INTRODUCTION
A dental anesthesia simulation model (DASM) offers students the opportunity to practice a local anesthesia technique and develop both psychomotor skills and confidence before going to direct patient care in a dental clinical setting (1). Learning with a DASM is safer for students than practicing on a human subject for the first time. In contrast, using the classical “student to student” learning model, in which a student performs an injection on a partner, involves a risk of injury as well as ethical issues (2,3,4,5). Therefore, a student learning with a DASM reduces risk of damage for the subject receiving the injection and avoids ethical concerns.
The DASMs have been investigated for teaching-learning impact on dental anesthesia, but the literature shows contradictory results regarding their effectiveness. The most common DASMs reported in the literature are those including a metallic electronic sensor (MES) located at an anatomical point that corresponds to the puncture site for blocking a nerve (6,7,8). With the DASMs plus MES, a student handles an anesthesia syringe with a dental needle to touch the puncture site, and when the metallic needle comes into contact with the MES, an audible signal indicates that the student has reached the right puncture site. That type of simulator is intended only to identify the puncture site, because the injection of an anesthetic solution might break the simulator’s electrical system (1). Brand et al. evaluated the effect of training with a DASM plus MES on the self-reported confidence of dental students after performing inferior alveolar nerve blocking (IANB) (7). The trained group and the non-trained group showed similar values of self-reported confidence (7). Marei et al. evaluated the efficacy of a DASM on dental students’ knowledge acquisition (8). Both the DASM-trained group and the non-trained group answered a written knowledge acquisition assessment; the two groups obtained similar scores in the clinical knowledge section of the assessment (8). However, Cabrera et al. observed that dental students increased their perception of learning when they trained for an anesthesia technique using a DASM before performing in a clinical setting (1). These inconsistent findings indicate more research is needed to determine the impact of DASMs on dental student perception of learning to confidently perform anesthesia techniques.
Some DASMs are manufactured like a simple typodont model with anatomical landmarks on which an injection can be performed with an anesthetic solution - they do not have an electronic system. To date, no study has explored that type of DASM. Training with a DASM designed for injection might have a positive impact on dental students’ perception of learning because the simulation of a puncture plus the injection of dental anesthesia could provide more psychomotor skills than the simulation of a puncture alone.
Choosing the most effective DASM is also important because they are a significant financial investment for universities, especially in newly industrialized countries. Because of contradictory information on the impact of simulation on how students learn to administer dental anesthesia, we investigated protocols for simulation-based learning (SBL) (1). In our dental school, we use the DASM plus MES and the typodont DASM to our knowledge those two DASMs have not been investigated to determine their impact on learning. Accordingly, the aim of our study was to compare the perception of learning by dental students trained with two distinct DASMs with dental students who were not trained with a DASM.
METHODS
We used two DASMs: 1) the conduction anesthesia model (CAM; Nissin Dental Products, Japan; Figure 1), and 2) the infiltration anesthesia jaw model (IAM; Nissin Dental Products; Figure 2). The CAM is a model with a metallic electronic sensor, and it is used for learning to puncture. The IAM is a model without a metallic electronic sensor and it is used for learning to puncture and inject.
The study was conducted in full accordance with the World Medical Association Declaration of Helsinki. All participants signed an informed consent, and an ethics committee approved the study (Identification approval: ID CEID-001A-2016- ver 1.0). The participants had never performed a dental anesthetic technique on a patient and had never used a DASM. Thirty-six healthy students in the 5-year undergraduate dental program of the School of Dentistry (Universidad Veracruzana) participated in the study. They reported no allergies to lidocaine, benzocaine or any other compound in a dental anesthesia solution. All participants had passed didactic courses on human anatomy, human physiology and dental anatomy; those courses are pre-requisites for the course of dental anesthesia. The students were randomly divided into three groups: Group 1,12 students with no training with a DASM (G1); Group 2,12 students trained with the CAM (G2); and Group 3,12 students trained with the IAM (G3).
