Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Médica Costarricense
versión On-line ISSN 0001-6002versión impresa ISSN 0001-6012
Acta méd. costarric vol.61 no.1 San José ene./mar. 2019
Clinical guideline
Quality indicators in colonoscopy
2Hospital Enrique Baltodano Briceño, Liberia.
7Hospital de la Anexión, Nicoya.
8Hospital San Juan de Dios, San José, Costa Rica.
Colonoscopy is considered as the gold standard study for colorectal cancer. The efficacy of colonoscopy depends on multiple factors, including a correct bowel preparation, careful inspection tecnique, close following of the screening guidelines and adecuate training of the colonoscopist.
The initiative of establishing local quality indicatorsarise from the necessity to arise the quality of the colonospy delivered by Costarican endoscopists. On this document, the Costarican Society of Gastroenterology and Digestive Endoscopy establishes quality indicators for performing safe and effective colonoscopy.
Keywords: colonoscopy; quality indicators; adenoma; early detection of cancer
Colonoscopy is the preferred method to evaluate the colon. If done properly, it is a safe procedure. In addition, it constitutes the gold standard for the detection of colorectal cancer worldwide,1 both for patients with average risk, that is, those without intrinsic factors that promote neoplastic degeneration, as well as for those with increased risk carriers of hereditary polyposis syndromes long-standing inflammatory bowel disease or first-degree heredofamilial history with colorectal cancer.
The effectiveness of colonoscopy depends on multiple factors. The quality of the bowel preparation influences the duration and effectiveness of the procedure.2 Meticulous inspection and adequate time to discharge the patients are factors associated with an increase in the adenoma detection rate.3 A high adenoma detection rate is necessary to consider that a screening colonoscopy is safe, and thus reduce the risk of interval colon cancer.4 Finally, adequate training and operator experience are associated with decreased occurrence of adverse events.5
Recent studies suggest that the effectiveness of colonoscopy for the prevention of proximal colon cancer is less.6 This is probably linked to multiple factors, such as poor preparation and adenomas not detected or incompletely resected. Improving right colon cancer detection should be one of the main goals of quality programs in colonoscopy.
Multiple studies have shown that gastroenterologists are more effective than surgeons in prevention of colorectal cancer by colonoscopy.7-9 This is probably related to a higher percentage of complete studies (cecal intubation) and a better adenoma detection rate in gastroenterologists. It is essential that specialists who perform colonoscopies often determine the quality of their studies.
The quality of medical care can be measured when comparing the performance of an individual against a point of reference. The particular parameter used for comparison is called quality indicator. The Costa Rican Association of Gastroenterology and Digestive Endoscopy has developed this document in order to standardize the quality indicators associated with performing colonoscopy in our country.
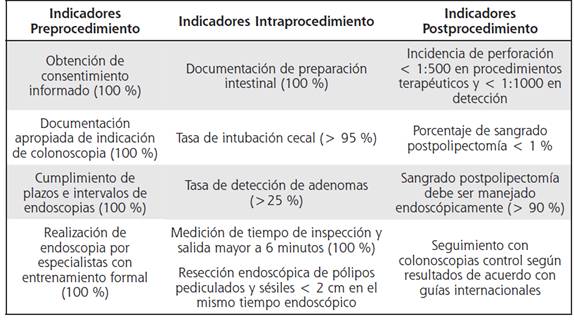
Quality indicators for colonoscopy published by the American Society for Gastrointestinal Endoscopy (ASGE) 10 and the European Society of Gastrointestinal Endoscopy (ESGE) 11, were reviewed and adapted to national reality. The quality indicators were divided into: pre-procedure, intra-procedure and post-procedure.
Pre-procedure quality indicators
The pre-procedure period refers to the contact between the endoscopy team and the patient before the introduction of the endoscope. Pre-procedure quality indicators contemplate:
1. An informed consent was obtained that includes the risks associated with colonoscopy in all patients.
Informed consent must include the risks, benefits and options of colonoscopy. The most frequent risks associated with colonoscopy include bleeding, perforation, infections, events associated with sedation and existence of injuries not observed.
