Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Médica Costarricense
versión On-line ISSN 0001-6002versión impresa ISSN 0001-6012
Acta méd. costarric vol.58 no.4 San José oct./dic. 2016
Articles
Endoscopic injection for the correction of Vesicoureteral reflux
1Servicio de Urología, Hospital Nacional de Niños.
2Servicio de Urología, Hospital San Juan de Dios, Caja Costarricense de Seguro Social. Universidad de Costa Rica.
Vesicoureteral Reflux (VUR) is one of the most important causes of pediatric nephropathy in many countries.1,2 Understanding the pathophysiology and course of the disease has led to the conservative management of most patients. However, there is a group of patients with recurrent urinary tract infections, febrile, in spite of prophylactic antibiotics, whose probability of spontaneous resolution is unlikely and have scarred kidneys, which require surgical treatment.3,4 Surgical procedures include laparoscopic and open ureteral reimplantation, and endoscopic subureteral injection.5
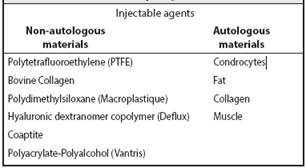
Endoscopic subcutaneous injection with STNG technique is performed under general anesthesia, cystoscopy is performed, a 3-French ureteral catheter is inserted to lift the anterior wall of the ureter, the material is injected through a special syringe under direct vision, with the bezel facing up at 6 o’clock clockwise, as shown in Figure 1; it is then introduced into the mucosa 2-3 mm distal to the uretero-vesical junction and is advanced in the submucosal plane by 4-5 mm towards the lumen. The needle is inserted at the submucosal level in front of the refluxing ureter and advanced to an intraluminal position. Sufficient Deflux is injected to create the bulging image (volcano shape) that converts the ureteral orifice into a crescent-shape (Figure 2), which is key to the procedure.6,7,8 Materials that can be used for injection are listed in Table 1.
Ultrasound and voiding cystourethrogram (VCUG) are followed up after any antireflux procedure at 3 months after surgery.9 Reflux degree is the greatest predictor for VUR resolution: the higher the grade, the lower the probability of spontaneous resolution. Endoscopic treatment is preferred for low-grade reflux, while open surgery is best for high-grade reflux. 10
Open surgery has a reported success rate of 100%, and approximately 89% for endoscopic injection. Although it has a lower success rate, endoscopic treatment was preferred because of its low morbidity and better postoperative recovery.
Even without resolution after endoscopic injection, a high rate of VUR grade decrease has been reported. These cases, or even those without changes, could receive a new endoscopic attempt, and when a new therapeutic failure occurs, the open approach can be used.11-19
Methods
A retrospective observational study was carried out, reviewing records of patients diagnosed with vesicoureteral reflux, and submitted to endoscopic injection surgery between December 2011 and February 2015, by the Pediatric Urology Department of the Hospital Nacional de Niños (National Children’s Hospital) “Dr. Carlos Sáenz Herrera “.
Patients with a diagnosis of primary or secondary VUR were included, in whom it was possible to correct the secondary cause, although they persisted with VUR. Patients with persistent voiding dysfunction and those without VCUG after anti-VUR endoscopic injection were excluded.
In each case, the patient’s epidemiology (gender, age of diagnosis, patient’s clinical condition, surgical indication, associated pathologies) and pre-surgical studies (urinary tract ultrasound, VCUG, DMSA), surgical indication, the substance used for endoscopic injection, and post-surgical studies (ultrasound of the urinary tract, VCUG and VCUG by radionuclides).
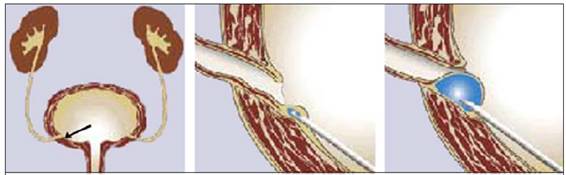
Figure 1: Original endoscopic injection technique. The arrow shows the injection site related to the ureteral orifice (middle image)
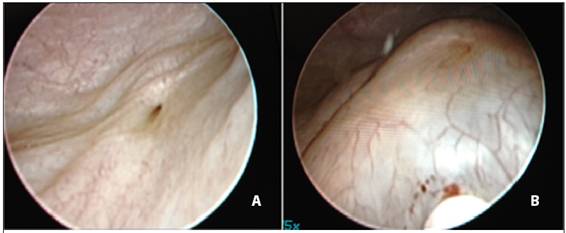
Figure 2: A) Appearance of a refluxing ureter B) After endoscopic injection, a bulge image is seen (mount shape).
Substances used in this study for endoscopic anti-reflux injection are: Macroplastique and Vantris.
Data was tabulated and graphs were made in the Microsoft Office Excel 2013 software.