THREE-STAGE LEARNING PROTOCOL
The protocol was performed to teach the technique for blocking the mental nerve (BMN) with anesthesia on teeth 44 and 45 (mandibular right first premolar and mandibular right second premolar) (9). We applied a three-stage learning protocol prior to the clinical practice: Stage-1, theoretical lecture; Stage-2, clinical demonstration; and Stage-3, DASM training (Table 1) (1). The professor of the dental anesthesia course (corresponding author) provided the instructions for the three stages of the learning protocol. The Stage-1 (theoretical information) was given by the professor in a classroom to all groups at the same time. The Stage-2 (clinical demonstration) was given by the professor in a clinic of the school of dentistry. Each group was separated into six participants to better assess student understanding of the technique. The clinical demonstration was done with a human subject on a dental chair as the six participants watched and heard the explanation immediately next to the dental chair. The Stage-3 (dental anesthesia simulation training) was given by the professor in a clinic for simulation of the school of dentistry. Each group was separated into six participants to better assess student understanding to the technique. Every participant then performed the DASM by himself or herself, following the protocol.
G1 followed the Stage-1 and the Stage-3 of the learning protocol. G2 and G3 followed three stages (Table 1). In the Stage-2, G2 used the CAM and G3 used the IAM. G2 used the DASM without practicing the injection, but the group received the explanation about placing the needle and performing the injection. The G3 used the DASM to practice the injection technique.
For Stages-2 and -3, the participants used dental syringes (M.A. Arain & Brothers, Pakistan). A cartridge of anesthetic solution - 2% lidocaine and 1:100,000 epinephrine (Zeyco S.A. de C.V., Mexico) - was used in Stages-2 and -3 for every repetition. Topic anesthesia was used in Stages-2 and -3 for every repetition (20% benzocaine, Zeyco S.A. de C.V). A dental needle (27G, short, Zeyco S.A. de C.V.) was used in Stages-2 and -3 for every repetition.
CLINICAL PRACTICE
After following the three-stage learning protocol, the participants performed the BMN using the student-to-student method: an operator performed the technique on a receptor, and after that the roles were reversed. G1 performed the BMN 24 hours after Stage-1. G2 and G3 performed the BMN 24 hours after Stage-2. For all groups, three students performed the BMN at the same time at a clinic with contiguous dental chairs so the professor could easily supervise the students, replicating the way we work in our dental anesthesia course.
MEASURING OF WORKING-TIME AND ANESTHESIA SUCCESS
Performance time is an indicator of the learning of psychomotor skills (10). Therefore, we tracked the working-time - in minutes and seconds - for each participant from the moment the student assembled the anesthesia cartridge and dental needle of the dental syringe until the student finished the BMN and recapped the dental needle. The success of the anesthesia was evaluated in terms of a positive or negative response to tetrahydrofluorethane spray (Hygenic Endo-Ice, Coltène-Whaledent, USA) administered five minutes after the BMN (11).
MEASURING OF THE PERCEPTION OF LEARNING
We defined perception of learning as the way you think about or understand someone or something. The definition of learning is: the activity or process of gaining knowledge or skill by studying, practicing, being taught, or experiencing something (12). In our study, perception of learning was defined as: the way the student thinks about the process of gaining knowledge or skill by experiencing with the DASM. A Likert Scale questionnaire is a suitable tool to measure the perception of learning; this study used this type of questionnaire to evaluate the impact of DASMs (1,6,7).
Immediately after finishing the BMN, the participants answered a 5-point Likert Scale with 8 items (Table 2). For positive items, the answers and values were as follows: totally disagree=1; partially disagree=2; don’t agree/don’t disagree=3; partially agree=4; and totally agree=5. For negative items, the answers and values were as follows: totally disagree=5; partially disagree=4; don’t agree/ don’t disagree=3; partially agree=2; and totally agree=1. The total scores of each test (n=12) from G1, G2 and G3 were compared to identify possible statistically significant differences (level of significance, P<0.05) with a one-way ANOVA and HSD Tukey test (13,14).
RESULTS
The average working-times for G1, G2 and G3 were 12:42 minutes (±2:08 minutes), 9:36 minutes (±1:12 minutes) and 8:03 minutes (± 1:04 minutes), respectively. Statistically significant differences were noted between G1 (Sig. = 0.000) and G2 (Sig.=0.023) and G3 (Sig.=0.000), as well as between G2 and G3. All participants achieved anesthesia at the first premolar and second premolar.
