Introduction
The treatment of teeth with incomplete rhizogenesis and pulp necrosis is a considerable clinical challenge involving endodontic treatment, to induce an apical barrier using bioactive materials (apexification) (1), and restorative treatment, the success of which depends on adequate adherence.
Mineral trioxide aggregate (MTA) has been widely used as a promising biomaterial to induce an apical barrier because it allows an adequate marginal seal (2), is biocompatible (3), and hardens in the presence of moisture (4).
The clinical success of MTA has been attributed to its bioactive nature. The addition of mineral trioxide to synthetic tissue fluid causes the release of its main cationic components and triggers the precipitation of apatite crystals on its surface, which seems to allow chemical adhesion to the dentin when in direct contact (5). This mechanism explains the sealing capacity that, coupled with the slight expansion of the material after setting, improves adaptation to the dentinal walls (6,7).
Due to the hydrophilic characteristics of the aggregate, the moisture present in tissue acts as a catalyst or activator of the chemical reaction through the release of calcium and hydroxyl ions (7,8,9,10), which are incorporated into the precipitates when in a suitable environment. Therefore, its application in moist (tissue fluids, blood, etc.) presents no problems, which is an indispensable characteristic for its use in various clinical procedures (apexification, perforation sealing, retro-obturation, etc.) (11,12).
The interaction of MTA with a phosphate buffered saline (PBS) solution promotes the formation of carbonated apatite by an amorphous calcium phosphate phase (13,14). Reyes-Carmona et al (14) verified the presence of precipitates with different morphologies composed mainly of calcium and phosphorous ions, which contribute to the formation of an intermediate layer between the material and the dentin, promoting an intratubular biomineralization process. Noncollagen proteins of dentin, such as dentin matrix acidic phosphoprotein 1 (DMP-1), present a molecular specificity for the elements of apatite, acting as a guide during the incorporation of these elements into the collagen matrix, thus controlling the process of biomineralization (13,14,15). This continuous process of ion exchange between the cement, PBS, apatite, and dentin is responsible for the chemical adhesion described by Sarkar et al (5).
The apatite formed by the MTA-PBS system is deposited on collagen fibers and promotes intratubular biomineralization through extensions that reach into the interior of the dentin tubules (tag-like structures) at the interface (1,14,16). This process significantly improves resistance to displacement, adhesive strength, and marginal sealing of the MTA with dentin (1,14,17).
Although endodontic therapy with MTA in necrotic teeth with incomplete rhizogenesis has been proven to be clinically successful (18), these teeth have a high incidence of fracture due to insufficient thickness and fragile dentinal walls, and difficulties related to performing an adequate restorative procedure have been reported (18,19).
Intraradicular dentine is a complex and heterogeneous structure with a topography that varies depending on the region, the age of the tooth, the amount and orientation of dentin tubules, moisture, the intra and peritubular dentin areas, and the permeability (20, 21). These characteristics highlight the technical difficulties inherent to adhesive procedures performed inside the root canal (22).
Adhesion reflects the possibility of appropriately sealing the interface between a cavity and a restorative material (22,23). One of the most important elements for the bond strength of adhesive systems to dentin are resin tag formation, resin infiltration inside the demineralized matrix, and chemical adhesion to the surface (24). Therefore, penetration of the adhesive system in dentin tubules and in the network of collagen fibers is the only reliable means to achieve a strong micromechanical bond between the resin- based materials and dentin (25).
The use of fiberglass posts associated with adhesive cementation for the restoration of endodontically treated teeth can reduce the incidence of fractures by creating a mechanically homogeneous unit (post/cement/dentin) in which tensions are evenly distributed and function as a single entity (22,26).
On the other hand, the REBILDA® Post System, which is commercially available from VOCO (Cuxhaven, Germany), is a practical system for the cementation of intraradicular posts. The system uses the self-etch dual-cured adhesive system Futurabond DC, the REBILDA® Post fiberglass- reinforced composite post, and REBILDA® DC resin cement, a dual-curing (DC) flowable adhesive composite system. According to Reill et al (27), the use of the REBILDA® System increased the fracture resistance of the post and core in an ex vivo model of endodontically treated teeth.
