Introduction
Craniofacial growth-development has a complex and multifactorial structure(1). Pharyngeal airway; head posture,functional anterior displacement, vertical and sagittal skeletal relationship, can be affected by factors such as maxilla and mandible position (2,3,4,5).
Class II malocclusion is a malocclusion that is frequently encountered with different combinations of skeletal and dental factors and constitutes approximately 1/3 of orthodontic malformations (6). This malocclusion, which may occur as a result of mandibular retrognathia, maxillary prognathia or a combination of both, has been reported to occur mostly from mandibular retrognathia (7). In the case of mandibular retrognathia, the soft palate length and angulation increase, as a result, the upper pharyngeal airway becomes narrower (8). Especially the hypopharynx; it has been reported that individuals with retrognathic mandible are narrower than normal subjects (8).
Airway obstruction has been associated with Class II malocclusion and vertical growth pattern. In many studies, mouth breathing and pharyngeal airway area have been reported to be narrowed in individuals with Class II malocclusion (9,10,11,12,13,14).
In many studies, researchers have examined nasopharyngeal dimensions in individuals with Class I occlusion and Class II malocclusion. As a result of the studies, they reported that the nasopharyngeal areas were wider or similar width in individuals with Class II malocclusion, and the hypopharyngeal and oropharyngeal areas were narrower (10,15,16). In studies using CBCT images, they found that individuals with Class II malocclusion had a narrower oropharyngeal airway size than those with Class I occlusion (16). In a longitudinal study conducted in the prepubertal and postpubertal periods of untreated Class I and Class II patients, the airway volumes of Class II patients were always smaller during the study compared to Class I patients (17).
Schwab et al. reported that mandibular and maxillary retrognathia caused narrowing of the posterior pharyngeal airway (18). Muto et al. found that patients with mandibular retrognathia had smaller oropharyngeal airway measurements than patients with mandibular prognathia in a study in which individuals in the postpubertal period evaluated airway size with lateral cepholametric measurements (19).
Individuals with Class II malocclusion have a narrower anteroposterior pharyngeal size due to mandibular retrognatism, short mandibular corpus and posterior rotation of the mandible. This narrowing of the palate occurs especially in the nasopharynx and the oropharynx. As a result of this narrowing, the tongue will not be in its normal position at rest, so individuals' respiratory functions may deteriorate during the day and there may be potential problems such as snoring, upper respiratory resistance, and obstructive apnea (9).
When the literature is examined, Class II malocclusions have been studied in many studies with other malocclusions in terms of both pharyngeal airway dimension and hyoid bone position. (2,3,4,5,8,9,10,13,14,15,16,17). However, it is limited to studies comparing the pharyngeal airway in the subgroups of Class II malocclusion separated by jaws it originates from. The purpose of this study; to examine pharyngeal airway dimensions and hyoid bone position according to different types of Class II malocclusions.
Materials and methods
Ethical approval for this retrospective study was obtained from the local ethics committee (Clinical Research Ethics Committee, Suleyman Demirel University (Ethics Approval Number: 16.01.2019-7), and informed consent was obtained from the parents of the patients included in the study. Patients with skeletal Class II malocclusion who were treated between June 2018 and June 2019 were divided into 3 subgroups.
The sample size was calculated based on a power analysis using G* Power analysis (G* Power Ver.3.0.10, Kiel, Germany) for superior airway space at alpha error probability of 0.05 and a power of 80% (20). The power analysis showed that a minimum of 21 individuals was required for each subgroup. In order to increase the power of the study more individuals were included in the study.
The inclusion criteria are the absence of any craniofacial anomalies or systemic disorders, no airway pathologies, adequate imaging quality of cephametric radiographs, and no previous orthodontic treatment. Pharyngeal airway dimensions are affected by the head posture. Therefore, those with a faulty head posture in cephalometric radiographs were excluded from the study. The head posture was examined according to vertebral positions and the Frankfort Horizontal plane in cephalometric radiographs. Also in this study, patients over 17 years old and patients with artifacts on their radiographs were excluded from the study. Factors that may affect the airway, such as age, gender, and growth-development period (puberta), were also examined in the groups, and no differences were found between the groups. Therefore, the groups were formed from well-matched individuals with a similar distribution of pubertal status. Out of the 608 patients included in the evaluation, a total of 221 individuals (131 females and 90 males) were included in the study.
