Introduction
Intellectual Disability (ID) is a disorder included in the group of developmental disorders, whose definition is based on intellectual function significantly below the average manifested before the age of 18, through limitations in at least one adaptive skill, or which present certain chronic conditions arising from mental and/or physical impairment (1). The term ID is used, in this context, as a synonym for learning disability (United Kingdom), mental retardation (Brazil) and mental disability (United States) (2).
Different clinical conditions must be considered for the conceptualization of ID, such as functional limitations and communication skills. The main diagnostic measure used in Brazil is based on the criteria established by the International Classification of Diseases and Related Health Problems (ICD-10) (3). ID can be classified as mild, moderate, severe, and profound mental retardation, in addition to the unspecified (significant impairment of behavior, requiring surveillance or treatment) (3).
Associated with physical or environmental factors, ID is characterized as the most common disorder capable of inhibiting or hindering the active participation of the carrier in society (4). Estimates about the prevalence of this condition vary according to the inclusion criteria and the methodologies used (5). In Brazil, epidemiological studies with ID patients are scarce, but national estimates indicate that the incidence of this condition is 11.5 per 100 live births (6).
In children with ID, the slower rate of development affects learning, interaction, and communication with others people (2). The risk factors identified in children with ID include lower IQ, lower communication skills, higher incidence of medical illnesses, and difficulties in social interaction or behavioral problems (7). Consequently, these restrictions can lead to dysfunction in self-care and make these children dependent on others for their activities of daily living (8), which can influence the quality of life of this group (9). International literature has shown that ID patients can have a reduced quality of life (9,10,11) Some factors may influence this situation, and, in addition to risk factors, social, economic, and demographic characteristics may be associated with the quality of life of these individuals (12).
The involvement of ID does not only affect children themselves but also their families (13). Children affected by the condition need more care, and their parents experience more stress when caring for them (14). In most cultures around the world, women have more responsibility for raising children, and the main caregivers/caregivers of children with ID are usually mothers (15). When facing children's problems, mothers can experience situations of physical and mental stress, which also affects the quality of life of these caregivers (16).
Oral health is another fundamental aspect of quality of life, and this is particularly consistent for people with intellectual disabilities (17). ID patients, especially those with associated motor limitations (18), have worse oral hygiene conditions and a higher incidence of oral diseases (19). Couto et al. (2018) evaluated the quality of life of Portuguese ID and observed that in more than half of individuals, oral health had a significant impact on quality of life (20).
In this context, this study seeks to evaluate the factors associated with the quality of life-related to the oral health of children with intellectual disabilities from the perspective of their parental-caregivers.
Materials and methods
Study design
This is a cross-sectional study, in which data collection was carried out through dialogued interviews with the heads of children with ID and oral clinical examination in them. The survey was carried in six institutions to support people whit disabilities (PWD) in the state of Sergipe, Brazil.
The variables related to the social context of the guardians were age, marital status, education, income, and the number of children. Variables on children include age, gender, hygiene, and eating habits, as well as a history of breastfeeding. The independent variables studied were dichotomized according to the median or were grouped into categories according to homogeneity or frequency distribution to verify the association between the outcome. The number of Brazilian minimum wages (R$ 937.00 = $ 172,00 - in july 2020) received per family was considered a parameter for socioeconomic status.
Sample and recruiting
The study consisted of a convenience sample, formed by pairs of children with mental retardation and their mothers, duly registered and attended at the institutions supporting the PWD in the municipalities of Aracaju and Nossa Senhora do Socorro selected for this study.
The initial survey estimated that there were 134 children diagnosed with mental retardation, aged 6 to 12 years, of both sexes, enrolled in government institutions in the cities of Aracaju and Nossa Senhora do Socorro. The choice of support units for PWD in the respective municipalities occurred due to the social representativeness of these institutions since they serve a large part of the disabled population of the municipalities included in this study, as well as the lack of health information in this group in Brazilian computerized databases. The final sample number of this study was composed of 92 pairs of responsible children. Furthermore, the data obtained in the study by Racy (2016) was used as a basis, which provided this study with 90% statistical power to test a difference of 11.7 means with 95% two-tailed reliability parameters (21).
