Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Acta Médica Costarricense
versão On-line ISSN 0001-6002versão impressa ISSN 0001-6012
Acta méd. costarric vol.58 no.1 San José Jan./Mar. 2016 Epub 01-Mar-2016
Articles
Kluyvera cryocrescens Bacteremia
Hospital México, Infectious Diseases Department. munoz.ronny@gmail.com
The Kluyvera species were described in 1936 by Kluyver and van Niel. However, they were molecularly characterized by Farmer, in 1981. The genus contains 4 species: Kluyveracryocrescens, Kluyveraascorbata, Kluyvera georgiana, and Kluyveracochleae. The latter, has not been detected in humans.
This enterobacteria is a free-living organism, found in water, soil, sewers, hospital sinks, and animal-derived products. In human beings, it is part of the normal intestinal flora, but in small amounts. Most often, this pathogen behaves as a commensal organism, however, it can rarely lead to sickness, and also behaves as an opportunistic pathogen. It is unknown if the infections caused by this germ are endogenous versus acquired from the environment, or if both ways are equally important.
The Kluyvera species belong to the Enterobacteriaceae family, with Gram-negative bacilli that have peritrichous flagella, which allows them to move, catalase-positive and oxidase-negative, which grow in McConkey agar, they can ferment glucose, they are indole-positive, methyl redpositive; Vogues Proskauer-negative, citrate-positive, H2Snegative, urease-negative, phenylalanine deaminasenegative, and arginine dihydrolase-negative, lysine-positive, and ornithine decarboxylase-positive. The colonies are similar to E. Coli, however, they are drier and rougher.
The sites of infections vary. They include peritoneal fluid, urine, and skin, even bacteremia. As of now, there isn’t a specific clinical pattern of infections by this bacteria.
Case description
73 year old male, works in automotive repair, diabetic for over 20 years, has hypertension, dyslipidemia, ischemic cardiomyopathy for the post transurethral resection 7 years prior.
His last hospital admission was 11 months ago, secondary to an ischemic cerebrovascular accident due to atherothrombosis, which left a partial hemiparesis of left upper extremity and a Rankin 2. There is no history of smoking, alcohol intake or drug addiction.
The patient was admitted to the Emergency Room with a one month history of an infectious process of his 4th and 5th toes of the right foot. Empiric treatment with oxacillin and clindamycin was initiated , without response, and a systemic inflammatory response and fever persisted. He also was found to have severe arterial insufficiency involving the distal circulation of the right lower extremity, for which a below-the-knee amputation was recommended. After surgery, the systemic inflammation resolved, therefore oxacillin and clindamycin were stopped.
Several days after surgery, the patient remained oxygen dependent; bilateral reticulonodular lung infiltrates were documented on the chest x-ray and an increase in C-reactive protein (CRP) at 149 ng/ml, and for this reason empiric treatment with third generation cephalosporins (Cefotaxime) was started, and both blood and urine cultures were obtained.
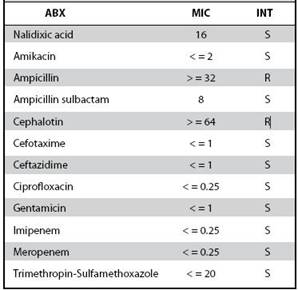
Both sets of blood cultures grew a gram-negative bacillus at 10.3 and 13.7 hours. Subsequently it was identified in VYTEK2 system as Kluyvera cryocrescens, which was corroborated as Kluyvera sp by analytical profile index. By that moment the antibiotic sensitivity testing was available and showed it was sensitive to cefotaxime (Table 1).
10 days of antibiotic treatment were completed with Cefotaxime, with a significant clinical improvement with a reduced requirement in oxygen supplementation and a significant decrease in the CRP.
Discussion
The Kluyvera cryocrescens infection is rare in humans; only 13 cases have been reported where Kluyvera cryocrescens has been isolated as the culprit pathogen. Of these, 9 have caused bacteremia (4 were considered a small outbreak in 2008, in a cardiovascular medicine ward), one in the urine of a patient with persistent proteinuria, one in the peritoneal fluid, one on bladder fluid in a patient with an acute emphysematous cholecystitis, and one case of soft tissue infection in a finger.