ANB° angle was used for grouping according to skeletal malocclusion. Individuals with skeletal Class II malocclusion were divided into three subgroups as maxillary prognathia (SNA>84°)(Group 1; 61 patients), mandibular retrognathia (SNB<78°)(Group 2; 118 patients), and combined (SNB<78° and SNA>84°) (Group 3; 42 patients), and airway measurements and hyoid measurements were compared.
Cephalometric analysis
Linear measurements used in study are in the NemoCeph software program (NX 2009 for Windows, Nemotec, Madrid, Spain), and area measurements in the SketchAndCalc™ software program (SketchAndCalc Area Calculation software, Axiom Welldone ©, https: //www.sketchandcalc. com/) was performed on digital lateral cephalometric films after digital calibration.
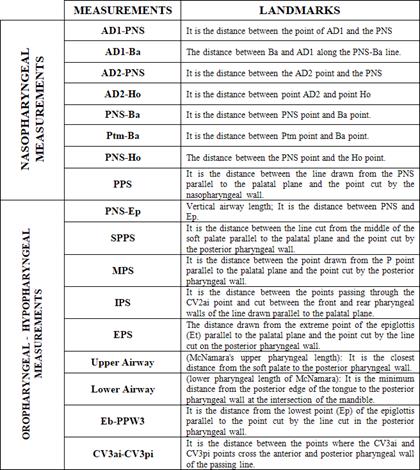
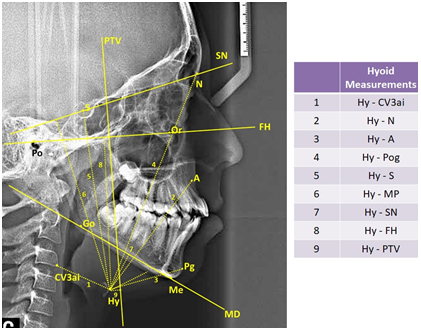
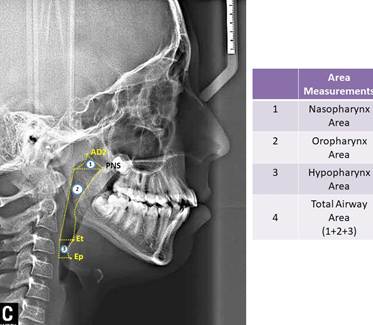
In study, 35 cephalometric points (Figure 1), 8 cephalometric planes, and 30 cephalometric measurements (Figure 2) were used. In the cephalometric analysis; 5 craniofacial, 8 nasopharyngeal, 7 oropharyngeal, 2 hypopharyngeal (Figure 3), 9 hyoid measurements (Figure 4) and 4 area measurements (Figure 5) were used.
Statistical analysis
Kolmogorov-Smirnov test was used to determine whether the data had normal distribution. Since the parameters evaluated in the study were generally distributed homogenously in the subgroups, parametric tests were used.
The distribution of sex and growth- development (CVM-Cervical Vertebral Maturation) stages of the patients were compared with the Pearson chi-square test. In determining the growth and development period, cervical vertebral maturation period was determined by Lamparski method, the lateral cephalometric films taken at the beginning of treatment (21). One-way ANOVA was used to evaluate patients subdivided according to Class II malocclusion. Tukey Post-Hoc tests were used for bilateral comparisons for significant parameters. In order to determine the error margin of the measurements, 55 randomly selected films from 221 lateral cephalometric films were repeated by the same researcher after the first measurements. Cronbach α coefficients were determined for each measurement. Repeatability coefficients were found to be high for each measurement (α≥876).