Those responsible for the children were contacted by phone, informed about the study and, upon acceptance, a meeting was held with those who spent the most time taking care of the children to present the research objectives.
Inclusion and exclusion criteria
To be eligible for the study, participants had to meet the following inclusion criteria: be registered in the institutions covered by the study, be included in the age group between 6 and 12 years old, present a medical diagnosis of mental retardation (ICD-10 code: 79) and not have any other type of disability (3). The medical diagnosis of mental retardation was obtained through the medical records provided by the institutions. Also, guardians should spend at least 12 hours a day with the child.
Participants were excluded due to the lack of information in the clinical record, the inability to attend the place where the study was being conducted, and the refusal to participate.
Data collection
Data collection was carried out in two stages: (i) dialogue interview for the application of questionnaires for socioeconomic, demographic, psychosocial assessment, eating and hygiene habits, and history of breastfeeding with parents- caregivers; (ii) oral clinical examination to assess oral hygiene and dental caries in children. Both steps were performed by the same evaluator.
Dailogue interview
Upon prior appointment, the interviews took place in person at the institutions, before the children's oral clinical examination. The questionnaires were applied by a pair of evaluators, previously trained in the reading and intonation of each question, and the answers to the printed instruments.
In the questionnaire, the questions addressed to the responsible persons evaluated the socio- demographic and economic conditions based on the criteria established by the National Health Survey of Brazil of the Brazilian Institute of Geography and Statistics (Instituto Brasileiro de Geografia e Estatística-IBGE).
Data on quality of life and impact on the family were collected using the Brazilian versions of the Parental-Caregiver Perceptions Questionnaire (P-CPQ) and the Family Impact Scale (FIS) (22, 23).
The P-CPQ is a reliable measure that assesses the parent caregiver's perception of the quality of life about children's oral health. In general, it consists of an automatic questionnaire, composed of 33 questions, using the 5-point Likert- type answer options, which assess the perceptions of parents-caregivers about the impacts of oral diseases on the quality of life of children and adolescents from 6 to 14 years. The 33 items of the P-CPQ are distributed in different subscales, which are: "oral symptoms" (OS), "functional limitation" (FL), "emotional well-being" (E-WB) and "social well-being" (S-WB) (22).
For the P-CPQ scale, the final score ranges from 0 to 124, with high scores indicating a greater negative perception of caregivers concerning the quality of life-related to their children's oral health (22). The FIS is an evaluation scale that analyzes the effects of children's oral disorders on the functioning of their family, referring to the frequency of events in the previous three months. The instrument consists of 14 items divided into four domains: parent/family activity, parent/family emotions, family conflict, and financial burden. The final score for the FIS scale ranges from 0 to 56, where the highest score means the greatest impact of the child's oral condition on the family's quality of life (23).
Oral clinical examination
The oral clinical examination was carried out by the evaluators of the Postgraduate Program in Dentistry at the Federal University of Sergipe, in an environment with natural lighting, with the use of an odontoscope, spherical tip probe (0.5mm), cotton and surgical gloves. According to the criteria established by the World Health Organization, the verification of the experience of dental caries and oral hygiene was measured through the Index of Decayed, Lost and Filled Teeth for primary dentition (dmft) and permanent dentition (DMFT), and Oral Hygiene Index (OHI-S), respectively.
For children with mixed dentition, the caries index was assessed by the sum of the components d + m / D + M + F. The dmft / DMFT was categorized according to the experience of dental caries: dmft / DMFT 0 = caries-free; 1 to 2 = low experience; from 3 to 4 = moderate experience and ≥ 5 = high experience.
The condition of oral hygiene, assessed by the OHI-S index, is based on the amount of debris (DI-S) and dental calculations (CI-S) that affect the six representative surfaces of the teeth in the mouth. The surfaces examined for OHI-S were selected from four posterior and two anterior teeth (first right upper molar, right upper central incisor, first left upper molar, lower left central incisor, first left lower molar, and first left lower molar). The vestibular surfaces were examined for all teeth, with the exception of the lower molars, where the lingual surfaces were examined.