Some of the patients had a central venous catheter, as our patient did, but hasn’t been the most common finding.
The consistent presentation was fever, however, some cases presented with dyspnea, cough, chills, nausea, thrombocytopenia and hypoglycemia. The outcome appears to be favorable in the majority of the cases. Of the 13 reported cases of K. cryocrescens, only two died. In regards to the in-vitro treatment, K cryocrescens is naturally sensitive to tetracycline, aminoglycosides, ampicillin/sulbactam, ticarcillin, piperacillin-tazobactam, third-generation cephalosporins, carbapenems, aztreonam, quinolones, trimethoprim, chloramphenicol, fosfomycin and nitrofurantoin. Likewise, it is resistant in vitro to erythromycin, clarithromycin, lincosamides, streptogramins, glycopeptides, linezolid and rifampin.
The largest published experience with clinical success is with third-generation cephalosporins, fluoroquinolones, carbapenems and aminoglycosides, which comes from case reports. So, there isn’t a first- line treatment backed up by evidence. One must take into account the availability, cost, adverse reactions, toxicity, and development of resistance, at the time when starting treatment.
REFERENCES
1. Kluyver AJ and van Niel CB. Prospects for a Natural System of Classification of Bacteria. Zentralblattfür Bakteriologie, Bd 94 1936; 369-402; 377. [ Links ]
2. Farmer JJ 3rd, Fanning GR, Huntley-Carter GP, Holmes B, Hickman FW, Richard C, Brenner DJ .Kluyvera, a new (redefined) genus in the family Enterobacteriaceae: identification of Kluyveraascorbata sp. nov.andKluyveracryocrescens sp. nov.in clinical specimens. J. Clin. Microbiol. 1981; 13, 919-33. [ Links ]
3. Gil d de M, Navarrete CM; Lizama V, Zaror A, Arce E. Bacteremia caused by Kluyvera cryocrescens: report of two cases. Rev Chil Infectol 2001; 18:72-74. [ Links ]
4. Sarria JC, Vidal AM, Kimbrough RC 3rd.. Infections caused by Kluyvera species in humans. Clin. Infect. Dis.2001; 33, E69-74. [ Links ]
5. Paredes RD, Villalobos VJ, Avilés MA, Alvarado E. Meningitis por Kluyverasp. en una paciente con una derivación lumbo-peritoneal: Reporte de un caso. Acta Méd Costarric, 44, 126-12 [ Links ]
6. Toprak D, Soysal A, Turel O, Dal T, Özkan Ö, Soyletir G, Bakir M. Hickman Catheter-Related Bacteremia with Kluyvera cryocrescens: a Case Report. Jpn. J. Infect. Dis. 2008; 61, 229-30. [ Links ]
7. Jung-Chung L, Chi-Hsiang C, L KS and Feng-Yee C. Nosocomial Outbreak of Kluyvera cryocrescens Bacteremia. Infect Control Hosp Epidemiol. 2002; 23:62-4 [ Links ]
8. West BC, Vijayan H, ShekarR. Kluyveracryocrescens finger infection: case report and review of eighteen Kluyvera infections in human beings. Diagn. Microbiol. Infect. Dis.1998; 32, 237-41. [ Links ]
9. BolatF, Kilic SC, Abaci C, Cevit O, Gultekin A. A neonate with kluyvera sepsis: a case report. Iran. J. Pediatr. 2013; 23, 371-2. [ Links ]
10. Stock I. Natural Antimicrobial Susceptibility Patterns of Kluyveraascorbata and Kluyveracryocrescens Strains and Review of the Clinical Efficacy of Antimicrobial Agents Used for the Treatment of Kluyvera Infections. J Clin Microbiol. 1981; 13: 919-933 [ Links ]
Received: May 12, 2015; Accepted: October 29, 2015











 texto em
texto em