SPSS package program (SPSS for Win, ver 20.0; SPSS Inc, Chicago, Ill.) was used for data analysis. Results were considered statistically significant at p<0.05 significance level.
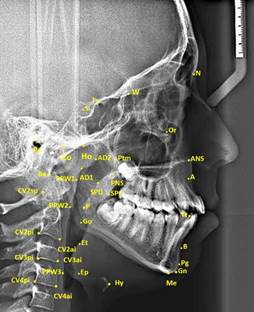
Figure 1 Cephalometric landmarks used in study. (S: It is the geometric center point of Sella tursica; N: It is the most advanced point in the middle oxal plane, where the nasofrontal suture intersects the sagittal plane, and the deepest point of the recess in that area; Ptm: It is the lowest point of the fissure formed by the retromolar tubercle of maxillary and the pterygoid part of the sphenoid bone; PNS: It is the most posterior and end point of the hard palate in the sagittal plane; A: It is the deepest point of concave located between the anterior nasal spina and prosthion; Pg: It is the most advanced point of the mandibular symphysis in the sagittal plane; Ba: The junction between the base of the cranium and the outer edge of the clivus cranium and the endocranium edge; Hy: Hyoid is the top and anterior point of the bone corpus; P: It is the extreme point of the soft palate; Ep: The Epiglottis base is also the most posteroinferior point in the tongue base; Et: It is the end point of the epiglottis; Ho: It is the point at the intersection between the perpendicular line drawn from PNS to the Sella-Basion and the cranial base; AD1: It is the point where the line connecting the PNS and the Basion intersect the posterior of the nasopharyngeal wall; AD2: It is the point at the intersection of the line drawn from the PNS to the midpoint of the line connecting the Sella-Basion and the posterior of the nasopharyngeal wall.)
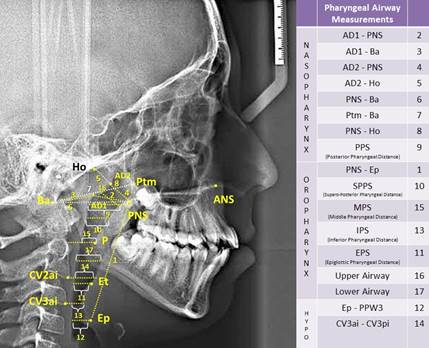
Figure 3 Pharyngeal airway measurements used in study. (PPS: palatal pharyngeal distance: on the line passing from PNS, parallel to FH. SPSS, superior posterior pharyngeal distance: on the line passing from the midpoint of the soft palate, parallel to FH. MPS, middle pharyngeal distance: on the line passing from P, parallel to FH. IPS, inferior pharyngeal distance: on the line passing from cv2a, parallel to FH. EPS, epiglottic pharyngeal distance: on the line passing from E, parallel to FH.)
Results
Distribution of patients with skeletal Class II malocclusion included in the study according to chronological age, gender and growth-development period are shown in (Table 1).
The mean age of 221 patients (131 female and 90 male) with Class II malocclusion was found to be 13.32±2.50 years. 27% of the Class II patients were maxillary prognathia (61 patients; 34 female, 27 male; mean age of 12.92±2.65 years); 54% of the Class II patients were mandibular retrognathia (118 patients; 70 female, 48 male; mean age of 13.49±2.44 years) and 19% of the Class II patients were identified as combined (42 patients; 27 female, 15 male; mean age of 13.40±2.46 years). Most Class II patients (108 patients-48.86%) are in peak growth periods. No significant relation was observed between the types of Class II malocclusion and chronological age, gender and growth-development periods (p>0.05). No difference in demographic data indicates that the groups are well matched even though the group numbers are different.
When the effects of skeletal Class II malocclusion subgroups on the pharyngeal airway were examined, there was no statistically significant difference in the nasopharyngeal, oropharyngeal and hypopharyngeal parts between the skeletal Class II malocclusion types (p>0.05) (Table 2).