The OHI-S value was organized from the sum of DI-S and CI-S. The oral hygiene index can vary between 0 to 3.0 and be classified as good oral hygiene (0 to 0.6), regular oral hygiene (0.7 to 1.8) or poor oral hygiene (1.9 to 3.0), according to the model suggested by Greene and Vermillion (24).
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences software (IBM® SPSS 25.0 for Windows, Inc., Chicago, IL, USA). The Shapiro-Wilk test was adopted to verify normality and demonstrated that the quantitative dependent variable, total P-CPQ score, presented a non-parametric distribution.
Descriptive data were expressed as absolute and relative frequency, median and interquartile range. Inferential statistics was tested using Mann-Whitney U test and the Kruskal-Wallis, followed by the Bonferroni correction. The level of significance was considered when p <0.05.
Ethical aspects
This study was carried out by the principles of the Declaration of Helsinki and with Resolution 196/1996 of the National Health Council of Brazil (Conselho Nacional de Saúde do Brasil), receiving a favorable opinion from the Research Ethics Committee of the Federal University of Sergipe, under the number of order approval protocol 1.639.022. After obtaining permission from each institution involved in the study, the participants who agreed to participate in the research signed the Free and Informed Consent Form.
Results
Among the 134 children and their parents- caregivers eligible for the study, 4 (3.7%) children were hospitalized, 16 (11.9%) did not present their medical records properly filled out and 21 (15.6%) parent-caregivers refused to participate in the study. study. Finally, the sample consisted of 92 pairs of children and their guardians, 100% of whom were mothers.
Most mothers were under 40 years old (58.6%), were married (60.8%) and had 5 to 9 years of study (68.4%). They had more than 3 children (38.1%) and received less than one Brazilian minimum wage per family on a monthly basis (82.6%) (Table 1).
Regarding children, most were between 10 and 12 years old (75.0%), were female (66.3%), performed daily self-care activities in oral hygiene (92.3%), had daily brushing frequency of once a day (75.0%), with a history of breastfeeding (64.1%), bottle use (85.8%) and daily fruit consumption (51.9%) (Table 1).
The mean of the global P-CPQ was higher among mothers with more than 9 years of study (p=0.022), in female children (p=0.012), who were breastfed (p=0.018) and who brushed their teeth through least once a day (p=0.011). The FIS was not associated with any of the child's sociodemographic and behavioral variables (Table 2).
The global mean P-CPQ score in the sample was 23.28±7.0. Among the subscales, functional limitation and oral symptoms had the highest averages 12.07±3.67 and 11.04±4.20, respectively. The average FIS score was 0.64±3.73 (descriptive data not shown in the table). Considering each subscale of the P-CPQ, only the impact on functional limitation was associated with mothers' education (p=0.004) and breastfeeding (p=0.038) (Figure 1).
As for oral health, 40.2% of children were found without caries disease, while 30.5% and 29.3% had low/moderate and high caries experience, respectively. There was no association between the severity of dental caries and the mean global P-CPQ and the subscales of the instrument (p>0.05) (Table 3).
The condition of oral hygiene was observed as good in 29.3% of the children, 6.5% as regular and 64.1% as poor, however, there was no association between the average perception of those responsible for health-related quality of life oral health of children and their subscales (p>0.05) (Table 3).
Table 1 Characteristics of caregivers and children included in the study (n=92). Brazil, 2020.