Thus, our study aims to evaluate the biomineralization process promoted by ProRoot MTA and an experimental MTA combined with PBS as an intracanal medication using an ex vivo model and to analyze the adhesion process when using the REBILDA® Post System.
Materials and methods
Analysis of the biomineralization process of the experimental mta
A total of 12 single-rooted teeth were used, which were extracted for reasons unrelated to this study and were donated through a protocol of free informed consent.
Sections of 2-mm thickness were obtained from each tooth and the diameter of the root canal was standardized (Figure 1). The samples were placed in a solution of EDTA-17% (3min), followed by NaOCl-1% (3min), and then washed with distilled water and dried.
The root sections were randomly divided into 2 groups (n=12) and filled with different cements as described below.
Group 1: ProRoot (MTA) (Dentsply Tulsa Dental, Oklahoma, USA) diluted with distilled water in a concentration of 1 g/0.26 mL.
Group 2: MTA Exp = a cement based on MTA+20% bismuth oxide (Seelze, Hannover, Germany) + 10% calcium chloride (Labsynth, Diadema, SP, Brazil), which was diluted with distilled water in a concentration of 1 g/0.18 mL.
A dentin disc without any material was used as a control. The powder/liquid ratio was established according to Reyes-Carmona et al (14).
Immediately after filling, the samples were placed in 15 mL of PBS (pH =7.2) and incubated at 37 °C for 35 days. The PBS was replaced every 5 days, and this solution was collected (5,15,25, and 35 days), and the pH was determined using a digital pH meter (INSTRUTHERM, PH-1700, Sao Paulo, Brazil).
The obtained values were analyzed descriptively.
Every 5 days, the formation of precipitates was documented, and the surfaces of 10 samples were gently scraped with the blade of a spatula. The collected precipitates were dried in an incubator at 37 °C and weighed on a digital analytical balance (Mettler PE, 160, United States). The data obtained were statistically analyzed using t-tests in the GraphPad Prism program. The critical value of statistical significance was 5%.
The remaining 2 samples from each group were dried at 37 °C for 48 h and embedded in metal cylinders (stubs). The assembly was coated with a layer of 300 Å gold-palladium. The specimens were examined by scanning electron microscopy (SEM) (HITACHI, S-570, Japan) operating at 15 Kv.
The chemical composition of the precipitates was determined by EDAX's energy dispersive spectroscopy under a scanning electron microscope (HITACHI, S-570). To analyze ultrastructural features, the precipitates were photographed under various magnifications (125-5000X). The data were recorded and analyzed descriptively.
Evaluation of the biomineralization and adhesion processes in teeth with simulated incomplete rhizogenesis
Twenty-four extracted single-rooted teeth were used, and the crown and apex were sectioned and standardized to 16-mm lengths. The canal diameter was standardized with Gates-Glidden #2-4 drills under constant irrigation with NaOCl-3%. To standardize the diameter of the foraminal opening, retrograde preparation was performed with Gates-Glidden #5 drills (1.30-mm diameter). The final irrigation was completed with EDTA-17% (3 min), saline for neutralization, and finally NaOCl-3% (2 min). Subsequently, the root portions were washed in distilled water and dried in an incubator at 37°C for 24 h.
Apical plugs of 5-6 mm in length were created with ProRoot MTA. Each sample was placed in a wet foam block with PBS to simulate periapical tissues, and PBS was used as an intracanal medication (Figure 4B) for different durations (Group 1: 48 h; Group 2: 7 days; and Group 3: 15 days).
At the indicated time points, the restorative protocol was performed with the REBILDA® Post System (VOCO) in each of the roots according to the manufacturer's instructions. The samples were stored in the incubator at 37 °C for 2 weeks. Subsequently, a section was created along the longitudinal axis of the samples (Figure 2), and each fragment was processed for SEM analysis according to the protocol (14).