In the measurements we evaluated the position of the hyoid bone, a statistically significant difference was found between the three groups in the measurement of Hy-Pg (mm) (p<0.05). Hy-Pg (mm) value was lower in the mandibular retrognathia group than the other two groups. When the Tukey test results were examined, a statistically significant difference was observed between the mandibular retrognathia group and the maxillary prognathia group (p<0.05). Finally, when the area measurements were examined, no statistically significant difference was found between the three groups in all area measurements (p>0.05) (Table 3).
Table 1 Demographic data according to the subgroups of skeletal Class II malocclusion.
| - | - | (Group 1) | (Group 2) | (Group 3) | - | - |
| - | - | Maxillary Prognathia (n=61) | Mandibular Retrognathia (n=118) | Combined (n=42) | TOTAL (n=221) | p |
| Chronological Age †(ẋ± SD) | - | 12.92 ± 2.65 | 13.49 ± 2.44 | 13.40 ± 2.46 | 13.32 ± 2.50 | 0.117 |
| Gender * n (%) | Male | 27 (44.26) | 48 (40.68) | 15 (35.71) | 90 (100) | - |
| - | Female | 34 (55.74) | 70 (59.32) | 27 (64.29) | 131 (100) | 0.686 |
| Growth Development Period *n (%) | Pre-Peak | 12 (19.67) | 24 (20.33) | 5 (11.90) | 41 (100) | - |
| - | Peak | 30 (49.18) | 55 (46.61) | 23 (54.76) | 108 (100) | 0.311 |
| - | Post-Peak | 19 (31.14) | 39 (33.06) | 14 (33.33) | 72 (100) | - |
†: One-way ANOVA test;
*: Pearson chi-square test.
Table 2 Comparison of pharyngeal airway measurements according to the subgroups of skeletal Class II malocclusion.
| - | - | Group 1 Maxillary Prognathia | Group 2 Mandibular Retrognathia | Group 3 Combined | Tukey Post-Hoc Test | - | - | ANOVA |
| - | - | ẋ± SD | ẋ± SD | ẋ± SD | 1-2 | 1-3 | 2-3 | p |
| NASOPHARYNGEAL MEASUREMENTS | AD1-PNS | 23.93±5.18 | 24.10±4.96 | 25.17±5.13 | NS | NS | NS | 0.419 |
| - | AD1-Ba | 21.18±4.05 | 20.60±4.31 | 20.64±4.24 | NS | NS | NS | 0.666 |
| - | AD2-PNS | 18.08±4.16 | 16.44±3.96 | 17.42±4.04 | NS | NS | NS | 0.666 |
| - | AD2-Ho | 10.35±4.05 | 11.02±4.11 | 10.00±3.35 | NS | NS | NS | 0.290 |
| - | PNS-Ba | 44.76±5.66 | 44.38±5.13 | 45.50±4.91 | NS | NS | NS | 0.491 |
| - | Ptm-Ba | 39.70±4.27 | 39.15±3.77 | 40.11±5.12 | NS | NS | NS | 0.400 |
| - | PNS-Ho | 28.77±3.63 | 29.81±3.40 | 30.32±7.47 | NS | NS | NS | 0.185 |
| - | PPS | 25.89±4.92 | 25.22±5.34 | 26.29±5.04 | NS | NS | NS | 0.458 |
| OROPHARYNGEAL MEASUREMENTS | PNS-Ep | 55.57±6.89 | 57.41±6.84 | 56.02±6.76 | NS | NS | NS | 0.192 |
| - | SPSS | 9.50±3.01 | 9.32±2.90 | 9.84±2.73 | NS | NS | NS | 0.604 |
| - | MPS | 12.11±3.59 | 11.34±3.33 | 12.66±3.47 | NS | NS | NS | 0.077 |
| - | IPS | 12.75±3.80 | 12.00±3.73 | 12.67±4.03 | NS | NS | NS | 0.371 |
| - | EPS | 10.92±3.07 | 10.23±3.09 | 10.90±3.51 | NS | NS | NS | 0.286 |
| - | Upper Airway | 6.92±2.62 | 6.93±2.70 | 7.49±2.19 | NS | NS | NS | 0.447 |
| - | Lower Airway | 10.06±3.32 | 9.36±2.81 | 10.46±3.03 | NS | NS | NS | 0.083 |
| HYPOPHARYNGEAL MEASUREMENTS | Ep-PPW3 | 13.99±3.32 | 12.24±3.52 | 14.08±3.70 | NS | NS | NS | 0.286 |
| - | CV3ai- CV3pi | 10.54±3.78 | 9.40±3.23 | 10.48±3.52 | NS | NS | NS | 0.060 |
ẋ:Mean; SD: Standart Deviation; P: One-way ANOVA test; NS: not-significant p>0.05.