| Variables | n | % |
|---|---|---|
| Parental-caregiver | - | - |
| Age | - | - |
| < 40 years | 54 | 58.6 |
| ≥ 40 years | 38 | 41.4 |
| Marital status | - | - |
| Single | 21 | 22.8 |
| Married | 61 | 66.3 |
| Separated/divorced/widowed | 10 | 10.9 |
| Schooling level (years of study) | - | - |
| 0 - 4 | 8 | 8.7 |
| 5 - 9 | 63 | 68.5 |
| ≥ 9 | 21 | 22.8 |
| Number of children | - | - |
| One | 28 | 30.4 |
| Two | 29 | 31.5 |
| Three or more | 35 | 38.1 |
| Family income | - | - |
| ≤ One BMW# | 76 | 82.6 |
| > One BMW | 16 | 17.4 |
| Children | - | - |
| Age | - | - |
| Up to 9 years | 23 | 25.0 |
| Between 10 to 12 years | 69 | 75.0 |
| Gender | - | - |
| Female | 61 | 66.3 |
| Male | 31 | 33.7 |
| Independence in daily oral hygiene | - | - |
| Yes | 85 | 92.3 |
| No | 7 | 7.7 |
| Brushing frequency | - | - |
| 1 time a day | 69 | 75.0 |
| 2-3 times a day | 23 | 25.0 |
| History of breastfeeding | - | - |
| Yes | 59 | 64.1 |
| No | 33 | 35.9 |
| Bottle-feeding | - | - |
| Yes | 79 | 85.8 |
| No | 13 | 14.2 |
| Daily fruit consumption | - | - |
| Yes | 47 | 51.9 |
| No | 45 | 48.1 |
Results are expressed in absolute (n) and relative (%) frequency; #BMW: Brazilian minimum wage.
Table 2 Median and interquartile range (IQR) between sociodemographic and economic characteristics, eating habits, oral hygiene practices and breastfeeding history for P-CPQ and FIS. (n = 92). Brazil, 2020
| Variables | n | % | Overall P-CPQ | P-value | FIS | P-value |
|---|---|---|---|---|---|---|
| Parental-caregiver | - | - | - | - | - | - |
| Age | - | - | - | - | - | - |
| < 40 years | 54 | 58.6 | 26.00 (22.00; 26.00) | 0.642£ | 0.00 (0.00; 0.00) | 0.808£ |
| ≥ 40 years | 38 | 41.4 | 26.00 (22.00; 26.00) | - | 0.00 (0.00; 0.00) | - |
| Marital status | - | - | - | - | - | - |
| Single | 21 | 22.8 | 26.00 (22.00; 27.00) | 0.00 (0.00; 0.00) | ||
| Married | 61 | 66.3 | 26.00 (23.50; 27.80) | 0.447§ | 0.00 (0.00; 0.00) | 0.870§ |
| Separated/divorced/widowed | 10 | 10.9 | 26.00 (23.50; 26.00) | - | 0.00 (0.00; 0.00) | - |
| Schooling level (years of study) | - | - | - | - | - | - |
| 0 - 4 | 8 | 8.7 | 24.00 (22.00; 26.03)a | - | 0.00 (0.00; 0.00) | - |
| 5 - 9 | 63 | 68.5 | 26.00 (22.00; 26.00)b | 0.042§ | 0.00 (0.00; 0.00) | 0.985§ |
| ≥ 9 | 21 | 22.8 | 28.00 (24.00; 30.00)b | - | 0.00 (0.00; 0.00) | - |
| Number of children | - | - | - | - | - | - |
| One | 28 | 30.4 | 24.00 (22.00; 26.00) | - | 0.00 (0.00; 0.00) | - |
| Two | 29 | 31.5 | 26.00 (23.00; 28.00) | 0.114§ | 0.00 (0.00; 0.00) | 0.957§ |
| Three or more | 35 | 38.1 | 26.00 (22.00; 26.00) | - | 0.00 (0.00; 0.00) | - |
| Family income | - | - | - | - | - | - |
| ≤ One BMW# | 76 | 82.6 | 26.00 (22.00; 26.00) | 0.647£ | 0.00 (0.00; 0.00) | 0.932£ |
| > One BMW | 16 | 17.4 | 25.00 (22.00; 26.00) | - | 0.00 (0.00; 0.00) | - |
| Children | - | - | - | - | - | - |
| Age | - | - | - | - | - | - |
| Up to 9 years | 23 | 25.0 | 24.00 (18.00; 27.00) | 0.528£ | 1.70 (±6.30) | 0.118£ |
| Between 9 to 12 years | 69 | 75.0 | 26.00 (22.00; 26.00) | - | 0.29 (±2.28) | - |
| Gender | - | - | - | - | - | - |
