Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Médica Costarricense
versión On-line ISSN 0001-6002versión impresa ISSN 0001-6012
Acta méd. costarric vol.58 no.2 San José abr./jun. 2016
Articles
Mucocutaneous leishmaniasis treated with miltefosine
1Servicio de Dermatología del Hospital de Grecia, Caja Costarricense de Seguro Social.
2Servicio de Otorrinolaringología del Hospital “Dr. Rafael Ángel Calderón Guardia”, Caja Costarricense de Seguro Social fulincr@yahoo.com
Mucocutaneous leishmaniasis is a zoonotic disease transmitted by the bite of a vector or a female mosquito of three frecuente types: Phlebotomus in the Old World, and Lutzomya and Psychodopygus in the New World.1,2 Within the mosquito it takes the form of a promastigote and when its inoculated in humans in the cells of the reticuloendothelial system, that of the amastigote. New World leishmaniasis is caused by Leishmania b. braziliensis and Leishmania b. panamensis.
Man originally does not belong to the transmission cycle of this parasite, but the emergence of forest habitat and its ecosystem, has turned the human being into an accidental host.1 Globalization, increased foreign visitors to national forests, the increase in population with the development and expansion of the economy, makes man invade more the forests where the vectors of leishmania live.3 Traditional treatment of choice has been the use of pentavalent antimonials, as well as meglumine antimoniate (Glucantime®) and sodium stibogluconate (Pentostam®), but its side effects, such as cardiotoxicity, make some people with underlying heart disease are not candidates for the use of this treatment and, for that reason, seek the use of new therapeutic options.
Case Presentation
Male patient aged 78, resident of Naranjo of Alajuela, farmer, married and Catholic, with a family history of arterial hypertension and gastric cancer of the mother, no medical or surgical significant history and known medical history of hypertension, diabetes mellitus type 2, chronic atrial fibrillation with appropriate ventricular response, anticoagulated and a history of a cerebrovascular ischemic event suffered 4 years ago; current treatment with enalapril, glibenclamide, digoxin and warfarin.
It was presented to the consultation of Otolaryngology (ORL) of the Grecia Hospital, with a superficial ulceration with violaceous raised edges and the bottom had an ulcer with hematic scabs on the right ear helix; a endoscopy was performed in which multiple ulcerations were observed in the nasal mucosa with deviation of the nasal septum and a presbycusis. It was decided to send a smear and culture of Leishmania of the dermatosis, and with a reference to the Department of Dermatology of the same center. As seen by the dermatologist of the Hospital it was determined to perform an excisional biopsy for the hematoxylin and eosin staining, in order to rule out possible tumor process versus infectious process. Time thereafter the result of the biopsy came out with the diagnosis of unspecified infectious granulomatous dermatitis. The patient was questioned thoroughly, who reveals that 1 year before the onset of symptoms he had been bitten by a mosquito in San Carlos, so with that history and the histopathological report, they continued with the shipment and coordination of a reaction of Montenegro to the Mexico Hospital, which was reported to be positive. With this evidence a biopsy was performed by the ORL service in the nasal mucosa, to make a polymerase chain reaction (PCR, for its acronym in English) by Leishmania, which was performed at the National Children’s Hospital, and it was reported positive for Leishmania panamensis.
Discussion
Mucocutaneous leishmaniasis in the new world is a disease that can be caused by: Leishmania (V) braziliensis, Leishmania (V) panamensis, Leishmania amazonensis, Leishmania (V) guyanensis,4 whose transmission is carried out by the mosquito of the genus Phlebotomus in the Old World and Lutzomyia or Psychodopygus in the New.4 Inside the mosquito the protozoan is in the form of promastigote while its being inoculated into the skin, then its phagocytosed by the macrophages and becomes amastigote.3 The skin lesions are observed clinically as nodules, then ulcerate and form plaques with a necrotic crateriform ulcer with a necrotic bottom and a violet edge, often covered with adherent scabs,4 as in the case of this patient, the lesion was found in the right ear helix, site of inoculation by the transmitter mosquito. The spread of the parasite of the Leishmania of the new world, of the primary skin lesion to the mucosa, can occur in months or years after the appearance of the primary skin lesion,3 as reported in this patient, it occurs in a period of 8 months. The vascular anatomy of the nasal cavities and specifically the nasal septum, favored the parasite reservoir -in this case the Leishmania-; the deposit of the parasites interfered with the vascular supply of the cartilaginous structures, which led to a deterioration of the compromised structure and caused primary ulcerative lesions, and secondly, scarred outgrowing lesions; this process was the result of a long-term outcome of a cutaneous leishmaniasis not treated5 (Figure 1).