2. The colonoscopy was performed for an appropriate indication and this was documented in the report.
Appropriate indications for performing colonoscopy include:12
a. Significant alterations in an image study
b. Evaluation of low digestive bleeding
c. Evaluation of iron-deficiency anemia
d. Screening for colorectal cancer in patients older than 50 years
e. Follow-up of patients with a history of colorectal cancer
f. Screening for dysplasia in patients with inflammatory bowel disease
g. Studies for chronic diarrhea
The primary objective of this indicator is to reduce the number of procedures performed for an inadequate indication.13
3. The established deadlines must be met according to the guidelines for the post-polypectomy follow-up and after the resection of a cancer, as well as the established 10-year interval in patients with average risk and after a negative colonoscopy with proper preparation.14
For colonoscopy to be cost effective and to minimize its risks, the intervals between procedures must be optimized.
The recommended intervals assume that the colonoscopy was performed with adequate preparation, that the cecum was reached and the exploration was meticulous. The performing a colonoscopy with an interval of less than 10 years in patients with average risk of colorectal cancer is not effective cost and exposes patients to unnecessary risks, which is unjustifiable.
Colonoscopy should be performed exclusively by gastroenterologists or specialists from related branches who have completed a formal training in digestive endoscopy, that includes at least 275 colonoscopies supervised by a duly accredited specialist.9
The specialty of gastroenterology usually offers the more intensive training in performing colonoscopy. Most study programs and international guidelines establish as a requirement at least 275 procedures under supervision before setting the level of competence of the student. Research developed in gastroenterology residents has shown that the cecal intubation rate is not reliable until they have practiced more than 500 colonoscopies.15 These data suggest that the minimum number of colonoscopies to assign competition should be reconsidered.
It has been shown that gastroenterologists detect and resect adenomas more frequently, which suggests a direct relationship between intensive training and these quality indicators. The lower probability of detection and resection of polyps by non-gastroenterologists who perform colonoscopy, reduces the potential benefits of this procedure in the prevention of colorectal cancer.9,16
Intra-procedure quality indicators
The quality of the evaluation of the colon consists in the exploration of the entire colon, including the cecum and the terminal ileum, as well as a detailed mucous inspection. The cecal intubation increases sensitivity and reduces the cost by eliminating the need for complementary radiographic studies, or of repeating the colonoscopy. A detailed and careful inspection of the mucous is essential for the prevention of colorectal cancer. The detection of precancerous lesions is the primary objective of most colonoscopies.
The need to repeat studies, the appearance of adverse events and the surgical management of polyps that can be endoscopically resected, reduce the cost-benefit ratio of the colonoscopy. It is essential that endoscopists evaluate their practices and implement the necessary improvements to reduce the costs associated with colorectal cancer detection and prevention.
The intra-procedural period extends from the time when sedation begins until the endoscope is removed. It includes all the technical aspects and therapeutic maneuvers of the process.
Intra-procedure quality indicators include the following:
1. The quality of the intestinal preparation must be documented for colonoscopy in all procedures and it should be appropriate, in such a way as to allow the use of the follow-up intervals recommended in the detection guides.
The quality of the preparation is based on the ability of visualizing adequately the mucous during colonoscopy. The endoscopist must document the quality of the preparation in each procedure.17 Non-standardized terms should be avoided to describe the intestinal preparation. The use of the Boston scale is recommended, internationally validated, to describe the preparation of the colonoscopy.18 According to international guidelines, it is defined as a proper intestinal preparation with a scale of Boston ≥ 6.11 If the colonic preparation is inadequate and the procedure is performed to detect colorectal cáncer or post-polypectomy follow-up, the colonoscopy should be repeated in a span of one year or less.
The presence of poor intestinal preparation prolongs the cecal intubation and revision times during the exit, in addition to significantly reducing the detection of small and large polyps.19
It is recommended that the percentage of studies that are done with inadequate preparation is less than 15%. Multiple clinical studies suggest that the use of preparation in divided doses (split dose) improves adequate intestinal preparation rates. The most relevant factor for a proper preparation is the interval between the end of the intake of the preparation and the beginning of the procedure.20 The quality of intestinal preparation decreases with increase in the interval between the end of the intake and the start of the study. This happens especially in the right colon. The use of intestinal preparation in divided doses in all patients who are going to undergo colonoscopy, ending the last shot 2 hours before the study.