Table 3 shows the mean scores obtained from the 5-point Likert Scale. A one-way ANOVA test showed significant statistical differences between groups (p 0.010). Statistically significant differences were noted between G1 and G2 and G1 and G3 with a post hoc test (Table 4).

Figure 1 The conduction anesthesia simulation model (CAM) is a typodont with anatomical landmarks including the mandibular ramus. The simulation model is fixed to a phantom head which is then is mounted on the backrest of the dental chair (A). It includes an electronic device (B,#) that produces a signal when the dental needle touches the metallic electronic sensor (B,*).
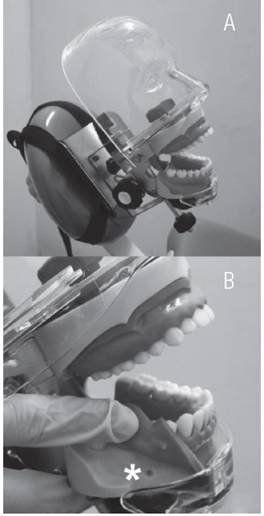
Figure 2 The injection anesthesia simulation model (IAM) is a typodont with anatomical landmarks and is designed for the practice of injecting anesthetic solution. The simulation model is fixed to a phantom head which is then is mounted on the headrest of the dental chair (A). The mental foramen (B) is visible next to the mark (*).
Table 1 Three-stage learning protocol in groups 1, 2 and 3.
| Stage | Topics | G1 | G2 | G3 |
| Theoretical lecture (40 minutes) | Anatomical considerations of the mental nerve. Localization of the anatomical puncture site and drying of the zone with a cotton tip. Application of topical anaesthesia and recommended contact time (two minutes). Assembly of the anaesthesia cartridge and dental needle on the aspirative dental syringe. Performing injection and recommended injection time (two min. per cartridge). Performing puncture and aspiration with the dental syringe. Re-capping the dental needle with the one-handed scoop technique. | Yes | Yes | Yes |
| Clinical demonstration (30 minutes) | Anatomical considerations of the mental nerve. Localization of the anatomical puncture site and drying of the zone with a cotton tip. Application of topical anaesthesia and recommended contact time (two minutes). Assembly of the anaesthesia cartridge and dental needle on the aspirative dental syringe. Performing injection and recommended injection time (two min. per cartridge). Performing puncture and aspiration with the dental syringe. Re-capping the dental needle with the one-handed scoop technique. | Yes | Yes | Yes |
| Dental anaesthesia simulation training 3 repetitions (30 minutes) | Anatomical considerations of the mental nerve. Localization of the anatomical puncture site and drying of the zone with a cotton tip. Application of topical anaesthesia and recommended contact time (two minutes). Assembly of the anaesthesia cartridge and dental needle on the aspirative dental syringe. Performing injection and recommended injection time (two min. per cartridge). Performing puncture and aspiration with the dental syringe. Re-capping the dental needle with the one-handed scoop technique. | No | Yes with CAM | Yes with IAM |
G1: group without training with a dental anesthesia simulation model, G2: group with training with the conduction anaesthesia simulation model (CAM). G3: group with training with the infiltration anaesthesia simulation model (IAM).
Table 2 Post-clinical questionnaire and mean scores of group 1 and 2, with items quantified on a five- point Likert scale.
| I easily identify the mandibular zone where the mental nerve runs. |
| I’m confident in doing the puncture and injection. |
| It takes a long time to manage the anesthetic technique. |
| My movements with the hand taking the syringe are controlled. |
| Localising the puncture site takes a long time. |
| I can do the mental nerve alveolar block again with no supervision. |
| I’m afraid of causing pain to the patient when I perform the injection. |
| I use great effort to control my hand in the direction of the injection site. |
Post-clinical questionnaire and mean scores of group 1 and 2, with items quantified on a five-point Likert scale The items explore the dental students’ perception of learning how to perform mental nerve blocking.