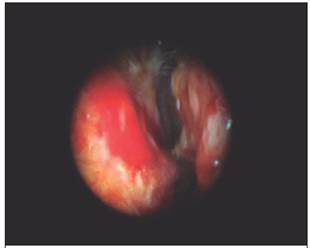
Figure 1 Nasal endoscopy performed in the ORL Department of the Grecia Hospital, which shows a red nasal mucosa with multiple white superficial ulcerations.
Among the differential diagnosis of the cutaneous leishmaniasis are: sporotrichosis, typical and atypical mycobacterial infection, ulcers by bacterial and traumatic infections, basal cell carcinoma, squamous cell or melanoma; as to the condition of the nasal mucosa it can be differentiated with rhinoscleroma, lepromatous leprosy, paracoccidioidomycosis, Wegener granulomatosis, nasopharyngeal carcinoma and lymphomas.6,4 The diagnosis was based on the epidemiological history, smear and culture of mucocutaneous lesions in the middle of Novy-MacNeal-Nicolle (NMN) or Schneider’s, with the demonstration of the parasite whose sensitivity is very low (50%), this was demonstrated that in both the result was negative; Leishmania, which is a delayed hypersensitivity reaction (Montenegro reaction) was positive in the patient, being not allergic, and the biopsy for histology of a skin sample for the hematoxylin and eosin staining, with giant cells and lymphohistiocytic cells where consistent with the sample sent, although the finding was negative for intracellular amastigotes (Leishman-donovan body) or extracellular; this diagnosis factor will always depend on the experience and ability to recognize the parasite by the pathologist; molecular detection technique such as PCR by Leishmania, it offers a greater specificity and sensitivity to the above methods,4,7-9 it was positive for Leishmania panamensis in this case, affirming what was described in the world literature.
The treatment of choice are pentavalentes antimonials, such as antimoniate N-methylglucamine (Glucantime®) and sodium stibogluconate (Pentostam®), whose side effects include: musculoskelatal pain, nausea, vomiting, diarrhea and abdominal pain, headache, fever, rash, erythema and urticaria. This was not used in the patient due to associated underlying treatment, since of in an anticoagulated, the intramuscular injection is associated with bruises and mild to moderate pain at the site of application,10 and it should be noted that the institution provides only the Glucantime® of intramuscular application. Reactions in cases of intravenous injections are: phlebitis, thrombophlebitis and edema in the catheter insertion sites; also it has been reported mild to moderate increase of liver and pancreatic enzymes.10 Whenever you want to apply the pentavalentes antimonials it should be considered the patient comorbidities, since the electrocardiographic abnormalities include prolongation of the QT interval and alterations in ventricular repolarization, with involvement of the T wave and S-T segment on the electrocardiogram,10,11 and to avoid any complications due to medication, because of the underlying chronic atrial fibrillation that the patient has, its use was avoided. Another therapeutic option such as pentamidine, which interferes with DNA synthesis protozoan, whose side effects are usually: hypoglycemia, hypotension, headache, increased blood urea nitrogen and creatinine, diabetes, pancreatitis, leukopenia with abnormal T wave and ST segment on the electrocardiogram,3 for obvious reasons it is not considered.
The use of amphotericin B, which in many industrialized countries is considered as second-line treatment, acts on ergosterol, which is a steroid present in the Leishmania, causing an increase in the permeability of the cell membrane, producing an entry of ions into parasite and resulting in death.3 Its nephrotoxicity and side effects make this a drug for hospital use;3,2 when analyzing the patient’s case, his advanced age and being away from family, it was determined that the possibility of depressive symptoms would increase polypharmacy and hospital stay, so this option was not considered.
