Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista Costarricense de Cardiología
Print version ISSN 1409-4142
Rev. costarric. cardiol vol.19 n.1-2 San José Jan./Dec. 2017
Original work
National registry of heart failure in Costa Rica. The RENAIC CR study
1Programa de insuficiencia cardíaca, Hospital Clínica Bíblica, San José, Costa Rica; e-mail: sacagce@icloud.com
2 Servicio de Cardiología, Hospital San Vicente de Paul, C.C.S.S., Heredia, Costa Rica; e-mail: drdanielquesada@gmail.com
3Servicio de Cardiología, Hospital Max Peralta, C.C.S.S., Cartago, Costa Rica; e-mail: gcastillocr@yahoo.com
4Servicio de Cardiología, Hospital San Rafael, C.C.S.S., Alajuela, Costa Rica; e-mail: luislainez69@gmail.com
5Servicio de Cardiología, Hospital San Rafael, C.C.S.S., Alajuela, Costa Rica; e-mail: drmorasiglo21@gmail.com
6Servicio de Cardiología, Hospital Rafael A. Calderón Guardia, C.C.S.S., San José, Costa Rica; e-mail: cdbrenes@yahoo.com
7Servicio de Cardiología, Hospital Max Peralta, C.C.S.S., Cartago, Costa Rica; e-mail: drsoliscardiologo@gmail.com
8Servicio de Cardiología, Hospital Enrique Baltodano, C.C.S.S., Liberia, Costa Rica; e-mail: moisesvasquez29@gmail.com
9Servicio de Cardiología, Hospital México, C.C.S.S., San José, Costa Rica; e-mail: samiaao@gmail.com
10Servicio de Cardiología, Hospital Monseñor Sanabria, C.C.S.S., Puntarenas, Costa Rica; e-mail: natlozh@gmail.com
11Servicio de Cardiología, Hospital Max Peralta, C.C.S.S., Cartago, Costa Rica; e-mail: melissafrancisgomez@yahoo.com
Overall, it has been estimated that the prevalence of heart failure (HF) is approximately 1-2% of the adult population in developed countries. The prevalence of HF increases with age and the presence of other comorbidities 1-3. De spite improvements in the management of patients with HF that have led to a reduction of mortality and hospitalization rates in patients with HF with reduced ejection fraction, they remain unacceptably high 4. Thus, data from the ESC-HF pi lot study have shown that one-year all-cause mortality rates for chronic stable HF patients reach 7% and increase to 17% in hospitalized HF patients. In addition, one-year hospitaliza tion rates are markedly high (32% and 44%, respectively) 5. Moreover, costs associated to HF are huge and include infor mal care giving, health care costs and professional care. Over all, the main item corresponds to hospital costs, followed by cardiovascular medications 6.
However, it has been reported that there is significant regional variability in socioeconomic, clinical factors, etiolo gies and treatments in HF patients, leading to important dif ferences in prevalence, incidence and prognosis of patients with HF among different parts of the world 7-9. Since the information from one region of the world cannot be directly translated to other areas, it is mandatory to analyze the clini cal profile, risk factors, and management of patients with HF in every specific region.
Latin America (LA) is a heterogeneous region with HF risk factors of developed (i.e. diabetes, obesity, ageing, etc.) and nondeveloped countries (i.e. rheumatic fever, Chagas’ disease), and with a relative low total expenditure on health per capita, leading to significant differences in the prevalence and hospitalization and mortality rates compared with those reported in developed countries 10-12.
On the other hand, registries are useful to address some questions that hardly can be answered in randomized clinical trials, such as determining the clinical profile, risk factors, and the diagnostic and therapeutic approaches of patients with HF in daily clinical practice (13). The information provided from these registries may be particularly useful to develop different strategies in order to promote improvements in the diagnosis and management of patients with HF. Unfortunate ly, only a small number of registries of patients with HF have been developed in LA 7,14.
In order to improve the management and prognosis of patients with HF in Central America and the Caribbean, an international registry is being developed. The aim of the RE NAIC CR (REgistro Nacional de Insuficiencia Cardíaca en Costa Rica) registry is to analyze the clinical features, diagnostic and therapeutic approaches and evolution of patients with HF in Costa Rica.
