Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Médica Costarricense
versión On-line ISSN 0001-6002versión impresa ISSN 0001-6012
Acta méd. costarric vol.63 no.3 San José jul./sep. 2021
http://dx.doi.org/10.51481/amc.v63i3.1162
Original
Pancreatic coristoma within a duodenal diverticulum: a case report
1Universidad Privada San Juan Bautista, Facultad de Medicina; Asociación de Investigación y Ciencia de los Estudiantes de Medicina de la UPSJB ICA. Ica, Perú. 0000-0001-9366-0611
2Hospital Regional de Ica, Servicio de Gastroenterología; Departamento de Medicina Interna. Ica, Perú. 0000-0002-6471-2491
3Hospital Regional de Ica, Departamento de Medicina Interna. Ica, Perú. 0000-0003-0181-2345
4Hospital Regional de Ica, Departamento de Cirugía. Ica, Perú. 0000-0001-5189-1286
Pancreatic choristoma or also called heterotopic pancreas (HP) is a rare pathology in gastroenterology.1 It consists of the presence of aberrant pancreatic tissue in an area of the gastrointestinal tract where it should not be found, also without vascular or anatomical continuity with the organ itself, this is due to embryogenesis of the tissue in that area without a specific cause.2-4
There are few reports of this condition worldwide.5 It usually has no symptoms during childhood, and in adulthood they are variable; there have been reported cases of patients who debut with upper gastrointestinal bleeding, and others whose only sign is chronic abdominal pain.3, 6
The definitive diagnosis is histopathologic.2, 5, 7 Regarding treatment, surgery remains the best option to avoid the malignant evolution of the aberrant tissue.8
We present the case of a patient with chronic abdominal pain secondary to ectopic pancreatic tissue within a duodenal diverticulum.
Clinical case
Male, 46 years old, from Ica, with no pathologic or surgical history. The disease started six months before his admission with epigastric pain associated with a five kilograms weight loss during those months. He consults Gastroenterology because, during the last week, he has had premature fullness and episodes of emesis of biliary content, of moderate quantity, in addition to the previous symptoms.
Physical examination revealed superficial and deep palpation pain in the epigastrium, with no other findings. An upper gastrointestinal endoscopy was performed, showing a tumor lesion with central depression on the anterior wall of the duodenal bulb, approximately 3 cm in diameter, which was biopsied. A complete abdominal CT scan with contrast was performed showing the same saccular image in the bulb, which was then diagnosed as a duodenal diverticulum (Figure 1).
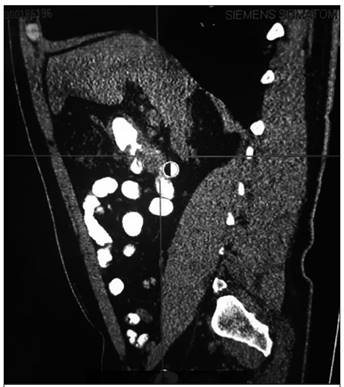
Figure 1 Enterotem with contrast in the anterior face of the duodenal bulb shows a saccular image approximately 2 cm in diameter (ARROW).
An exploratory laparotomy was performed to define the histology of the lesion. A 3.5 cm x 2.5 cm wide-based, hyper vascularized, and the edematous saccular tumor was found, originating in the inferior face of the pylorus, with projection to the gastric area. Diverticulectomy was performed followed by Finney pyloroplasty.
The histopathological study showed in the muscularis propria numerous ducts grouped in lobules and separated from each other by thick and irregular bundles of smooth muscle and dense connective tissue; also, the presence of islets of Langerhans compatible with pyloric pancreatic choristoma (Figures 2 and 3).,
The tissue was positive for CK AE1/AE3 (cytokeratins for the identification of keratins and basal) by immunohistochemistry, indicating the presence of two epithelia, both duodenal and pancreatic in the sample (Figure 4); while the chromogranin and synaptophysin studies were negative a fact that ruled out neuroendocrine tumors (Figures 5 and 6). This led to the final diagnosis of a complete type I pancreatic heterotopia. The patient evolved favorably from the procedure and to date is stable.
We have the patient’s informed consent for the preparation and publication of this article.