A series of microphotographs of the cement- post-dentin and MTA-dentin interface were taken. These microphotographs were aligned to facilitate visualization.
The ability to promote the MIT process with the different experimental protocols was evaluated at 500X-1000X magnification and classified by different scores between 0 and 3 (1). The observations were performed by 2 previously calibrated (Kappa test) operators. Scores were assigned according to the presence of MIT: Score 0.0, no MIT; Score 1.0, low MIT; Score 2.0, uniform MIT throughout the entire MTA-dentin interface; and Score 3.0, uniform MIT and mineralization in lateral branches. The assigned scores were analyzed with the Kruskal-Wallis and Dunn Multiple Comparison tests in the GraphPad Prism program. The level of significance was p=0.05.
Resin penetration (PR) by the REBILDA® Post adhesive system in the middle and cervical thirds was also evaluated by scores (28) as follows: Score 0.0, no PR; Score 1.0, low PR; Score 2.0, uniform PR throughout the entire interface of the dentin-adhesive system; and Score 3.0, uniform PR infiltrating the lateral branches. The assigned scores were analyzed with the Mann-Whitney test in GraphPad Prism statistical software. The level of significance was p=0.05.
Results
Analysis of the biomineralization process
The ProRoot MTA accumulated a greater amount of precipitates; however, no significant difference was found compared to the amount of precipitates formed by MTA Exp (p=0.0536) (Table 1).
Regardless of the group, the highest pH value was recorded on the fifth day (9.8-11.0). On the fifteenth day, a decrease was observed in all samples (8.8-8.7). In subsequent periods (25 and 35 days), pH levels remained relatively stable (7.4-7.7). The samples in the ProRoot MTA group showed the highest pH at all intervals. However, the MTA Exp group showed very similar behavior throughout the observation period. The pH of the solution in contact with the dentin disc remained at 7.2 throughout the experimental period.
The ultrastructural evaluation by SEM revealed the presence of precipitates with different morphologies (Figure 3). In general, both cements promoted the formation of precipitates, and no differences in ultrastructural or chemical composition were identified between the two materials. The average result obtained from the assessments of each sample at the different periods of time indicated the presence of calcium and phosphorus at a Ca/P molar concentration of 1.60-1.69 (Figure 4). Smaller quantities of precipitates with acicular extensions could be observed, which are typical of amorphous calcium phosphate. More compact and spherical precipitates were also detected.
Evaluation of the biomineralization and adhesion processes in teeth with simulated incomplete rhizogenesis
INTRATUBULAR MINERALIZATION AT THE MTA-DENTIN INTERFACE
Under SEM, cement, MIT, and dentin could be distinguished (Figure 5). Tables 2 and 3 summarize the data obtained from the microscopic evaluation.
The use of PBS for 48 h as an intracanal medication did not promote MIT in any sample (Table 2, Figure 5). When analyzing the samples from Group 2 (7 days), short and nonuniform MIT was noted; some type of biomineralization was observed in all but one sample. On the other hand, in all the samples from Group 3 (15 days), uniform MIT (Score 2) was observed, and only two samples showed slight mineralization of lateral branches (Score 3). Dunn's Multiple Comparison statistical test indicated a significant difference between the groups (Table 3).
EVALUATION OF THE INTERDIFFUSION ZONE OF THE RESIN-DENTIN SYSTEM
Based on these observations, in both the cervical and the middle third of the samples, the REBILDA® adhesive system effectively promoted the formation of the resin-dentin interdiffusion zone (RDIZ), including the formation of lateral branches in most of the samples (Figure 6). The formation of resinous tags was more evident in the cervical third; however, statistical analysis showed no significant difference between both thirds (p = 0.6477) (Tables 4 and Table 5).