Methods
The RENAIC CR is an ongoing, observational and prospective registry supported by the Cardiology Association of Costa Rica (Asociación Costarricense de Cardiología) and declared of public interest by the Ministry of Health of Costa Rica that is currently including HF patients from hospitals of Costa Rica. Outpatients and inpatients aged 18 years or older, of both sexes, with a diagnosis of HF attended at hospitals throughout Costa Rica are being consecutively included in this registry. The RENAIC CR registry has been approved by the Ministry of Health of Costa Rica. In this manuscript, the results recorded from February 2016 to February 2017 are presented. This is the first annual report of the RENAIC CR.
Data were collected from the medical history and physician interview and were entered into an electronic case report form specifically designed for this registry that ensured that all data were anonymous. Data from sociodemographic variables (age, sex, place of origin), cardiovascular risk fac tors (hypertension, dyslipidemia, sedentary lifestyle, diabe tes, smoking), vascular conditions (ischemic heart disease, HF hospitalizations, atrial fibrillation, chronic kidney disease, valve replacement, vascular disease, cerebrovascular dis ease), nonvascular comorbidities (chronic obstructive pul monary disease, thyroid disease, alcoholism, anemia, cancer), physical examination (blood pressure and heart rate), the etiology of HF, symptoms and functional class, complemen tary tests (electrocardiogram, chest X-ray, echocardiogram and recent blood analysis), precipitating factors, and cardio vascular medications and devices were recorded. No specific diagnostic or therapeutic intervention was performed during the study. The cause of death was taken from the death certificate recorded at the civil registry of Costa Rica.
Statistical analysis
A descriptive analysis was performed. Quantitative variables were described with measures of central tendency and dispersion (mean and standard deviation) and qualita tive variables were described as absolute (n) and relative (%) frequencies. The statistical analysis was performed using the SAS statistics package, version 9.4.
Results
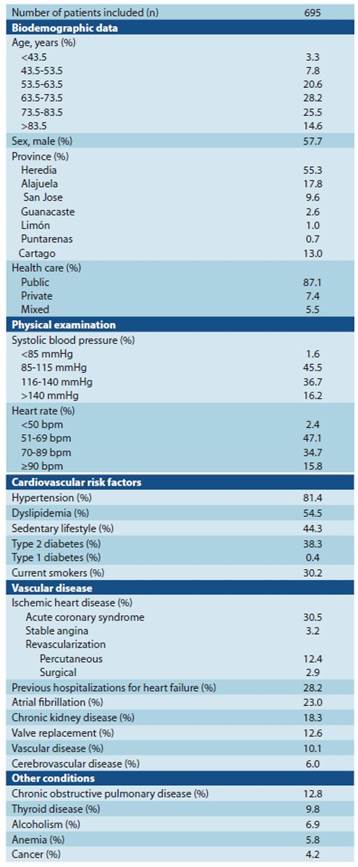
A total of 695 patients (68.3% were 63.5 years or older; 57.7% male) were included between February 2016 and Fe bruary 2017. Most patients (87.1%) were attended in the public health care system. The presence of cardiovascular risk factors and other comorbidities was very common. The most frequent cardiovascular risk factors were hypertension (81.4%), followed by dyslipidemia (54.5%). With regard to oth er comorbidities, 30.5% of patients had a history of previous acute coronary syndrome and 23.0% atrial fibrillation. A total of 196 (28.2%) patients had at least one previous admission for HF, of whom 77 (39.3%) patients had one hospitalization for HF and 13 (6.6%) patients two hospitalizations for HF (Table 1).
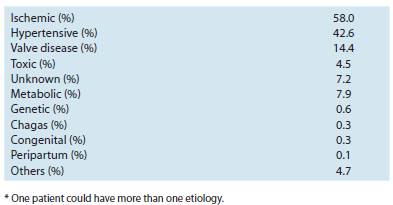
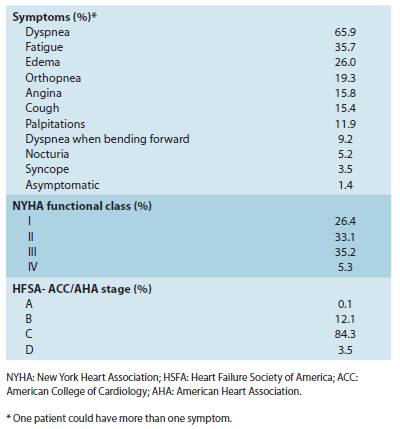
With regard to the etiology of HF, the most common cause was ischemic heart disease (58.0%), followed by hy pertension (42.6%). In only 0.3% of cases, Chagas´ disease was the cause of HF (Table 2). Most patients were on NYHA functional class II (33.1%) or III (35.2%) and on HFSA-ACC/ AHA stage C (84.3%). Dyspnea was the most common symp tom (65.9%), followed by fatigue (35.7%) (Table 3). Overall, 68.0% of patients were considered as stable, 26.1% had ve nous congestion, 4.7% acute pulmonary edema, and 1.2% cardiogenic shock.