According to the fasting guidelines of the Society American Anesthesiology, patients should take nothing orally for 2 hours after ingestion of clear liquids.21 Patients should be instructed to start the second dose of the preparation 4 to 5 hours before the scheduled time for the procedure and so that they must finish it 2 hours before this.
2. The frequency with which the cecum is intubated should be greater than 95% and must be documented photographically.
Cecal intubation is defined as the advance of the tip of the endoscope to a site proximal to the ileocecal valve, in such a way that all the cecum can be evaluated. The need to evaluate completely the cecum is that a significant percentage of colorectal neoplasms are located in the right colon. Low rates of cecal intubation have been associated with a higher frequency of interval proximal colon cancer.22 Cecal intubation should be documented by photographic capture of the ileocecal valve and the appendicular orifice. Experienced colonoscopists are in the ability to identify cecal intubation with 100% certainty.
An effective colonoscopist must be able to intubate the cecum in 95% of screening colonoscopies.23
3. The frequency with which adenomas are detected in asymptomatic individuals with average risk of colorectal cáncer should be greater than 25%.
There is evidence documenting the omission in the detection of adenomas by colonoscopists when colonoscopies are performed in tandem.24 In addition, it has been shown that colonoscopy fails to prevent all colorectal cancers in cohorts followed for more than 3 years, with the majority of cancers attributable to unidentified lesions and incomplete resections, as well as variations in tumor growth patterns. 25
In addition, it has been demonstrated a marked variation in the detection of adenomas by colonoscopists within the same clinical practice.26,27 This variation was the sustenance for the creation of objectives for the adenomas detection rate (ADR) .28
ADR is defined as the percentage of patients over 50 years of age in which one or more adenomas are detected during his first screening colonoscopy. Studies have documented that patients who are done screening colonoscopy by endoscopists with ADR less than 20% have a risk ratio 10 times higher to develop colon cancer, compared to those who have their colonoscopy with endoscopists with ADR greater than 20%.4
Recent studies suggest that some colonoscopists can achieve ADR greater than 40% .26 The higher than 30% ADR are associated with a reduction in the risk of developing colon cancer, both proximal and distal, both in men as in women.29
Based on this evidence, it has been proposed a minimum target of 25% as ADR in elderly patients of 50 years undergoing screening colonoscopy.
All colonoscopists must have a record of their TDR and those with an ADR lower than 25% should take concrete measures to improve their performance.
The ADR is the main indicator of quality in colonoscopy. There is a close correlation between the ADR and the recommended intervals for follow-up and screening. Colonoscopists with elevated ADR find and dry more precancerous lesions and they bring their patients back in shorter intervals, because the recommended follow-up intervals are short after the finding of precancerous lesions. On the contrary, colonoscopists with low ADR fail to identify patients with precancerous or multiple lesions and, therefore, recommend inappropriately long intervals between studies. This interaction makes it essential to know the ADR of each endoscopist to, in this way, ensure adequate protection of the patient.30
4. Exit inspection time during colonoscopy must be measured and, on average, it must be greater than 6 minutes.
Studies have shown an increase in the detection of neoplastic lesions, when the inspection time during the exit is greater than 6 minutes. The main utility of increasing the time of departure is to increase the ADR in colonoscopists with suboptimal performance.31
The detailed exploration of the colon requires time and this is the reason why there is a close relationship between time of inspection during the exit of the colonoscopy and the ADR.
5. Endoscopic resection of pedunculated polyps and sessile of less than 2 cm, should be done during the same endoscopic procedure.
Deferring the resection of small colonic polyps identified during a routine colonoscopy, increases costs and decreases the cost-benefit ratio of the procedure, which is unacceptable. The vast majority of polyps smaller than 2 cm are endoscopically resectable and should not be referred for surgical resection.
In some cases, certain polyps may be difficult to position for an adequate polypectomy, and it is advisable to send it to a referral center.32 Endoscopic resection of the vast majority of polypoid lesions is safe and more cost effective than surgical resection.33 If it is anticipated that the lesion will be referred to be resected by another endoscopist, the taking of multiple biopsies or a partial polypectomy with loop should be avoided, in order to prevent the development of fibrosis that limits a later resection.