Figure 1 Analysis of the biomineralization process of MTA. A. Assembly of the samples to select dentin discs of the middle third of the root. B. The samples were standardized with 2mm width and 2mm diameter cavities which were sealed with MTA. C. Samples immersed in PBS, for 35 days. The precipitates formed were collected and weighed to analyze their ultrastructural structure and chemical composition, 2 samples from each group were mounted in stubs and evaluated in SEM.
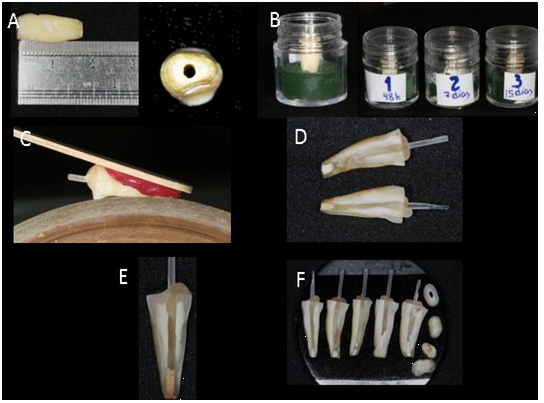
Figure 2 Evaluation of the biomineralization and adhesion processes in teeth with simulated incomplete rhizogenesis. A . Standardized specimens with a length of 16mm and a foraminal opening of 1.30mm in diameter. B. Storage in the sponge-PBS system. C. Longitudinal cutting of the samples. D. & E. Samples were analyzed at the MTA-POST-RESIN CEMENT-DENTINE interface. F. Samples placed in stubs for observation in SEM.
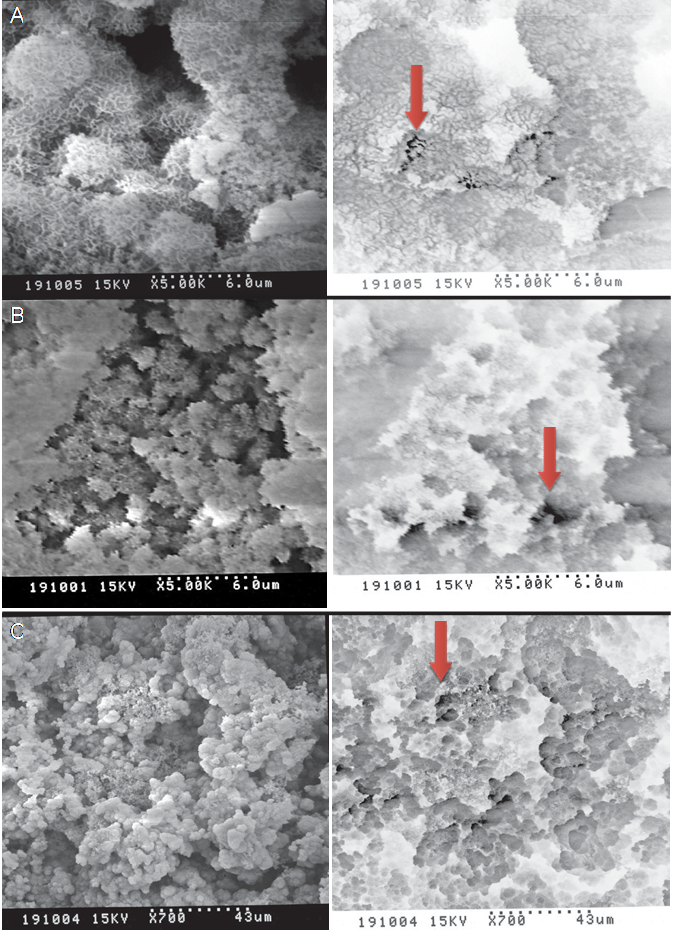
Figure 3 A-B. Spherical precipitates with acicular extensions. BI images denote areas with greater calcification (arrows). C. Areas with more compact lath-like precipitates and areas in BI which denotes greater mineralization (arrow).