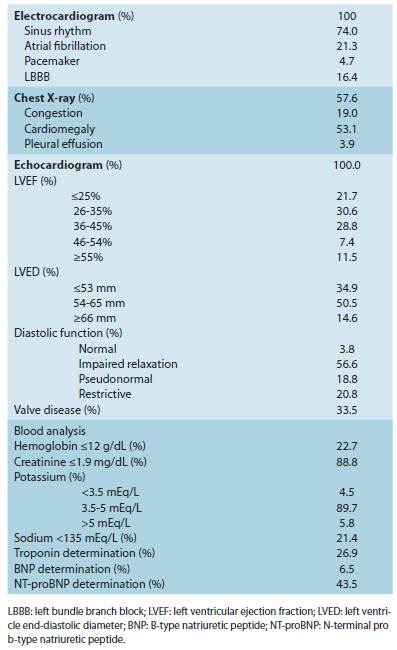
At the moment of inclusion in the registry, all patients had an electrocardiogram and an echocardiogram per formed. 81.1% of patients had left ventricular ejection fraction <45% and 52.3% <35%. Almost all patients (96.2%) had diastolic dysfunction. 22.7% of patients had anemia, and 5.8% hyperkalemia. BNP was determined in 6.5% of patients and NT-proBNP in 43.5% of patients (Table 4).
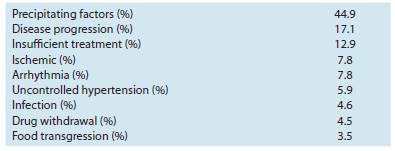
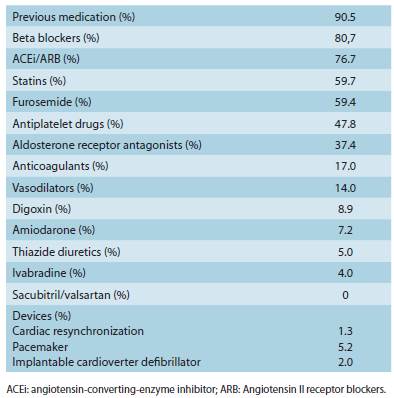
A precipitating factor leading to decompensation of HF was identified in 44.9% of patients (Table 5). The most com mon precipitating factor was disease progression (17.1%) fol lowed by insufficient treatment (12.9%). At the moment of inclusion in the registry, the majority of patients were receiv ing at least one cardiovascular medication (90.5%). 80.7% of patients were taking beta blockers, 76.7% angiotensin-con verting-enzyme inhibitor or angiotensin II receptor blockers and 37.4% aldosterone receptor antagonists (Table 6). 208 (29.9%) of patients were included in a hospital-based HF program. During the follow-up period, 5.3% of patients died.
Discussion
The RENAIC CR is the first registry that has included pa tients with HF from Costa Rica, and one of the first registries performed in patients with HF in LA. The information provid ed by RENAIC CR is of great value, since it allows determining the current situation of HF patients in Costa Rica and similar countries in order to detect improvement areas in the man agement of this population.