The lesions sent for surgical resection should be marked with china ink in 3 or 4 quadrants and in this way ensure the resection of the correct segment.
Post-procedure quality indicators
The post-procedure period extends from the time the endoscope is removed until subsequent follow-up. The care after the procedure includes: giving relevant instructions to the patient, recognition of the adverse events, assessment of histopathological findings and determination of the degree of patient satisfaction. The post-procedure quality indicators include:
1. Incidence of perforation less than 1 in 500 therapeutic procedures and 1 in every 1000 detection colonoscopies of and a percentage of post-polypectomy bleeding less than 1%. The drilling is considered as the event most serious adverse event associated with colonoscopy. About 5% of perforations during colonoscopy are fatal.34
Perforation rates greater than 1 in every 500 patients, should encourage a study to determine if there are any inappropriate practices. Among the suggested practices to reduce the risk of drilling, include: do not push against of a fixed resistance, remove the loops as soon as possible, use a pediatric colonoscope in cases of severe diverticular illness and use carbon dioxide instead of air for insufflation.
It is necessary to avoid the use of electrocautery in resection of small polyps and use submucosal injection prior to electrocautery resection of large sessile lesions.35
Intraprocedural perforations that occur can be resolved by closing with hemostatic clips.36
Bleeding is the most frequent adverse event after a polypectomy. It can be early or late. The different series suggest that postpolypectomy bleeding should be less to 1% .37 The risk of bleeding increases according to the size of the polyp, proximal location and with the use of anticoagulation or platelet antiaggregants.38
2. Post-polypectomy bleeding should be managed endoscopically successful in more than 90% of cases. The bleeding site should be treated with injection combined with the placement of hemoclips or cauterisation.39
3. A recommendation for a control colonoscopy should be provided, according to the monitoring guides after the review of the histological findings.
Current guidelines recommend screening by colonoscopy every 10 years in the general population, every 5 years in patients with less than 2 small tubular adenomas and every 3 years in patients with more than 3 tubular adenomas, in villous adenomas, in those greater than 1 cm or in those associated with high grade dysplasia.40 Overuse of colonoscopy should be avoided for screening, since this practice is not cost effective and exposes patients to unnecessary adverse risks.
Correction of poor performance
The primary purpose of measuring the indicators of quality is to improve patient care by identifying colonoscopists who have poor performance to retrain them properly. When an endoscopist has an ADR lower than recommended, you must make the necessary adjustments and demonstrate improvement within a reasonable time. It has been evidenced that the most effective interventions related with improving ADR, include education linked to appearance endoscopy of precancerous lesions and instruction about the proper inspection technique during the release phase.41
Colonoscopy should be avoided by endoscopists who do not reach the minimum levels of ADR after a period of retraining.
The experience is conclusive that low levels of ADR put in the patients in risk.4
Conclusions
For colonoscopy, the priority quality indicators are an ADR greater than 25%, a cecal intubation greater than 95% and the correct use of recommended intervals for screening and followup of colorectal cancer. These 3 indicators are associated with highly relevant clinical outcomes and, therefore, they must be strictly monitored.
The realization of high quality colonoscopy constitutes the fundamental role of the colonoscopist in the multidisciplinary effort to reduce the incidence and mortality of colorectal cancer.