| Female | 61 | 66.3 | 26.00 (24.00; 26.00) | 0.012£ | 0.79 (±4.40) | 0.508£ |
| Male | 31 | 33.7 | 22.00 (18.00; 26.00) | - | 0.35 (±1.79) | - |
| Independence in daily oral hygiene | - | - | - | - | - | - |
| Yes | 85 | 92.3 | 26.00 (22.00; 26.00) | 0.279£ | 0.88 (±4.22) | 0.797£ |
| No | 7 | 7.7 | 26.00 (24.00; 28.00) | - | 0.00 (±0.00) | - |
| Brushing frequency | - | - | - | - | - | - |
| 1 time a day | 69 | 75.0 | 24.00 (22.00; 26.00) | 0.022£ | 0.86 (4.29) | 0.344£ |
| 2-3 times a day | 23 | 25.0 | 21.05 (10.00; 24.00) | - | 0.00 (±0.00) | - |
| History of breastfeeding | - | - | - | - | - | - |
| Yes | 59 | 64.1 | 26.00 (24.00; 26.00) | 0.018£ | 1.09 (±4.25) | 0.657£ |
| No | 33 | 35.9 | 24.00 (21.00; 26.00) | - | 0.66 (±3.97) | - |
| Yes | 79 | 85.8 | 26.00 (22.00; 26.00) | 0.728£ | 0.58 (±2.97) | 0.862£ |
| Bottle-feeding | - | - | - | - | - | - |
| No | 13 | 14.2 | 24.00 (21.00; 26.00) | - | 2.23 (±8.04) | - |
| Daily fruit consumption | - | - | - | - | - | - |
| Yes | 47 | 51.9 | 26.00 (22.00; 26.00) | 0.774£ | 1.23 (±5.17) | 0.120£ |
| No | 45 | 48.1 | 26.00 (22.00; 26.00) | - | 0.02 (±0.14) | - |
# BMW: Brazilian minimum wage; £ Mann-Whitney Test; § Kruskal-Wallis; Different letters mean statistically different results (p< 0.005): significance values were adjusted using the Bonferroni correction.
Table 3 Distribution of the median and interquartile range of the P-CPQ and FIS scores in relation to dental caries and oral hygiene (n=92). Brazil, 2020.
| Clinical condition | n | % | Overall P-CPQ (±SD) | OS* | FL* | E-WB* | S-WB* | FIS |
|---|---|---|---|---|---|---|---|---|
| Severity of dental caries (dmft/DMFT) | - | - | - | - | - | - | - | - |
| Caries free | 37 | 40.20 | 26.00 (22.00; 26.00) | 12.00 (11.00; 12.00) | 14.00 (10.00; 14.00) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) |
| Low experience | 17 | 18.60 | 26.00 (22.00; 26.00) | 12.00 (12.00; 12.00) | 12.00 (10.00; 14.00) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) |
| Moderate experience | 11 | 11.90 | 26.00 (22.00; 26.00) | 12.00 (12.00; 12.00) | 14.00 (10.00; 14.00) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) |
| High experience | 27 | 29.30 | 26.00 (22.00; 26.00) | 12.00 (12.00; 14.00) | 12.00 (12.00; 14.00) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) |
| P-value§ | - | - | 0.903 | 0.143 | 0.984 | 1.000 | 1.000 | 1.000 |
| Oral hygiene (OHIS-S) | - | - | - | - | - | - | - | - |
| Good | 27 | 29.30 | 26.00 (22.00; 26.00) | 12.00 (10.00; 12.00) | 12.00 (10.00; 14.00) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) |
| Fair | 6 | 6.60 | 24.00 (24.00; 26.75) | 12.00 (11.50; 12.00) | 13.00 (12.00; 14.00) | 0.00 (0.00; 0.75) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) |
| Poor | 59 | 64.10 | 26.00 (22.00; 26.00) | 12.00 (12.00; 12.00) | 12.00 (10.00; 14.00) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) | 0.00 (0.00; 0.00) |
| P-value§ | - | - | 0.665 | 0.323 | 0.782 | 1.000 | 1.000 | 1.000 |
*OS: Oral symptoms; FL: Functional limitations; E-WB: Emotional well-being; S-WB: Social well-being; § Kruskal-Wallis.