The miltefosine as a treatment for leishmaniasis was used from the start as an antineoplastic agent, until in India in 1998, it was used to treat visceral leishmaniasis. Today it is used in: Ethiopia, India, Colombia, Bolivia and Guatemala, for the treatment of cutaneous leishmaniasis; despite its gastrointestinal side effects, mild elevation of transaminases and creatinine and teratogenicity, that makes the drug that should be avoided or used with caution in women of reproductive age, it becomes one of the better tolerated treatment options.12 In studies conducted in Brazil with miltefosine (Impavido®), no amastigotes were observed in mice treated with higher doses of 30mg / kg / day for 21 days, and to confirm the cure of these, the parasite load was measured in their tissues when the 250 days of miltefosine cycle ends, by PCR. The complete clinical cure was obtained at doses greater than 30mg / kg / day,12 option when analyzing the comorbidities, the treatment and the cure reception at home, was the most viable alternative for the patient.
Acknowledgements: to Dr. Orlando Jaramillo Antillón and the Dermatology Department of the Mexico Hospital, for the great contribution of their knowledge and recommendations for this case.
Work performed at the Department of Dermatology, San Francisco de Asis Hospital, Grecia.
1Department of Dermatology of the Grecia Hospital, Costa Rican Department of Social Security. 2Department of Otolaryngology of the “Dr. Rafael Ángel Calderón Guardia” Hospital, Costa Rican Department of Social Security. fulincr@yahoo.com
REFERENCES
1. Valdir S Amato, Alexandre R. S. Padilha, Antonio C. Nico demo, Maria I. . S Duarte, Mario Valentini, David E. Uip, et al. Use of Itraconazol in the Treatment of Mucocutaneous Leishmaniasis: A Pilot Study. Int J Infect Dis. 2000;4:153-157. [ Links ]
2. Juan Diego Vélez L, Diana Cristina Carrillo C. Leishmaniasis cutánea y anfotericina B liposomal: Reporte de Caso. Infectio (Rev Colomb Infect). 2013;17: 201-204. [ Links ]
3. Valdir S Amato, Felipe F Tuon, Hélio A Bacha, Vicente A Neto, Antonio C Nicodemo. Mucosal leishmaniasis Current scenario and prospect for treatment. Acta Tropica. 2008;15:1-9. [ Links ]
4. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller BS, Leffell DJ. Fitzpatrick Dermatología en Medicina General. Octava ed. Madrid: Editorial Panamericana, 2013. [ Links ]
5. M Faye, Rotailer P. Particularidades de las infecciones otorrinolaringológicas en el medio tropical. Madrid: Editorial Masson, 2009. [ Links ]
6. Danny Zaghi BS, Claire Panosian, Miguel A Gutierrez, Aric Gregson, Emma Taylor, Maria Teresa Ochoa. New Wold cutáneos leishmaniasis: Current challenges in diagnosis and parenteral treatment. J Am Acad Dematol 2011;64:587-592. [ Links ]
7. Carol Singer, Donald Armstrong, Thomas C. Jones, Ronald H. Spiro. Imported Mucocutaneous Leishmaniasis in New York City. Am J Med 1975;59:444-447. [ Links ]
8. Barboza de Paulo LF, Rocha GF, Luisi CM, Rosa RR, Durighetto AF. Mucocutaneous leishmaniasis: mucosal manifestations in an endemic country. Int J Infect Dis 2013;17:e1088-e1089. [ Links ]
9. Joseph W Costa Jr, Danny A Milner, James H Maguire. Mucocutaneous leishmaniasis in a US citizen. Oral Surg oral Medicine Pathol 2003;96:573- 577. [ Links ]
10. Oliviera LF, Schubach AO, Martins MM, Passos SL, Oliveira RV, Marzochi MC et al. Systematic review of the adverse effects of cutaneous leishmaniasis treatment in the New Word. Acta Tropica 2011;118:87-96. [ Links ]
11. G. Antezana, R Zeballos, C Mendoza, P Lyevre, L Valda, F Cardenas et al. Electrocardiographic alterations during treatment of Mucocutaneous leishmaniasis with meglumine antimoniate and allopurinol. Trans R Soc Trop Med Hyg 1992;86:31-33. [ Links ]
12. Prado Godinho JL, Simas-Rodrigues C, Silva R, Ormenyi TP, de Souza W, C. F. Rodrigues J. Efficacy of miltefosine treatment in Leishmania amazonensisinfected BALB/c mice. Int J Antimicrob Agent 2012;39:326-331. [ Links ]
Received: August 21, 2015; Accepted: December 03, 2015











 texto en
texto en 