With regard to the clinical profile of patients with HF in cluded in different registries, in the EuroHeart Failure survey, 51% of women and 30% of men were aged >75 years and 53% of patients were men 15. In the Spanish RICA registry, mean age was 78 years, 47% were men, 85% of patients had hypertension, 44% diabetes, 54% atrial fibrillation, 22% prior myocardial infarction and 31% chronic kidney disease 16. In the I Brazilian Registry of HF, mean age was 64 years, 40% were men, and 71% of patients had hypertension, 34% diabetes, 27% atrial fibrillation, 27% prior myocardial infarction and 24% chronic kidney disease 14. In the INTER-CHF study, mean age was 53, 60, 56 and 67 years in those patients included in Africa, Asia, Middle East and South America, re spectively. The majority of patients were men (52%, 59%, 72% and 61%, respectively), 62%, 59%, 68% and 74%, respectively, had hypertension, 17%, 28%, 56% and 22%, respectively, dia betes, 8%, 22%, 19% and 18%, respectively prior myocardial infarction and 4%, 7%, 12% and 12%, respectively, chronic kidney disease 7. In our registry, 68% of patients were ≥63.5 years and 40% ≥73.5 years. The majority of patients were male (58%) and the presence of cardiovascular risk factors (81% had hypertension and 39% diabetes) and other co morbidities (31% had prior myocardial infarction, 23% atrial fibrillation and 18% chronic kidney disease) was very com mon. In summary, there are important disparities regarding the clinical profile of patients with HF according to the region of origin. In developed countries, patients are older and the presence of cardiovascular risk factors such as hypertension or diabetes or other comorbidities such as previous myocardial infarction or chronic kidney disease is usually more com mon than in emerging countries. These differences may lead to disparities in the prevalence and outcomes of HF patients and the need for developing specific strategies for the early diagnosis of HF adapted to each region of the world 17. Data from our registry strongly suggest that patients from Costa Rica share characteristics of both scenarios, developed and emerging countries.
In the INTER-CHF registry, ischemic heart disease was the most common HF etiology (26%), followed by hyperten sive heart disease (21%), idiopathic dilated cardiomyopathy (15%) and rheumatic valvular heart disease (6%), but with im portant regional variations 7. In the BREATHE registry, these numbers were 30%, 20%, 15% and 12%, respectively. Remark ably, Chagas` disease was the cause of HF in 11% of patients 14. In our study, the most common cause of HF was ischemic heart disease (58.0%), followed by hypertension (43%), and in only 0.3% of cases, Chagas` disease was considered as the underlying cause of HF. The disparities found in the percent ages of these studies may be related with differences in the clinical profile of patients included in the registries. In addition, it is well known that in contrast to other countries of LA, Chagas` disease is not endemic in Costa Rica 12. Moreover, it has been reported that when the registries are performed in decompensated HF hospitalized patients, ischemic heart disease is more common as the underlying cause of HF than when the registries are performed in outpatients 10.
In the EuroHeart Failure survey, 37% of patients were on NYHA functional class II, and 26% on NYHA functional class III/IV 15. In the RICA registry, among patients with left ven tricular ejection fraction <50%, 40% were on NYHA func tional class II and 44% on NYHA functional class III 16. In the INTER-CHF registry, in South America, 49% of patients were on NYHA functional class II and 26% on NYHA func tional class III, but with relevant variations when compared with the other regions 7. In our study, most patients were on NYHA functional class II (33%) or III (35%). Dyspnea was the most common symptom (66%), followed by fatigue (36%). This means that the majority of patients with HF have symptoms that are easily identifiable. Unfortunately, many patients with HF are underdiagnosed, particularly in elderly 18,19. On the other hand, since up to 26% were on NYHA functional class I, in those asymptomatic patients but with HF risk factors, and active search for the early diagnosis of HF should be performed 1.
In contrast to the EuroHeart Failure survey and RICA registry in which 46% and 41%, respectively, had systolic HF (15,16), this percentage increased to 59% in the BREATHE study (14) and 74% in the INTER-CHF registry 7. In our reg istry, 81% of patients had left ventricular ejection fraction <45% and 52% <35%. This is not surprising, since HF with pre served left ventricular ejection fraction is associated with el derly 19 that is more common in developed countries than in emerging countries 20.
With regard to the complementary tests, previous reg istries have shown that in a high proportion of HF patients, an echocardiogram is not performed (34% in the EuroHeart Failure survey, and 19% in the INTER-CHF study) 7,15. By contrast, in our registry all patients had an echocardiogram performed. This is very relevant, since the echocardiogram is a basic tool for the diagnosis and management of patients with HF 1, and our data suggest that fortunately, physicians are more conscious about the importance of performing an echocardiogram in HF patients.
On the other hand, natriuretic peptides are very use ful for the early diagnosis of HF and the management of HF patients during the follow-up 1. Unfortunately, their use in clinical practice is lower than required 21. In our study, pep tide natriuretics were determined in approximately half of patients. As a result, more efforts are needed to increase the implementation of these techniques (echocardiogram and natriuretics peptides) in clinical practice.