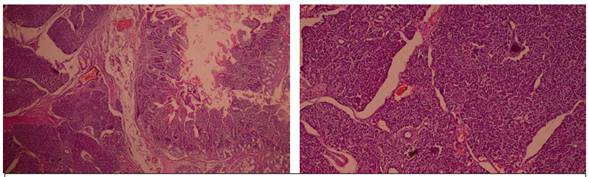
Figures 2 and 3. In the muscularis propria, numerous ducts grouped in lobules and separated by thick and irregular bundles of smooth muscle and dense connective tissue are observed; in addition, there are some islets of Langerhans. The histopathological picture is compatible with pyloric pancreatic choristoma.
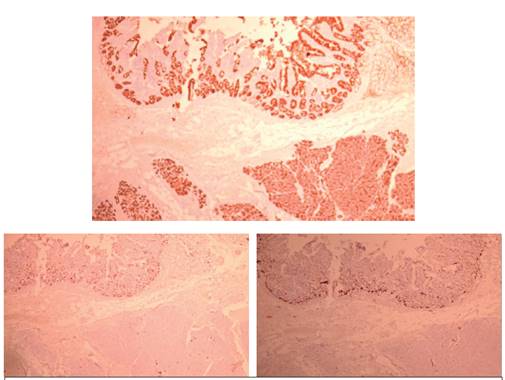
Figures 4, 5, and 6. In the immunohistochemical study, CK AE1/AE3 was positive. While in the immunohistochemical study of chromogranin.
Discussion
Choristomas are common in the gastrointestinal tract and are found incidentally during imaging examinations such as CT scans and invasive examinations such as endoscopy.9
Heterotopic tissue can occur at any location along the gastrointestinal tract, with the most frequent sites being the stomach and small intestine.1 The aberrant or heterotopic pancreas is an isolated mass of pancreatic tissue, completely separated from the main organ, where its embryogenesis occurs, but its mode of development is unknown.3, 4
Approximately 5% of the world’s population suffers from this condition and the symptomatology does not occur in childhood, but between 40 and 60 years of age; as in the case of our patient.5 Pancreatic ectopia is rarely reported in the literature, while the signs and symptoms depend on the organ affected, with the stomach (30%), duodenum (25%), jejunum (16%), ileum (2.8%), and rarely esophagus being affected, with about 20 cases reported in the literature. 10-13 Among the cases of aberrant pancreatic tissue found in the duodenum, the case reports mention a preponderance of localization in the second portion of the duodenum.14, 15
The definitive diagnosis is by biopsy, which must be done to rule out malignancy or to define specific inflammatory causes.16 Sometimes there are alterations in the underlying tissues such as inflammation, fat necrosis, and diverticulum formation.7
In 1973, Gaspar Fuentes and collaborators, based on the old criteria of von Heinrich, proposed a new four types classification2, shown below, based on the structures of the pancreas found in this heterotopic tissue: type I (atypical pancreas (complete heterotopia)), which corresponds to our case. type II, only with pancreatic ducts (canalicular heterotopia), type III, with acinar cells only (exocrine heterotopia) and type IV, only with islets of Langerhans (endocrine heterotopia).
On the other hand, complications of this disease include pancreatitis, intussusception formation, intestinal obstruction, gastrointestinal bleeding, malignant degeneration, and pseudocysts. 17
Regarding treatment, surgical resection of the aberrant tissue remains the best option3. We are aware of the possibility of malignant degeneration that this ectopic tissue may undergo and that is why it is suggested to preventively monitor the patient periodically after the surgical procedure, to detect possible recurrences, although this is rare and little reported.8, 9
Conclusions
Despite its rarity, pancreatic choristoma should be considered within the possibilities of abdominal mass or chronic pain in adult patients.
Acknowledgments: To Dr. Pedro Salvador Antonio Travezan, for providing the histopathologic images.
Abbreviations: heterotopic pancreas (HP).
Sources of support: self-financed.