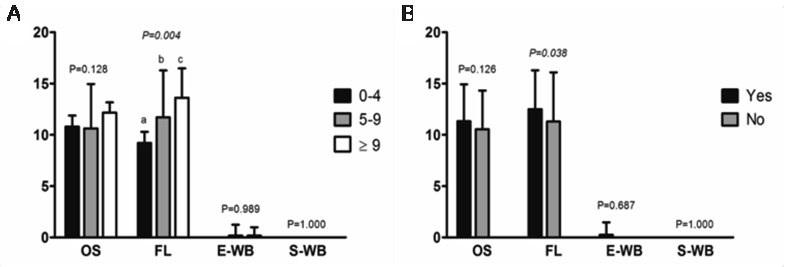
Figure 1 Subscales median scores for P-CPQ in relation to (a) schooling level and (b) history of breastfeeding. Different letters mean statistically different results (p<0.005): significance values were adjusted using the Bonferroni correction. OS=Oral symptoms; FL=Functional limitations; E-WB=Emotional well-being; S-WB=Social well-being. Brazil, 2020.
Discussion
The results found to reflect poor oral health conditions in children with ID, with a high presence of dental biofilm and caries experience. Mothers' perception of the impact of the oral condition on the child's and family's quality of life was low, however, the average perception of oral condition on the child's quality of life was observed among those with a higher level of education, responsible for sex children female, with a history of breastfeeding and who brushed their teeth less frequently. Regarding the dimensions assessed by the P-CPQ subscales, the impact of functional limitations was also associated with the mothers' education level and history of breastfeeding.
In this study, it was observed that most children had regular or poor oral hygiene, which corroborates the results found in a meta-analysis that confirmed that children with ID had significantly higher levels of dental biofilm than those without ID (25). National and international studies have also reported that ID patients tend to have poor oral hygiene, in addition to a high rate of experience of caries and periodontal disease, as well as a greater number of extractions and fewer restorative procedures when compared to the general population (26, 27).
The process of developing dental diseases in individuals with ID does not differ from those who do not have any disabilities. Similarly, both prevention and treatment modalities among these individuals do not differ, and the main factor related to oral problems in people with disabilities is the inadequate removal of dental biofilm (22).
The high experience of dental caries in this study was observed in 29.3% of children, higher estimate than those found in the local literature (28) and lower than the global values (29) literature. The Brazilian study by Batista et al. (2009), reported a strongly compromised dentition and unsatisfactory oral health in 24% of the children evaluated and with mental retardation, using the WHO criteria (28). Also, other studies that evaluated the oral health condition in Brazilian children from other groups of intellectually disabled people, such as those with Autism Spectrum Disorder and Down Syndrome, demonstrated a high caries experience present in 37.05% and 44.20% of the sample, respectively (30,31).
In addition to specific factors, such as functional and communication limitations, studies correlate the high experience of dental caries in intellectually disabled people with the social, demographic, and economic context of those responsible (32). These families are generally socially and emotionally disadvantaged, with this they have little knowledge of health, increasing the chances of triggering oral diseases among these patients (33). Also, it should be noted that the lack of parental guidance regarding the need for comprehensive care, the difficulty in understanding the effects of behavior on health and the benefits of dental treatment, may be factors that reflect the high caries experience in this group, as well as the process of access to adequate health services (34).
Parents-caregivers are the most influential models for their children, and the habits adopted during childhood, when the child is dependent on the guardian, are the powerful means to establish a new behavior in the child's routine, such as brushing. As a result, guardians need to have an adequate attitude and knowledge about oral health, to instigate good oral habits in their children (35). In this context, it is reinforced again that the social determinants of the guardians can influence the way they observe the oral condition of their children (36).
Several factors have been described as predictors of parents' perception of the oral health of children without disabilities, such as the child's age and sex, family income, ethnicity, and different oral health problems (37,38). However, the literature is not clear in relation to the factors associated with the perception of those responsible for the impact of oral health on the quality of life of children with ID. The study by Pani et al. (2013) assessed the perception of parents-caregivers of autistic children and found that the age and educational level of the parents was associated with a greater negative perception of the impact of oral health on children's quality of life (36). With similar characteristics, Aggarwal et al. (2016) observed the impact of oral health conditions on the quality of children with ID and their families and can conclude that the child's oral health perception can be influenced by the family's socioeconomic status (32).