REFERENCES
1. Centers for Disease Control and Prevention. Vital signs: colorectal cancer screening test used. United States, 2012. MMWR Morb Mortal Wkly Rep 2013;62:881-888. [ Links ]
2. Harewood GC, Sharma VK, de Garmo P. Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc 2003;58:76-79. [ Links ]
3. Lee RH, Tang RS, Muthusamy VR, Ho SB, Shah NK, Wetzel L, et al. Quality of colonoscopy withdrawal technique and variability in adenoma detection rates (with videos). Gastrointest Endosc 2011;74:128-134. [ Links ]
4. Kaminski MF, Regula J, Kraszewska E, Polkowski M, Wojciechowska U, Didkowska J, et al. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med 2010;362:1795-1803. [ Links ]
5. Chukmaitov A, Bradley CJ, Dahman B, Umaporn S, Warren J, Klabunde C. Association of polypectomy techniques, endoscopist volume, and facility type with colonoscopy complications. Gastrointest Endosc 2013;77:436-446. [ Links ]
6. Singh H, Nugent Z, Demers AA, Kliewer EV, Mahmud SM, Bernstein CN. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology 2010;139:1128-37. [ Links ]
7. Rabeneck L, Paszat LF, Saskin R. Endoscopist specialty is associated with incident colorectal cancer after a negative colonoscopy. Clin Gastroenterol Hepatol 2010;8:275-9. [ Links ]
8. Baxter NN, Warren JL, Barrett MJ, Stukel TA, Doria-Rose VP. Association between colonoscopy and colorectal cancer mortality in a US cohort according to site of cancer and colonoscopist specialty. J Clin Oncol 2012;30: 2664-9. [ Links ]
9. Ko CW, Dominitz JA, Green P, Kreuter W, Baldwin LM. Specialty differences in polyp detection, removal, and biopsy during colonoscopy. Am J Med 2010;123:528-35. [ Links ]
10. Rex D, Schoenfeld P, Cohen J. Pike IM, Adler DG, Fennerty MB. et al. Quality indicators for colonoscopy. Gastrointestinal Endoscopy, Volume 81, Issue 1,31 -53. [ Links ]
11. Kamisky, MF. Thomas-Gibson S. Bugajski M, Bretthauer M, Rees CJ, Dekker E. et al. Quality in screening colonoscopy. Endoscopy. 2017 Apr;49(4):378-397. [ Links ]
12. Early DS, Ben-Menachem T, Decker GA, Evans JA, Fanelli RD, Fisher DA, et al. Appropriate use of GI endoscopy. Gastroinest Endosc. 2012;75:1127-31. [ Links ]
13. Vader JP, Pache I, Froehlich F, Burnand B, Schneider C, Dubois RW, et al. Overuse and underuse of colonoscopy in a European primary care setting. Gastrointest Endosc 2000;52: 593-9. [ Links ]
14. Lieberman DA, Rex DK, Winawer SJ, Giardiello FM, Johnson DA, Levin TR. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology 2012;143:844-57. [ Links ]
15. Spier BJ, Benson M, Pfau PR, Nelligan G, Lucey MR, Gaumnitz EA. Colonoscopy training in gastroenterology fellowships: determining competence. Gastrointest Endosc.2010. 71(2):319-24. [ Links ]
16. Rex DK, Rahmani EY, Haseman JH, Lemmel GT, Kaster S, Buckley JS. Relative sensitivity of colonoscopy and barium enema for detection of colorectal cancer in clinical practice. Gastroenterology. 1997; 29: 575-79. [ Links ]
17. Lieberman D, Nadel M, Smith RA, Atkin W, Duggirala SB, Fletcher R, et al. Standardized colonoscopy reporting and data system: report of the Quality Assurance Task Group of the National Colorectal Cancer Roundtable. Gastrointest Endosc 2007;65:757-66. [ Links ]
18. Calderwood AH, Jacobson BC. Comprehensive validation of the Boston Bowel Preparation Scale. Gastrointest Endosc 2010;72:686-92. [ Links ]
19. Lebwohl B, Kastrinos F, Glick M, Rosenbaum AJ, Wang T, Neugut AI. The impact of suboptimal bowel preparation on adenoma miss rates and the factors associated with early repeat colonoscopy. Gastrointest Endosc 2011;73: 1207- 14. [ Links ]
20. Kilgore TW, Abdinoor AA, Szary NM, Schowengerdt SW, Yust JB, Choudhary A, et al. Bowel preparation with split-dose polyethylene glycol before colonoscopy: a metaanalysis of randomized controlled trials. Gastrointest Endosc 2011;73:1240-5. [ Links ]
21. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Committee on Standards and Practice Parameters. Anesthesiology 2011;114:495-511. [ Links ]