In the BREATHE registry, the main causes of HF decom pensation were poor adherence to medication (30%), fol lowed by infections (23%) 14. In the EuroHeart Failure survey, cardiac chest pain and arrhythmias accounted for 59% of the primary reasons for admission. Also, respiratory infection was an important contribution to admissions in some countries 15. In our study, the most common precipitating factor was disease progression (17%) followed by insufficient treatment (13%). It is important to know the most common precipitat ing factors, in order to reduce the risk of decompensation 22. However, as in our study, in nearly half of patients with decompensated HF no precipitating factor can be identified.
A number of studies have shown that many patients with HF do not receive evidence-based drug treatment, and when prescribed, the dosage used is lower than recommended 23-25. In the EuroHeart Failure survey, angiotensin-convert ing-enzyme inhibitors were prescribed in 62% of patients, beta-blockers in 37% and spironolactone in 21%. Only 17% of patients were under the combination of diuretic, angioten sin-converting-enzyme inhibitors and beta-blockers 25. In the INTER-CHF study, the use of beta blockers ranged from 48% in Africa to 86% in Middle East, the prescription of angio tensin-converting-enzyme inhibitors or angiotensin receptor blockers from 68% in Asia to 82% in Middle East and in the case of aldosterone inhibitors, from 44% in Asia to 59% in Af rica 7. In the BREATHE study, beta blockers were prescribed in 57% of patients, angiotensin converting enzyme inhibitors or angiotensin II receptor blockers in 66% and aldosterone antagonists in 46%. In addition, only 64% of the patients received advice about the correct use of these drugs 14. In our study, although cardiovascular drugs have been op timized during the follow-up, at the moment of inclusion in the registry, 81% of patients were taking beta blockers, 77% angiotensin-converting-enzyme inhibitor or angiotensin II receptor blockers and 37% aldosterone receptor antagonists. Importantly, in our registry, nearly 30% of patients were in cluded in a hospital-based HF program. Although this per centage is suboptimal, is much higher than that reported in Central America and Caribbean countries, despite the impact of hospital-based HF programs on improving the manage ment of this population 26. In summary, although in the last years there has been an improvement in the prescription of evidence-based HF therapies, it remains far from optimal, not only with regard to the proportion of patients taking beta blockers or renin angiotensin aldosterone system inhibitors, and the insufficient doses taken, but also with regard to the low use of cardiac devices or the small proportion of patients included in hospital-based HF programs 26. In addition, these efforts should not be limited to cardiologists, but also to all physicians that attend this high risk population 27.
The main limitation of the study comes from the design of this type of studies, without a control group. However, this is the best design to represent the “real world” clinical practice that actually was the aim of this study. Since physicians included patients voluntarily, the information provided in our study may not represent accurately the whole population of HF patients attended in Costa Rica. In addition, our data could only be extended to those countries with a similar health care system and clinical profile of patients.
Conclusions
The RENAIC CR is the first registry performed in HF pa tients in Costa Rica, and one of the first registries in LA. Nearly 700 patients were included in this registry. The presence of cardiovascular risk factors and other comorbidities was very common. The most common underlying cause of HF was isch emic heart disease, followed by hypertension. Most patients were on NYHA functional class II or III. Although in all patients with HF an echocardiogram was performed, in half of these patients natriuretic peptides were not determined. In about 55% of patients a precipitating factor leading to decompen sation of HF was not identified. At the moment of inclusion in the registry, nearly 20%, 25% and 63% of HF patients were not taking beta blockers, angiotensin-converting-enzyme inhibitor or angiotensin II receptor blockers and aldosterone receptor antagonists, respectively. The information provided by this registry may be very helpful for developing different strategies in order to improve the management of patients with HF in Costa Rica and similar countries of the region.
Summary points
Introduction. There is significant regional variability in socioeconomic, clinical factors, etiologies and treatments in HF patients. It is mandatory to analyze the clinical profile, risk factors, and manage ment of patients with HF in every specific region. The aim of the RENAIC CR registry is to analyze the clinical features, diagnostic and therapeutic approaches and evolution of patients with HF in Costa Rica.
Methods. The RENAIC CR is an ongoing, observational and prospective registry that is currently including HF patients from hospitals of Costa Rica. The results recorded from February 2016 to February 2017 are presented in this manuscript. This is the first annual report of the RENAIC CR.