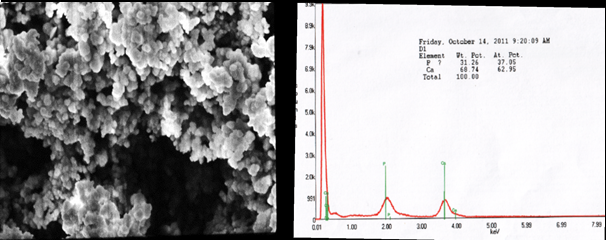
Figure 4 SEM photomicrograph of the precipitates analyzed by EDAX, EDAX spectrum showing the presence of calcium and phosphorus in a Ca / P ratio of 1.69.
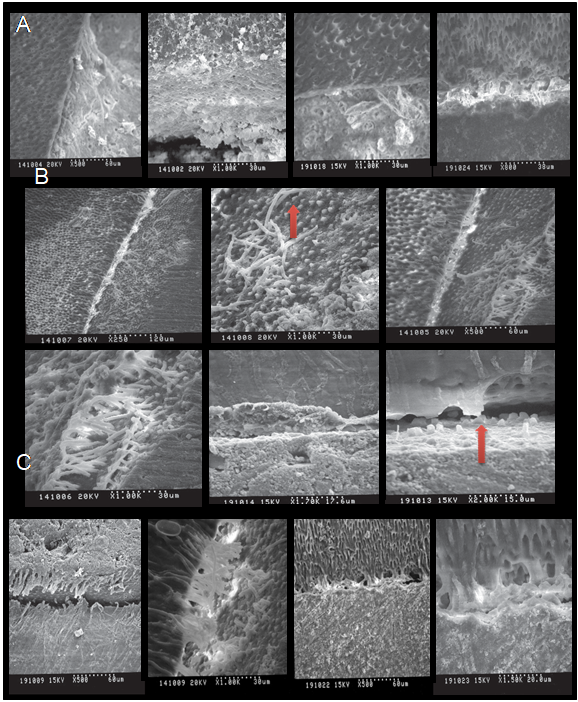
Figure 5 Intratubular mineralization (MIT). A. SEM Photomicrographs of the MTA-dentine Interface analysis of G1 (48h). There was no MIT.B. Representative SEM Photomicrographs of the analysis of group 2 (7 days). The formation of short MIT is observed throughout the samples. C. SEM Photomicrographs of the G3 (15 days). The uniform formation of MIT is observed.
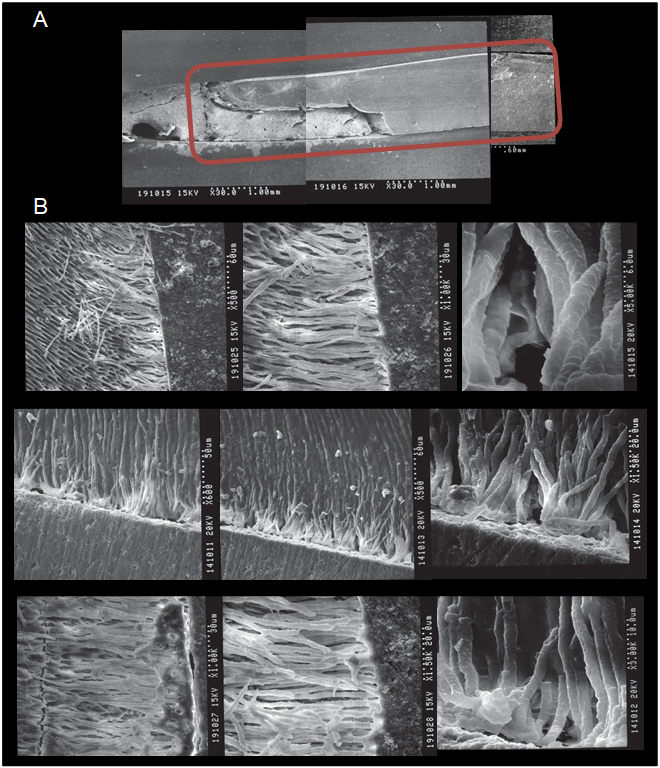
Figure 6 Dentin-Resin Interdiffusion (RDIZ). A. The samples were analyzed at the MTA-resin-dentin-cement cement interface. B. Representative SEM Photomicrographs of the analysis of Post-Cement Interface-adhesive- dentine system. Observe the uniform formation of ZIRD. The formation of long resinous tags and the presence of ramifications are evident.