22. Baxter N, Sutradhar R, Forbes DD, Paszat LF, Saskin R, Rabeneck L. Analysis of administrative data finds endoscopist quality measures associated with post-colonoscopy colorectal cancer. Gastroenterology 2011;140:65-72. [ Links ]
23. Rathgaber SW, Wick TM. Colonoscopy completion and complication rates in a community gastroenterology practice. Gastrointest Endosc 2006;64:556-62. [ Links ]
24. van Rijn JC, Reitsma JB, Stoker J, Bossuyt PM, van Deventer SJ, Dekker E. Polyp miss rate determined by tandem colonoscopy: a systematic review. Am J Gastroenterol 2006;101:343-50. [ Links ]
25. Pohl H, Robertson DJ. Colorectal cancers detected after colonoscopy frequently result from missed lesions. Clin Gastroenterol Hepatol 2010;8:858-64. [ Links ]
26. Chen SC, Rex DK. Endoscopist can be more powerful than age and male gender in predicting adenoma detection at colonoscopy. Am J Gastroenterol 2007;102:856-61. [ Links ]
27. Shaukat A, Oancea C, Bond JH, Church TR, Allen JI. Variation in detection of adenomas and polyps by colonoscopy and change over time with a performance improvement program. Clin Gastroenterol Hepatol 2009;7: 1335-40. [ Links ]
28. Rex DK, Bond JH, Winawer S, Levin TR, Burt RW, Johnson DA, et al. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U.S. Multi- Society Task Force on Colorectal Cancer. Am J Gastroenterol 2002;97: 1296- 308. [ Links ]
29. Corley D, Jensen CD, Marks AR, Zhao WK, Lee JK, Doubeni CA, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 2014;370: 1298-306. [ Links ]
30. Hewett DG, Rex DK. Improving colonoscopy quality through healthcare payment reform. Am J Gastroenterol 2010;105:1925-33. [ Links ]
31. Barclay RL, Vicari JJ, Greenlaw RL. Effect of a time-dependent colonoscopic withdrawal protocol on adenoma detection during screening colonoscopy. Clin Gastroenterol Hepatol 2008;6:1091-8. [ Links ]
32. Buchner AM, Guarner-Argente C, Ginsberg GG. Outcomes of EMR of defiant colorectal lesions directed to an endoscopy referral center. Gastrointest Endosc 2012;76:255-63. [ Links ]
33. Onken JE, Friedman JY, Subramanian S, et al. Treatment patterns and costs associated with sessile colorectal polyps. Am J Gastroenterol 2002;97:2896- 901. [ Links ]
34. Anderson ML, Pasha TM, Leighton JA. Endoscopic perforation of the colon: lessons from a 10-year study. Am J Gastroenterol 2000;95: 3418-22. [ Links ]
35. Paspatis GA, Tribonias G, Konstantinidis K, Theodoropoulou A, Vardas E, Voudoukis E, et al. A prospective randomized comparison of cold vs hot snare polypectomy in the occurrence of postpolypectomy bleeding in small colonic polyps. Colorectal Dis 2011;13:e345-8. [ Links ]
36. Cho SB, Lee WS, Joo YE, Kim HR, Park SW, Park CH, et al. Therapeutic options for iatrogenic colon perforation: feasibility of endoscopic clip closure and predictors of the need for early surgery. Surg Endosc 2012;26:473-9. [ Links ]
37. Sorbi D, Norton I, Conio M, Balm R, Zinsmeister A, Gostout CJ. Postpolypectomy lower GI bleeding: descriptive analysis. Gastrointest Endosc 2000;51:690-6. [ Links ]
38. Singh M, Mehta N, Murthy UK, Kaul V, Arif A, Newman Nl. Postpolypectomy bleeding in patients undergoing colonoscopy on uninterrupted clopidogrel therapy. Gastrointest Endosc 2010;71:998-1005. [ Links ]
39. Rex DK, Lewis BS, Waye JD. Colonoscopy and endoscopic therapy for delayed post-polypectomy hemorrhage. Gastrointest Endosc 1992;38: 127-9. [ Links ]
40. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2008;149: 627-37. [ Links ]
41. Coe S, Crook JE, Diehl NN, Wallace MB. An endoscopic quality improvement program (EQUIP) improves detection of colorectal adenomas. Am J Gastroenterol. In press. [ Links ]
1Support sources: We did not have sources of support for the execution of this document and none of the authors have conflicts of interest.
Received: May 24, 2018; Accepted: August 23, 2018











 texto en
texto en