the physical parametres of the laser, the material used to fill the cavities or the combination of laser- etched surface with or without acid etching.
In most of these studies, etching was achieved using Er,Cr:YSGG laser with a standard handpiece. The difference between the turbo handpiece and the standard handpiece is that the turbo handpiece, which uses turbo tips with spot diameters of 500, 700 and 900 microns, enables a focal distance of 3-5 mm off the tissue. In the light of this information, new studies comparing conventional lasers with Er,Cr:YSGG lasers with turbo handpieces are required.
In the present study, no statistically significant difference among the composite resin materials for SBS was found, which was similar with the results of Ilie et al. (34), Omran et al. (35) and Seyhan Cezayirli et al. (36).
Moreover, it was observed that filler content increased when translucency decreased. This results from the fact that light transmission is tightly depend on material opacity. Therefore, it can be deduced that the behaviour of bulk fill composites can not be predicted. Bulk fill composites can have a homogenous adhesion interface which can produce highly probable cohesive failure despite increased increment thickness. Accordingly, high mean SBS values of bulk increments can be achieved in comparison with conventional composite resins (35).
Bond strength is affected by many factors such as the type of acid/adhesive used, application time and chemical structure of the dentin (37).
The variants of the shear bond strength test were elasticity module of the restorative material bonded and the diameter of the sample; thickness of the adhesive resin; dentin depth (deep or superficial); type and contact point of the material bonded and speed of the test machine’s blade (38).
The elasticity module values of the restorative materials used in our study are as follows: Dentin (18,6 GPA); Filtek Z 250 (24,494 Gpa), Xtrafil bulk (21,6 Gpa), Filtek Bulk (17,2 Gpa), Tetric N (10 GPA). These values comply with those reported by Mandava et al. (39), Yamanel (40) and Rizzante et al. (41). In general, SBS values found in our study comply with these elasticity module values. Although the SBS values of the composites found in our study differ, these differences are not statistically significant.
Inadequate polymerization can result in excessive residual monomers, problems in bonding, leakage and fractures (42,43).
Benetti et al. (44) found that Tetric EvoCeram Bulk-Fill showed a higher depth of cure compared with the conventional resin composite. In addition, it was reported that bulk-fill resin composites had a higher depth of cure. The difference between the two restorative materials was referred to the developments in their initiator system and increased translucency. As for Tetric EvoCeram Bulk-Fill, the increased depth of cure was achieved with the addition of a new initiator together with the camphoroquinone/amine initiator systems. This new initiator is ivocerin. It effectively increases the depth of cure in Tetric EvoCeram Bulk-Fill in comparison with its regular nanohybrid resin based composite pendant Tetric EvoCeram since the chemical composition and the filler systems in both materials are comparable (21).
Except for the specific properties of the monomer, higher-molecular weight monomer systems usually exhibit a lower decrease of the degree of conversion with increasing incremental thickness in comparison with regular resin composite based on bisphenol-A-dimethacrylate (34). Filtek Bulk Fill consists of a high molecular weight aromatic dimethacrylate (AUDMA) and UDMA (45).
The fact that Tetric N Ceram and Filtek Bulk Fill, despite their low elasticity modules, had similar results as the other composite resins can be explained by these properties.
The commercially available bulk-fill resin composites must be placed in increments of 4mm into deep posterior cavities. This 4mm thickness must be strictly applied in order to avoid significant decreases in SBS values and subsequent adverse effects on dentin bond strength (35).
Misilli et al. (18) reported that bulk-fill composites can be applied in layers of 4mm in spite of the fact that the studied composites had better performance with a thickness of 2mm.
While the higher polymerization depth of bulk-fill composite resins compared with conventional composite resins is achieved with the high translucency of the materials, reduced polymerization stress is associated with improvements in organic matrix and inorganic filler content (46).
Bulk-fill composites had similar bond strengths with conventional composites thanks to their feature which enabled them to be placed in increments of 4mm. The conventional composite resin, on the other hand, is polymerized in increments of 2mm, which prevent a decrease in bond strength.
More in vitro studies supported with clinical data are required to investigate the performance of bulk-fill composites.
There were several limitations in our study. One of our limitations was that thermal cycle was not used to evaluate the long-term results of aging in our study. It was reported that SBS might aslo be affected by thermal cycle. The second limitation of our study was that the laser device was used according to the instructions of the manufacturer. Laser-etching with different parametres of the turbo handpiece might affect the SBS. A third limitation of our study was that scanning electron microscope (SEM) was not used to detect failure modes.
CONCLUSION
Based on the findings of this study, the following conclusions were drawn:
1.Laser etching of the dentin tissues is not as effective as acid etching. An improvement in lasers is required in order to enhance their effect on hard tissues, which in turn can present it as an alternative to acid.
2.As for SBS, bulk-fill composites can be safely used like conventional composites.