Among the sociodemographic variables assessed in this study, only the level of education was associated with a greater perception of the impact of oral conditions on children's quality of life, pointing out that those with less education perceive the impact of oral conditions on their children's lives less, as well as low education, reduces the search for dental care and self-care in oral health (39). According to more years of schooling among those responsible, the greater the chances of access to health information, as well as the promotion of better self-care, which can have a positive effect on the perception of the impact of oral conditions on the child's quality of life (39). In this circumstance, the low level of education observed in the caregivers of children and adolescents with ID is due to the need for these individuals to abandon their studies to dedicate themselves to the integral role of caregiver, which leads to low levels of information and self-care with the child health (40).
The lower frequency of brushing among children can trigger several oral disorders and, consequently, more complaints of pain or discomfort, and only then do the caregivers become more aware of the impact of oral conditions on their quality of life. Linked to this, those with lower education levels may not be properly oriented to intervene and promote adequate oral hygiene for children, considering the fact of little or no knowledge in health, but it should be emphasized that health education can act as a tool transformed in changing habits and appropriate attitudes in the caregivers' routine (41,42).
The average perception of those responsible for the impact of oral health on the quality of life of female children was higher when compared to male children. This result corroborates with those found in other studies and demonstrates that women complain more about oral problems that affect them (43). Also, this may be because girls have a higher prevalence of hormonal changes that can influence their oral health, in addition to greater demands on the aesthetic appearance of the smile, which make them more sensitive to the presence of caries and consequently, it causes greater complaints about his oral condition (43,44).
A meta-analysis, involving approximately 400 studies, showed that breastfeeding has several positive effects for the child, improves the affective bond between mother and child, and reduces the risk of respiratory infections and obesity (45). Also, functional stimuli arising from breastfeeding, such as sucking, chewing, swallowing, and breathing are related to craniofacial growth, as well as being associated with the correct development of dentofacial structures (46).
In our sample, breastfeeding was associated with a greater perception of caregivers about the influence of functional limitations on the child's quality of life. This may be related to the fact that breastfeeding mothers observe more the child's oral cavity during breastfeeding (47), being able to identify the presence of several oral problems, such as mouth sores, parafunctional habits, gingival bleeding, difficulty in biting, chewing, swallowing or eating food (48). Although this study did not evaluate breastfeeding duration, an association was recently found between longer breastfeeding duration and a greater perception of children's oral health (47,49).
The results suggest that the impact of oral health-related quality of life was greater at the individual than at the family level. It is also observed that those responsible did not report the impact of oral health on the social well-being of children, and this can be attributed to numerous factors, among them the fact that the low level of education of parents affects the perception of children's oral conditions and the lack of knowledge about what a proper oral condition looks like. Also, the "I don't know" responses reported were included, but considered absent, which may contribute to the result found and be justified by their low level of education.
One of the limitations of this study is that its transversal character makes causal inferences impossible. In addition to this, the absence of a control group and the use of a sample for convenience increases the possibility of bias. The assessed sample was deliberately limited to those referred to specialized health services, providing a group of individuals with a higher prevalence of potential risk factors for oral health problems when compared to other groups in the general population. Also, the present study did not assess the severity of the patients' general clinical condition, since such information was not available in the medical records of children with ID, however some previous studies did, and a greater impact was observed among patients with greater disease severity (32).
Conclusion
The results found in this study emphasize the need for understanding and training of caregivers about their active role in the proper maintenance of children's oral condition. Considering the high experience of caries and poor oral hygiene among children with ID, as well as the influence of different factors on the perception of those responsible for the impact of oral conditions on their children's lives, it is necessary to promote the importance of health oral health for general health. Also, the importance of looking for dental care services, adequate and supervised brushing and healthy eating habits to limit the progression of dental caries and other oral disorders in the population with intellectual disabilities should be reinforced.