Results. Nearly 700 patients (68.3% ≥63.5 years; 57.7% male) were included in this registry. The presence of cardiovascular risk factors and other comorbidities was very common. The most common underlying cause of HF was ischemic heart disease (58.0%), followed by hypertension (42.6%). Most patients were on NYHA functional class II (33.1%) or III (35.2%). Although in all patients with HF an echocardiogram was performed, in half of these patients natriuretic peptides were not determined. In about 55% of patients a precipitating factor leading to decompensa tion of HF was not identified. At the moment of inclusion in the registry, nearly 20%, 25% and 63% of HF patients were not taking beta blockers, angiotensin-converting-enzy me inhibitor or angiotensin II receptor blockers and aldosterone receptor antagonists, respectively.
Discussion. The RENAIC CR is the first registry that has included patients with HF from Costa Rica, and one of the first registries performed in patients with HF in LA. Data from our registry strongly suggest that patients from Costa Rica sha re characteristics of both scenarios, developed and emerging countries. In line with other studies, underdiagnosis and undertreatment is com mon in HF patients in Costa Rica.
Conclusion. The information provided by this registry may be very helpful for develo ping different strategies in order to improve the management of patients with HF in Costa Rica and similar countries of the region.
Acknowledgements:
Editorial assistance was provided by Content Ed Net, Madrid, Spain. Accomplished with financial support from NOVARTIS® pharmaceutical company, and given to Costa Rican Car diology Association. It is declared there is no conflict of interest in the investigation development. Graphic design and page layout by Sergio Aguilar Mora.
REFERENCES
Ponikowski P, Voors AA, Anker SD et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart. J. 37(27), 2129-2200 (2016). [ Links ]
Mosterd A, Hoes AW. Clinical epidemiology of heart failure. Heart. 93(9), 1137-1146 (2007). [ Links ]
Bleumink GS, Knetsch AM, Sturkenboom MCJM, et al. Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk and prognosis of heart failure The Rotterdam Study. Eur. Heart. J. 25(18), 1614-1619 (2004). * Este estudio demostró que casi 1 de cada 3 individuos de 55 años de edad desarrollará IC durante el seguimiento. Transcurridos 5 años desde el primer diagnóstico de IC, sólo el 35% permanece con vida. [ Links ]
Bergethon KE, Ju C, DeVore AD et al. Trends in 30-Day Readmission Rates for Patients Hospitalized With Heart Failure: Findings From the Get With The Guidelines-Heart Failure Registry. Circ. Heart. Fail. 9(6) (2016). * En este estudio se informó una leve mejoría en las tasas de readmisión por todas las causas a 30 días durante los últimos 4 años en pacientes con IC. [ Links ]
Maggioni AP, Dahlström U, Filippatos G et al. EURObservational Research Programme: regional differences and 1-year follow-up results of the Heart Failure Pilot Survey (ESC-HF Pilot). Eur. J. Heart. Fail. 15(7), 808-817 (2013). [ Links ]
Delgado JF, Oliva J, Llano M et al. Health care and nonhealth care costs in the treatment of patients with symptomatic chronic heart failure in Spain. Rev. Esp. Cardiol. (Engl Ed). 67(8), 643-650 (2014). * Este estudio demostró que los costos asociados con la IC eran altos, principalmente los costos hospitalarios y de la medicación. [ Links ]
Dokainish H, Teo K, Zhu J et al. Heart Failure in Africa, Asia, the Middle East and South America: The INTER-CHF study. Int. J. Cardiol. 204, 133-141 (2016). * En este estudio se informó una variabilidad regional significativa en los factores socioeconómicos y clínicos, en las etiologías y en los tratamientos en pacientes con IC de diferentes regiones del mundo. [ Links ]
Pfeffer MA, Claggett B, Assmann SF et al. Regional variation in patients and outcomes in the Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist (TOPCAT) trial. Circulation. 131(1), 34-42 (2015). [ Links ]
Kristensen SL, Martinez F, Jhund PS et al. Geographic variations in the PARADIGM-HF heart failure trial. Eur. Heart. J . 37(41):3167-3174 (2016). [ Links ]
