Intoduction
Hallermann-Streiff syndrome ((HSS), OMIM (Online Mendelian Inheritance in Man) 234100), is a rare but highly recognizable congenital syndrome which described firstly by Aubry in 1893 and later by Hallermann (1948) and Streiff (1950) (1). Although the genetic basis and underlying molecular mechanism are not yet known (2), second asymmetric bronchial arch defect at the fifth or sixth gestational week, maternal infections, father age, and toxin exposure may be the predisposing factors in HSS (3). Both sexes are equally affected (4). The general diagnosis of HSS is based on the presence of clinical findings: birdlike craniofacial features, prominent, thin, pointed nose, blue sclera, bilateral congenital cataracts, nystagmus, proportionate nanism, bilateral microphthalmia, relatively small stature, hypotrichosis, frontal and parietal bossing, cutaneous atrophy, cranial suture dehiscence with open fontanelles, high- arched palate, dental anomalies, microstomia, and mandibular hypoplasia with anterior displacement of the mandibular condyle (5). Dental anomalies have been detected in 50-80% of the patients. These are absence of teeth, natal teeth, enamel hypoplasia, severe caries, dental malformation, supernumerary teeth, malocclusion and premature eruption in primary dentition (6).
In this case report, a 6-year-old male patient diagnosed with HSS has described the clinical findings and dental anomalies. Conservative treatment protocols and a 12-month follow-up are presented.
Case report
A 6-year-old male patient previously diagnosed with HSS was referred to the Department of Pediatric Dentistry at the Faculty of Dentistry, Gaziantep University (Turkey). The patient and his parents were informed about the case report and consent forms were obtained. This patient was the third child of consanguineous healthy parents (mother; 26, father; 30). There was no sign of the syndrome on the other two brothers. The patient was born at 38 weeks of gestation with vaginal birth and weighed 3400 g and length of 51 cm, and had no mental retardation. Sleep apnea and wheezing during the first 6 months were also recorded.
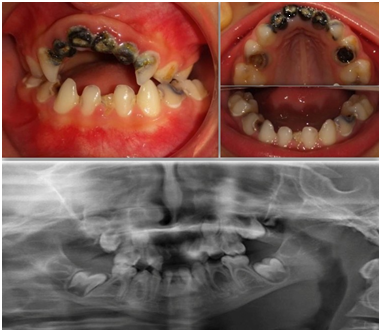
Microcephaly, brachycephaly, frontal bossing, microstomia, hypoplastic alae nasi, beaked nose, micrognathia and double chin, congenital cataract, microphthalmia, nystagmus, strabismus, skin atrophy, prominent scalp veins, localized hypertrichosis, sparse hair, eyebrows, and eyelashes were recorded by extraoral examination (Figure 1). Mandibular hypoplasia, malocclusion especially open-bite, deep palate, malformed teeth, deep caries and the congenital absence of eighteen teeth (11,12,21,22,14,15,24,25,41,42,43,44,45,31,32,33,34, and 35) were detected by intraoral and radiographic examination (Figure 2).
A treatment planning including preventive applications, restorative, surgical and preventive orthodontics procedures was determined for the patient. He was subjected to an intensive preventive program consisting of weekly oral hygiene instructions and dietary recommendations so that he would be able to use his existing teeth for a longer time and his growth and development would be ensured in a healthy way. It was decided to extract the teeth with root resorption or deep caries lesion that could not be treated (51,52,61,62, and 74). The teeth of 54 and 84 were amputated with MTA (Angelus, Londrina, PR, Brazil), and covered with Ormocer-based composite (Admira Xtra Fusion, VOCO, Cuxhaven, Germany). The composite resin restorations were also applied on 53,63, 64,65,72, 73, 75, 82, 83, and 85. Nance and band loop space maintainer was applied to the spaces resulting from the absence of teeth. Nance Appliance with bands on teeth 55 and 65 was fixed, and the acrylic was extended to the front of the alveolar crest and artificial teeth were placed in the 51 and 61 teeth region to provide aesthetic rehabilitation. After the treatment protocols, oral and hygienic conditions were evaluated for 12 months; in the first 3 months, monthly and then every 6 months (Figure 3).
Discussion
HSS is a rare oculomandibulofacial discephaly with hypotrichosis that occurs as a sporadic mutation (7). The differential diagnosis of HSS should be made with progeria, mandibular dysostosis, Wiedemann-Rautenstrauch syndrome and seckel syndrome (8). Progeria is an autosomal dominant inherited childhood disease that is characterized by premature aging and may result in death due to atherosclerosis complications such as myocardial infarction, stroke, atherosclerosis or heart failure (9). In patients with mandibulofacial dysostosis and Hallermann-Streiff syndrome, the findings of micrognathia, high palatal dome and molar hypoplasia are similar, but mandibulofacial dysostosis is usually associated with lower eyelid and ear anomalies. Although Wiedemann Rautenstrauch syndrome patients have a similar facial appearance, they do not show ocular symptoms. In Seckel syndrome, the absence of cataracts in the eyes, deformities in the ears, normal temporomandibular joints, and severe microcephaly enable the syndrome to be distinguished from HSS (1,10). Francois has mentioned positive (Dissefaly and bird face, dental anomalies, proportional short stature, hypotrichosis, microphthalmia, skin atrophy) and negative signs (Ear anomalies, palpebral anomalies, nail and lip anomalies, premature atherosclerosis, arthrosis, mental retardation) in order to identify and diagnose the disease (11). In this patient, all positive signs described by Francois have been observed and the patient has no negative signs. Therefore, the patient's findings are typical for this syndrome.
Cohen described the incidence of each criterion which was identified by Francois. The incidence of dental anomalies, one of these criteria, was 85% (12). These were mandibular hypoplasia, hypodontia, malocclusion, dental malformation, natal teeth and premature eruption in primary dentition (13). Odontodysplasia (6, 14), permanent teeth with the absence of roots, impacted teeth (10), hypoplastic coronoid, and condylar processes (4) were also reported in patients with HSS. In this case, enamel-dentin structures and pulp chamber of the teeth were noted normally. However, mandibular hypoplasia, malocclusion (especially anterior open-bite) and deep palate were observed.
In this case, the most remarkable dental anomaly was oligodontia characterized by many missing teeth (n≥6). The patient's permanent teeth (except for 16,17,26,27,36,37, 46, 47,13, 23) have been detected missing congenitally by panoramic radiograph. However, it has been suggested that the age of 10 years was critical for confirming the absence of a second premolar (15). Therefore, the follow-up of the patient is so important to evaluate the prognosis of tooth agenesis. In a case, a 20- year follow-up of the patient with HSS with 16 missing teeth, orthodontic, restorative and prosthetic applications were presented (13). In this case, endodontic and restorative procedures were applied to keep the existing deciduous teeth in the mouth as much as possible. However, the root resorption of deciduous teeth is unpreventable. Therefore, especially in patients with HSS associated with missing teeth, implant and removable prosthesis was recommended along with the completion of growth (8,16).
Conclusion
This case report presents the orofacial findings of a 6-year-old patient with HSS and conservative treatment approaches. The identification of facial and dental anomalies of this rare syndrome is very important to determine the prognosis of the disease and to take protective and preventive measures. Therefore, each case presented with the syndrome may contribute to the literature. In this case, due to a large number of dental anomalies, patient follow-up is continuing for providing aesthetic and functional rehabilitation and its sustainability.