Results
A total of 33 cases evaluated at the Pediatric Urology Service of the Hospital Nacional de Niños with a diagnosis of VUR, according to clinical and test results, were submitted to endoscopic anti-VUR injection between December 2011 and February 2015.
Out of the analyzed population, 66.6% were girls and 33.3% were boys. There was no mean age of VUR diagnosis. In patients with VUR, the degree of reflux was classified on each affected side, with a total of 42.4% of patients with bilateral VUR (14 cases), 36.36% (12 Cases) with left VUR, and 21.21% (7 cases) with a right side affected; accounting for a total of 47 ureteral units evaluated.
The most frequently diagnosed reflux degree was grade II, in 44.7%, followed by grade III in 38.3% of cases. The most frequent reflux type was of primary origin, in 82% of patients.
The most frequent symptoms were: symptomatic urinary tract infection (82%), enuresis (3%), macroscopic hematuria (3%), impaired renal function (6%) and only 6% of the patients were asymptomatic (incidental diagnosis due to ureteral dilatation).
VUR was associated with detrusor sphincter dyssynergia in 12% of cases, duplicated collecting system in 9%, polycystic kidney in 6%, paraureteral diverticulum, renal agenesis and hypospadias in 3% of cases.
The preoperative studies performed in all cases were: urinary tract ultrasound, VCUG and DMSA. The most frequent alteration was the loss of the cortical-medullary ratio in 24% of the cases, followed by the ureteropyelocalicial dilatation of the affected system in 21%, multicystic kidney in 6%, renal ectopia, lithiasis and renal agenesia in only 3% of the cases. Preoperative DMSA showed that 57.6% of the patients had renal scars.
The most frequent surgical indication was recurring urinary tract infection (39.4%); followed by persistent VUR (24.2%).
Vantris was used in 63.6% of patients and Macroplastique in 27.4%. Subureteral STING technique was the most used, in 93.9%, and only 2 cases (6.1%), performed the intraureteral technique.
Most patients presented resolved their vesicoureteral reflux after surgery (88%); less patients persisted with a lower degree of reflux than at the time of diagnosis (12%); all were again submitted endoscopic anti-reflux injection, and only one patient persisted with VUR, however it was a low grade VUR with no associated symptoms, so it is being managed conservatively.
One patient had a surgical complication, with a false urethral passage, which was managed conservatively, with excellent evolution.
Discussion
In the study population, VUR was more frequent in girls, there were patients from all provinces of the country, and the most frequent degree of VUR in patients undergoing endoscopic anti-reflux injection was grade II, followed by grade III. The sample has an important heterogeneity regarding age, ranging from 6 months to 8 years old at the time of diagnosis, and an average of 4 years old.
The average time between diagnosis and surgery was 2 and a half years, which is short considering that it includes an observation period before surgical management is indicated. As for epidemiology, data resembles that found in the literature: girls account for most diagnosis and the most common presenting symptom is urinary tract infection.
Changes in DMSA were found in 57.57%, which is associated, according to the literature, with late diagnosis of vesicoureteral reflux, and inadequate management of urinary tract infections. Preoperative studies were those used in the literature: urinary tract ultrasound, VCUG and DMSA. The most frequent surgical indication is persistent urinary tract infection, and the persistence of reflux beyond 5 years old, which is the time when anatomic growth and ureterovesical junction remodeling occurs. These data agree with those described in the literature.
The majority of patients had a diagnosis of grade II and III VUR, and reported a higher rate of resolution by endoscopic anti-reflux injection; only four cases had persistent vesicoureteral reflux following anti-reflux injection, but with a lesser degree than at baseline; three cases had grade III VUR and one had grade IV; all four cases were re-injected with endoscopic anti-reflux therapy, and three resolved their VUR, while only one persisted with grade I asymptomatic VUR, so it is being given a conservative management. There are no reports of patients with grade V VUR treated with endoscopic anti-reflux injection.
Only one patient presented a complication related to the surgical procedure, and was a false urethral passage, which was managed conservatively, without major problems. According to the literature, there is a low incidence of complications with endoscopic anti-reflux injection, with injected ureterovesical junction stenosis being the most common.
The success rate of endoscopic injection in the analyzed patients was 88%. Further prospective studies are required to assess the long-term outcome of these patients, since even in the literature the latency of the injected material for this surgery has not been defined.
The correction of vesicoureteral reflux by endoscopic injection with Macroplastique and Vantris is safe, effective and minimally invasive. Early correction of VUR protects children with and without renal scars, and decreases the prolonged use of antibiotic prophylaxis. Endoscopic subureteral injection with Vantris and Macroplastique is an effective method for short-term RVU correction; the success rate is not influenced by the degree of reflux and the configuration of the ureteral orifice. Long-term results are needed from patients with VUR treated with endoscopic anti-reflux injection to assess the rate of VUR recurrence.