Table 3 Comparison of hyoid and area measurements according to the subgroups of skeletal Class II malocclusion.
| - | - | Group 1 Maxillary Prognathia | Group 2 Mandibular Retrognathia | Group 3 Combined | Tukey Post-Hoc Test | - | - | ANOVA | - |
| Hyoid bone measurements | - | ẋ± SD | ẋ± SD | ẋ± SD | 1-2 | 1-3 | 2-3 | p | - |
| - | Hy - CV3ai | 30.13±3.69 | 30.18±3.88 | 32.33±3.17 | NS | NS | NS | 0.711 | NS |
| - | Hy - A | 71.14±7.01 | 70.16±8.75 | 70.52±6.60 | NS | NS | NS | 0.057 | NS |
| - | Hy - Pg | 47.80±6.54 | 43.80±5.91 | 45.13±9.41 | 0.021 | NS | NS | 0.020 | * |
| - | Hy - N | 114.67±8.79 | 116.47±8.79 | 112.45±12.09 | NS | NS | NS | 0.057 | NS |
| - | Hy - S | 43.76±7.19 | 45.41±5.91 | 44.74±6.30 | NS | NS | NS | 0.057 | NS |
| - | Hy - SN | 93.38±9.18 | 94.94±8.40 | 94.74±10.55 | NS | NS | NS | 0.538 | NS |
| - | Hy - MP | 11.62±4.24 | 12.91±4.68 | 11.67±5.55 | NS | NS | NS | 0.141 | NS |
| - | Hy - FH | 74.99±7.23 | 76.01±7.98 | 75.33±9.58 | NS | NS | NS | 0.711 | NS |
| - | Hy - PTV | -1.05±7.61 | -2.48±6.53 | -1.17±5.83 | NS | NS | NS | 0.315 | NS |
| Area measurements | Oropharynx Area | 432.69±139.34 | 427.38±117.28 | 458.86±107.26 | NS | NS | NS | 0.354 | NS |
| - | Nasopharynx Area | 145.29±65.38 | 132.36±59.95 | 143.90±55.24 | NS | NS | NS | 0.319 | NS |
| - | Hypopharynx Area | 210.91±83.31 | 194.57±85.17 | 218.98±73.82 | NS | NS | NS | 0.190 | NS |
| - | Total Area | 788.90±228.10 | 754.32±188.37 | 821.76±173.61 | NS | NS | NS | 0.143 | NS |
ẋ:Mean; SD: Standart Deviation; P: One-way ANOVA test; *p<0.05; **p<0.01; ***p<0.001; NS: Not significant p>0.05.
Discussion
Class II malocclusions are characterized by the prognathic maxilla, retrognathic mandible, or a combination of these two conditions. It is well known that treatment of Class II malocclusion leads to improved respiratory disturbance due to airway obstruction (22,23). According to Balter, the etiology of Class II malocclusion is the positioning of the tongue backwards and causes discomfort in the cervical region (24). This results in mouth breathing. It is emphasized in the literature that the narrowing of the pharyngeal airway space causes changes in the respiratory tract (3,25). Thus, it can be concluded that the variation in the skeletal pattern may predispose to upper airway obstruction (3,24,25).