Conflict of interest: the authors declare no conflict of interest. jesus.24.47.1996@gmail.com /
jesus_24_47@hotmail.com
Referencias
1. Offner FA, Langner C. Heterotopic tissue in the gastrointestinal tract. Pathologe. 2018;39:402-408. [ Links ]
2. Bromberg SH, Camilo Neto C, Borges AF, Franco MI, França LC, Yamaguchi N. Pancreatic heterotopias: clinicopathological analysis of 18 patients. Rev Col Bras Cir. 2010; 37:413-9. [ Links ]
3. Betzler A, Mees S, Pump J, Schölch S, Zimmermann C, Aust D, et al. Clinical impact of duodenal pancreatic heterotopia - Is there a need for surgical treatment? BMC Surg. 2017; 17: 53. [ Links ]
4. Calabrese E, Lolli E, Maccioni F, Poggioli G. Complete heterotopic pancreas. Dig Liver Dis. 2018; 50: 969. [ Links ]
5. Zhang Y, Sun X, Gold JS, Sun Q, Lv Y, Li Q, et al. Heterotopic pancreas: a clinicopathological study of 184 cases from a single high- volume medical center in China. Hum Pathol. 2016;55:135-42. [ Links ]
6. Kim DU, Lubner MG, Mellnick VM, Joshi G, Pickhardt PJ. Heterotopic pancreatic rests: imaging features, complications, and unifying concepts. Abdom Radiol (NY). 2017; 42:216-225. [ Links ]
7. Rezvani M, Christine M, Sandrasegaran K, Olpin JD, Elsayes KM, Shaaban AM. Heterotopic Pancreas: Histopathologic Features, Imaging Findings, and Complications. Radiographics. 2017; 37:484-499. [ Links ]
8. Jun SY, Son D, Kim MJ, Kim SJ, An S, Park YS, et al. Heterotopic Pancreas of the Gastrointestinal Tract and Associated Precursor and Cancerous Lesions: Systematic Pathologic Studies of 165 Cases. Am J Surg Pathol. 2017;41:833-848. [ Links ]
9. Johncilla M, Yantiss RK. Malformations, choristomas, and hamartomas of the gastrointestinal tract and pancreas. Semin Diagn Pathol. 2019; 36:24-38. [ Links ]
10. Aslan S, Nural MS. CT features of asymptomatic heterotopic pancreas in jejunal mesentery. Turk J Gastroenterol 2019;30:208-10. [ Links ]
11. Schiappacasse G, Villacrés F, Cavalla C, Orellana F, Gallardo A, Charles R. Pseudoquiste de páncreas intramural gástrico como causa de retención gástrica. Rev Med Chile 2018;146: 933-937. [ Links ]
12. Xiang S, Zhang F, Xu G. Ectopius pancreas in the ilium: An unusual condition and our experience. Medicina (Baltimore). 2019; 98:e17691. [ Links ]
13. Trifan A, Târcoveanu E, Danciu M, Huţanaşu C, Cojocariu C, Stanciu C. Gastric heterotopic pancreas: an unusual case and review of the literature. J Gastrointestin Liver Dis 2012; 21:209-12. [ Links ]
14. Chin KM, Tanb D, Chanc N, Goha B. Successful preoperative diagnosis of heterotopic pancreas in the duodenum. Int J Surg Case Rep. 2019; 55:125-128. [ Links ]
15. Li J, Huang H, Huo S, Liu Y, Xu G, Gao H, et al. Ectopic pancreatic tissue in the wall of the small intestine: Two rare case reports. Medicine (Baltimore). 2017;96: e7986. [ Links ]
16. Bazán-Zender C, Reyes-Coloma L, León-Cueto JL, Revoredo-Palacios G, Arias-Stella Castillo J, Pezo A. Páncreas heterotópico como causa de invaginación intestinal: primer caso reportado en el Perú. Rev Peru Med Exp Salud Publica. 2015;32:598-602. [ Links ]
17. Cazacu IM, Luzuriaga-Chavez AA, Nogueras- Gonzalez GM, Saftoiu A, Bhutani MS. Malignant Transformation of Ectopic Pancreas. Dig Dis Sci. 2019;64:655-668 [ Links ]
Received: August 07, 2021; Accepted: November 30, 2021











 texto en
texto en 