Table 1 Amount of precipitates formed by the cements (gr).
| Groups | n | Media | Median | Minimum | Máximum | SD |
|---|---|---|---|---|---|---|
| ProRoot MTA | 10 | 0,9480 | 0,9500 | 0,8800 | 1,000 | 0,04658 |
| MTA Exp | 10 | 0,9000 | 0,8900 | 0,8700 | 0,9300 | 0,02449 |
Table 2 Descriptive Statistics of MIT Evaluation.
| Groups | n | Media | Median | Minimum | Máximum | SD |
|---|---|---|---|---|---|---|
| 1 (48h) | 8 | 0,0000 | 0,0000 | 0,0000 | 0,000 | 0,0000 |
| 2 (7 D) | 8 | 1,000 | 1,000 | 0,0000 | 2,000 | 0,4714 |
| 3 (15 D) | 8 | 2,300 | 2,000 | 2,000 | 3,000 | 0,4830 |
Table 3 Statistic Analyses of MIT Evaluation.
| Dunn´s Multiple Comparison Test | P <0.05 |
|---|---|
| 48 h vs 7 D | Yes* |
| 48 h vs 15 D | Yes*** |
| 7 D vs 15 D | Yes* |
Table 4 Descriptive Statistics of RDIZ Evaluation.
| Root third | n | Media | Median | Minimum | Maximum | SD |
|---|---|---|---|---|---|---|
| Cervical | 8 | 2,750 | 3,000 | 2,000 | 3,000 | 0,4629 |
| Medium | 8 | 2,625 | 3,000 | 2,000 | 3,000 | 0,5175 |
Discussion
The formation of precipitates began in the first hour after immersion of the samples in PBS and was observed for up to 35 days, forming a layer of precipitates all over the dentin. Both ProRoot MTA and MTA Exp promoted the formation of carbonated apatite precipitates on the surface of the samples, as observed in the images obtained by SEM. The background image (BI) showed the areas with greater calcification. These findings coincide with the data previously described by Reyes-Carmona et al (14), who reported the formation of carbonated apatite from crystalline maturation processes through an initial phase of amorphous calcium phosphate.
The ultrastructural evaluation and the SEM-EDAX chemical analysis allowed us to verify the presence of precipitates with different Ca/P proportions and forms. To a lesser extent, spherical precipitates with acicular extensions were observed. Tay et al (13) reported that these precipitates occur during the transformation of calcium phosphate into apatite, which is pH-dependent. The different precipitates are a consequence of the surface activity of the apatites that incorporate and substitute the elements into their structures, resulting in morphological alterations (29). In greater quantities, compact precipitates and agglomerates were observed; these precipitates have been described in the literature as lath-like layers (30,31,32). The number, size, and morphology of the precipitates may be related to the contact time of the cement with PBS (31).
Carbonate apatite is also known as biological apatite (33), which forms the mineral phase of hard tissue (bone, dentin, and cement); however, it does not have the same chemical composition as synthetic calcium hydroxyapatite - Ca10(PO4)6(OH)2. Carbonate apatite contains small amounts of magnesium, sodium, phosphorous, fluorine, and chlorine and has the following formula: (Ca,Mg,Na)10 (PO4HPO4CO3) 6(OH)2 (20).