Although many studies in the literature (26,27,28). Reported that mandible location and skeletal malocclusions affect upper airway dimensions, some studies also noted that skeletal malocclusions did not affect upper airway dimensions (29). Although there is no study comparing all subgroups of Class II malocclusions in terms of the pharyngeal airway in the literature, some limited studies have compared individuals with mandibular retrognathia with Class I and Class III malocclusions (4).
Studies of the pharyngeal airway in Class II malocclusion patients are very limited, and none of the studies showed any difference or correlation between airway size in skeletal Class II patients with prognathic maxilla and retrognathic mandible. Therefore, in this study, it was tried to distinguish the pharyngeal airway relationship between different jaw-borne Class II subjects.
Soni et al. compared the mandibular retrognathia to the maxillary prognathia group and reported a difference in oropharynx measurements as a result of the study (22). However, the disadvantage of the findings of this study is that both hypopharyngeal measurements were not made and combined Class II malocclusions were not evaluated.
Küçükkaraca et al. compared pharyngeal airway measurements in the Division 1 and Division 2 groups of Class II malocclusions. As a result of the study, they reported that the lower airway was narrower than Class I malocclusion in both subgroups of Class II malocclusion (9). Oz et al. and Dincer et al. evaluated Class II malocclusions according to different vertical growth patterns. They stated that there were smaller airway space in patients with high-angle skeletal Class II malocclusions (23,30).
Akcam et al. compared the nasopharyngeal and oropharyngeal airway dimensions of 45 individuals (21 boys, 24 girls) with skeletal Class II malocclusion in prepubertal, pubertal and postpubertal development periods. As a result of the study, it was reported that nasopharyngeal airway dimensions increased with development and oraferangeal airway dimensions remained the same (31).
In the study of CBCT images of 57 male and 44 female between the ages of 14-18, El and Palomo evaluated the position of the airway and the mandible according to the cranium. In the study, patients were examined in five groups as Class I, Class II mandibular retrusion, Class II maxillary protrusion, Class III maxillary retrusion and Class III mandibular protrusion. The oropharyngeal and nasopharyngeal airways were narrower in the Class II mandibular retrusion group, but the same relationship was not found in the Class II maxillary protrusion group (4). In current study, although the oropharyngeal and nasopharyngeal airway dimensions were found narrower in the mandibular retrognathia group, they were not statistically significant.
Sloan et al. examined the position of the hyoid bone and its movements during swallowing in 45 children with an average age of 12 years with Class I, Class II division 1 and Class II division 2 malocclusion. They reported that in children with dental Class I malocclusion, the hyoid bone was positioned lower and lower than the mandible, and higher in children with Class II malocclusion. They stated that the vertical position of the hyoid bone during swallowing mostly changed in the Class I malocclusion group (32). Sarı et al. compared 19 individuals with Class I malocclusion and 19 individuals with Class II division 2 malocclusion and suggested that the hyoid bone was closer to the upper reference planes in the Class II division 2 group (33). In this study, a significant difference was found only in the Hy-Pg value from the measurements we evaluated the position of the hyoid bone. In the mandibular retrognathia group, the distance between Pg point and hyoid was found less due to mandibular deficiency. In measurements other than Hy-Pg, the hyoid position was found to be similar vertically and sagittally in subgroups of Class II malocclusions.
In the current study, CBCT was not used due to reasons such as high radiation dose, unsuitable for routine use and cost. Thus, the findings of the present prospective clinical study should be assessed within the limitations of the two-dimensional radiography design.
From this study we conclude that airway dimensions in the nasopharynx are similar among subgroups of Skeletal Class II malocclusion. Also, airway dimensions in the oropharynx and hypopharynx were decreased in the mandibular retrognathia group, but were not significantly found. Finally, the distance between the hyoid bone and the pogonion has decreased in the mandibular retrognathia group due to the position of the chin.