Authors affiliations:
1 Urology Department, Hospital Nacional de Niños.
2 Urology Department, Hospital San Juan de Dios, Caja Costarricense de Seguro Social. Universidad de Costa Rica.
Abbreviations: VUR, Vesicoureteral Reflux; VCUG, voiding cystourethrogram; US, ultrasound; DMSA, Dimercaptosuccinic Acid Gammagraphy.
francor23@gmail.com
Referencias
1. Chertin B, Arafeh WA, Zeldin A, Kocherov S. Preliminary data on endoscopic treatment of vesicoureteric reflux with polyacrylate polyalcohol copolymer (Vantris): Surgical outcome following single injection. J Pediatr Urol. 2011;7:654-7. [ Links ]
2. Molitierno J, Scherz H, Kirsch A. Endoscopic treatment of vesicoureteral reflux using dextranomer hyaluronic acid copolymer. J Pediatr Urol 2008;4:221. [ Links ]
3. Ormaechea M, Ruiz E, Denes E, Gimenez F, Dénes FT, Moldes J, et al. New tissue bulking agent (polyacrylate polyalcohol) for treating vesicoureteral reflux: Preliminary results in children. J Urol. 2010; 183: 714-7. [ Links ]
4. Farshid A, Amir A, Mahtab Z, Farhad T, et al. The influence of ureteral orifice configuration on the success rate of endoscopic treatment of vesicoureteral reflux. Advanced Biomedical Research. 2013;2:1-8. [ Links ]
5. De Badiola F, Soria R, et al. Results of treatment of grades IV and V vesicoureteral reflux with endoscopic injection of polyacrylate polyalcohol copolymer. Pediatric Urology. 2013; 1:1-4. [ Links ]
6. Kocherov S, Ulman I, et al. Multicenter Survey of Endoscopic Treatment of Vesicoureteral Reflux Using Polyacrylate Polyalcohol Bulking Copolymer (Vantris); Urology. 2014;84:689-693. [ Links ]
7. Tamer Helmy, Doaa Sharaf, Ahmed Abdel Halim, Ashraf Hafez, and Mohammed Dawaba. Can Distal Ureteral Diameter Predict Reflux Resolution After Endoscopic Injection?; Urology. 2015; 85: 896-899. [ Links ]
8. Sean T. Watters, Jennifer Sung, Steven J. Skoog; Endoscopic treatment for vesicoureteral reflux: How important is technique? Journal of Pediatric Urology. 2013; 9:1192-1197. [ Links ]
9. Belman B. Vesicoureteral reflux. Pediatric Clin North Am 1997;44:1171. [ Links ]
10. Rodríguez J. Reflujo vesicoureteral. Revista Chilena Pediatría. 2000; 7:441-446. [ Links ]
11. Bailey R. Vesicoureteric reflux in healthy infants and children. In: Hodson J, Kincaid-Smith P, editors. Reflux nephropathy. New York: Masson; 1979; 59-61. [ Links ]
12. Sargent MA. What is the normal prevalence of vesicoureteral reflux? Pediatr Radiol. 2000; 30:587-93. [ Links ]
13. Rushton HG. The evaluation of acute pyelonephritis and renal scarring with technetium 99mdimercaptosuccinic acid renal scintigraphy: evolving concepts and future directions. Pediatr Nephrol. 1997;11:108-20. [ Links ]
14. Chand DH, Rhoades T, Poe SA, Kraus S, Strife CF; Incidence and severity of vesicoureteral reflux in children related to age, gender, race and diagnosis. J Urol. 2003; 170: 1548-50. [ Links ]
15. Horowitz M, Gershbein AB, Glassberg KI; Vesicoureteral reflux in infants with prenatal hydronephrosis confirmed at birth: racial differences. J Urol. 1999; 161: 248-50. [ Links ]
16. Pinto KJ; Vesicoureteral reflux in the Hispanic child with urinary tract infection. J Urol. 2004; 171: 1266-7. [ Links ]
17. Garin EH, Campos A, Homsy Y; Primary vesicoureteral reflux: review of current concepts. Pediatr Nephrol. 1998; 12: 249-56. [ Links ]
18. Campbell-Walsh. Urología. IX Edición. Capítulo 117. Páginas 3423-3481. Elsevier Argentina, S.A. Buenos Aires, Argentina 2008. [ Links ]
19. Matthew H. Hayn, Marc C. Smaldone, Michael C. Ost, Steven G. Docimo, Minimally Invasive Treatment of Vesicoureteral Reflux; Urol Clin N Am 2008; 35: 477-488. [ Links ]











 texto en
texto en