At physiological pH, the formation of carbonated apatite can be described as a process that occurs in 2 stages (29). First, the Ca/P ratio is less than 1.5 and is associated with an increase in the pH of the solution. In the second stage, the Ca/P ratio increases, and the pH simultaneously decreases. As noted earlier in this study, the pH values (11.0-10.0) indicated the alkalinity of the solution. In the pH reading at 15 days, a decrease in pH was observed (8.8-8.7), which can be attributed to the incorporation of OH- ions released by the cements into the structure of the apatite (13, 34).
Based on this information, we can deduce that a calcium phosphate phase is initially formed, which acts as a precursor for the formation of carbonated apatite.
Bioactivity describes the ability of a material to interact with tissue and allow integration into the receiving environment. When a bioactive material is implanted, a series of biochemical and biophysical reactions occur at the implant-tissue interface, resulting in the formation of a layer of carbonated apatite (35). The bioactivity of MTA can be attributed to its ability to form carbonated apatite, which is important in the formation and maintenance of the material-bone tissue interface (32,36). This characteristic may explain the potential of MTA to stimulate the repair and deposition of mineralized tissue. The formation of apatite was confirmed on the dentin surface in both the ProRoot MTA and the MTA Exp groups; therefore, both materials can be considered bioactive cements.
Reyes-Carmona et al (1) reported that the use of PBS as an intracanal medication promotes the deposition of carbonated apatite, which generates MIT at the MTA-dentin interface. However, the authors used this medication for two months, which is a clinically unfeasible period, as this length of time increases the risk of recontamination of the pulp space and delays endodontic treatment.
Therefore, this part of the study analyzed PBS as an intracanal medication for different durations. From a clinical perspective and as observed in our study, the use of PBS as an intracanal medication for 15 days can promote a biomineralization process, enhancing an effect in the bond strenght and marginal infiltration, which are both important factors for the success of apexification treatment.
Induction of the biomineralization process in the internal part of the MTA apical plug is important because upon MIT formation, the resistance to displacement of the MTA with dentin significantly increase (16). Martin et al (17) observed that the interaction of the apical plug with PBS improves the marginal seal, thus avoiding microfiltration.
The previous generations of adhesive systems cause total/partial elimination of the smear layer and demineralization of the dentin by means of self-etch technique, revealing a network of collagen fibrils (28). Resin infiltration in this network allows the formation of a RDIZ with resin tags, thus causing micromechanical retention of the resin to the demineralized substrate (28,37, 38). The effectiveness of an adhesive system to achieve an RDIZ can be evaluated by using SEM to observe the uniformity and quality of RDIZs and the formation of the lateral branches at the interface between the system and the walls of the root dentin (28,38,39). This evaluation was performed because the formation of resin tags and RDIZs contributes to appropriate mechanical adhesion to the dentin and thus proper sealing (40). Additionally, based on previous studies (41,42), the adhesive resin cement systems that form an appropriate RDIZ exhibit less microinfiltration than traditional cements.
In our study, the use of the REBILDA® Post System, which uses a self-conditioning adhesive system, yielded an adequate RDIZ in the cervical and middle thirds of the radicular portion, including the formation of lateral branching. Our findings are consistent with those of Ross et al (19) who suggest the use of the REBILDA DC® Post System as an effective treatment for the restoration of teeth with endodontic treatment because it promotes adequate adhesion with intraradicular dentin.
Based on the data found in this analysis, we can affirm that the REBILDA® Post System is an adequate adhesive system and provides an appropriate marginal seal. Notably, the use of PBS as an intracanal medication does not seem to influence the interdiffusion ability of the adhesive system in dentin at any of the experimental time points. However, more ex vivo studies are needed to evaluate whether this system increases the fracture resistance of the dental element as per se.
Based on the results of our study, we can conclude that apexification with MTA combined with the use of PBS as an intracanal medication for 15 days, in addition to the use of the REBILDA® Post System, seems to be an effective restorative protocol for the treatment of teeth with incomplete rhizogenesis.