Bocchi EA, Arias A, Verdejo H et al. The reality of heart failure in Latin America. J. Am. Coll. Cardiol. 62(11), 949-958 (2013). [ Links ]
Ciapponi A, Alcaraz A, Calderón M et al. Burden of Heart Failure in Latin America: A Systematic Review and Meta-analysis. Rev. Esp. Cardiol. (Engl Ed). 69(11), 1051-1060 (2016). * Este estudio demostró que la IC está asociada con altas tasas de mortalidad y hospitalización en AL. [ Links ]
Bestetti RB. Chagas Heart Failure in Patients from Latin America. Card. Fail. Rev. 2(2), 90-94 (2016). [ Links ]
Trullàs JC, Miró Ò, Formiga F et al. The utility of heart failure registries: a descriptive and comparative study of two heart failure registries. Postgrad. Med J. 92(1087):260-6 (2016). [ Links ]
Albuquerque DC, Neto JD, Bacal F et al. I Brazilian Registry of Heart Failure - Clinical Aspects, Care Quality and Hospitalization Outcomes. Arq. Bras. Cardiol. 104(6), 433-442 (2015). * Este registro informó una alta mortalidad intrahospitalaria en los pacientes admitidos con IC aguda en Brasil, debido en parte al subtratamiento de esta población. [ Links ]
Cleland JG, Swedberg K, Follath F et al. The EuroHeart Failure survey programme-- a survey on the quality of care among patients with heart failure in Europe. Part 1: patient characteristics and diagnosis. Eur. Heart. J . 24(5), 442-463 (2003). [ Links ]
Ruiz-Laiglesia FJ, Sánchez-Marteles M, Pérez-Calvo JI et al. Comorbidity in heart failure. Results of the Spanish RICA Registry. QJM. 107(12), 989- 994 (2014). [ Links ]
Dokainish H, Teo K, Zhu J et al. Global mortality variations in patients with heart failure: results from the International Congestive Heart Failure (INTER-CHF) prospective cohort study. Lancet. Glob. Health. 5(7), e665-e672 (2017). [ Links ]
Barrios V, Escobar C, De La Sierra A, Llisterri JL, González-Segura D. Detection of unrecognized clinical heart failure in elderly hypertensive women attended in primary care setting. Blood. Press. 19(5), 301-307 (2010). [ Links ]
Manzano L, Escobar C, Cleland JG, Flather M. Diagnosis of elderly patients with heart failure. Eur. J. Heart. Fail. 14(10), 1097-1103 (2012). [ Links ]
Kim Y. The dynamics of health and its determinants among the elderly in developing countries. Econ. Hum. Biol. 19, 1-12 (2015). [ Links ]
Januzzi JL, Troughton R. Are serial BNP measurements useful in heart failure management? Serial natriuretic peptide measurements are useful in heart failure management. Circulation. 127(4), 500-507 (2013). [ Links ]
Velavan P, Khan NK, Goode K et al. Predictors of short term mortality in heart failure - insights from the Euro Heart Failure survey. Int. J. Cardiol. 138(1), 63-69 (2010). [ Links ]
Lenzen MJ, Boersma E, Reimer WJ et al. Under-utilization of evidence-based drug treatment in patients with heart failure is only partially explained by dissimilarity to patients enrolled in landmark trials: a report from the Euro Heart Survey on Heart Failure. Eur. Heart. J . 26(24), 2706-2713 (2005). * En este estudio se informó subutilización de tratamiento farmacológico basado en la evidencia en pacientes con IC por parte de los cardiólogos europeos. [ Links ]
Drechsler K, Dietz R, Klein H et al. Euro heart failure survey. Medical treatment not in line with current guidelines. Z. Kardiol. 94(8), 510-515 (2005). [ Links ]
Komajda M, Follath F, Swedberg K et al. The EuroHeart Failure Survey programme--a survey on the quality of care among patients with heart failure in Europe. Part 2: treatment. Eur. Heart. J . 24(5), 464-474 (2003). [ Links ]
Cowie MR, Lopatin YM, Saldarriaga C et al. The Optimize Heart Failure Care Program: Initial lessons from global implementation. Int. J. Cardiol. 236, 340-344 (2017). [ Links ]
Tavares LR, Velarde LG, de Miranda VA, Mesquita ET. Perceptions of heart failure diagnosis and management: comparison between clinical cardiologists and family doctors. Arq. Bras. Cardiol. 87(2), 167-173 (2006). * En comparación con los médicos clínicos, los cardiólogos usan métodos de diagnóstico y tratamiento más intensivos en pacientes con IC [ Links ]
Received: October 24, 2017; Accepted: November 22, 2017











 text in
text in