Table 3 Results of the Likert Scale for the 3 groups.
| Group | Mean score | Standard Deviation |
| 1 | 24.83 | 4.04 |
| 2 | 29.83 | 4.08 |
| 3 | 28.91 | 3.08 |
Group 1: group with no training with simulation model. Group 2: group trained with the conduction anesthesia simulation (CAM). Group 3: group trained with the infiltrative anesthesia simulation model (IAM).
DISCUSSION
We evaluated the impact of two different DASMs on the perception of learning by dental students. To explore the impact of the two distinct DASM on the perception of learning by dental students before injecting a subject for first time, we chose the BMN for the study because it is a simple technique compared with the IANB used by others in DASM research (6,8). The BMN was also chosen because it can be taught on the IAM or on the CAM. However, the IANB cannot be taught on the IAM because that model lacks a mandibular ramus and pterygomandibular zone.
Using a DASM should develop psychomotor skills to students, so it is expected that the student trained with a DASM will achieve the blocking of a nerve with a consequent anesthesia of the tissues. Regarding the success of the anesthesia in our study, all participants (100%) achieved anesthesia on teeth 44 and 45; success was defined as a negative response to a cold stimulus on the teeth.
Local dental anesthesia is a challenge, even for dental professionals; for example, the blocking of the inferior alveolar nerve is a technique that requires a high level of theoretical knowledge and operator skill to achieve success (15,16,17). The BMN is a simple technique, which contributed to the high success rate observed in the study. In our previous study, we also observed the success of anesthesia in a non-complex technique performed for the first time (1).
We measured the working time whereas other studies have not. Working-time is a variable that measures the development of technical motor skills. Newell et al. reported that technical motor skills are completed more quickly when an operator shows greater ability (13). The G1 did not train for the assembly of the anesthesia cartridge and dental needle on the aspirative dental syringe before performing the clinical exercise. G1 also did not train for the aspiration step and injection step. The longest working-time for G1 is explained because of the absence of practice. In contrast, G2 and G3 practiced the assembly of the syringe, and they also practiced the aspiration. G3 was the only one that also practiced the aspiration; as a result, G3 showed the shortest working-time. The practice of aspiration and injection steps (2 minutes/cartridge) are manual actions requiring controlled movements, and an advantage of using the IASM is the possibility of doing those two steps. The results agreed with those in our previous investigation. The students who trained with the DASM showed a shorter average working-time than that demonstrated by students without the DASM training (1).
The dental students’ perception of learning was evaluated with a Likert Scale; an analysis based on our previous questionnaire determined a Cronbach’s alpha of 0.86 (1). The mean total score for G2 and G3 was higher than that for G1, and statistically significant differences were noticed between the groups (Table 4). The results showed that the use of a DASM impacted positively on the perception of learning. The students in G2 and G3 had the chance to practice the anesthetic technique and psychomotor skills were developed during the DASM training. However, there were no statistically significant differences between the G2 and G3. The experience of using a DASM for G2 and G3 was good enough to improve the perception of learning. The step of injection by itself may be not as determinant on the perception of learning as we thought. The similar result between the G2 and G3 is explained because the training with a DASM developed self-confidence of the participant in those two groups (6).
Our results agree with those results reported by Lee et al. (6); they found that the use of a DASM positively impacted the levels of preparedness and confidence of dental students performing the inferior alveolar nerve blocking (6). Lee et al. also reported a well-described protocol for using the DASM. Other studies showed no impact of DASM on learning, but those studies have not reported learning protocols. In our experience, the success of the DASM is based on a well-designed learning protocol (1). Thus, DASMs are a helpful addition to the dental anesthesia curricula if a protocol is explored.
Our study had limitations. The number of participants might seem low; however, it has been recommended that dental simulation should be applied in small groups to facilitate learning (6,18). We were not able to avoid interaction between participants. The interaction amongst participants after performing any stage might also affect their idea about what is expected on the answers to Likert Scale (7). The G1 did not perform any pre-clinical practice, so its participation had the disadvantage of being incomplete in comparison to G2 and G3. That situation resulted in the longer working time noticed in the G1. Finally, the study did not evaluate the impact of the clinical setting of the dental students; as instance, we did not explore if the students required additional help from the professor.