Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Acta Médica Costarricense
On-line version ISSN 0001-6002Print version ISSN 0001-6012
Acta méd. costarric vol.58 n.1 San José Jan./Mar. 2016 Epub Mar 01, 2016
Brief communications
Basic characteristics and treatment regimens in people with type 2 diabetes who participated in the International Diabetes Management Practices Study in Costa Rica
5Panamerican Clinic. San José, Costa Rica maryvinocour@yahoo.es
The IDMPS1 (International Diabetes Management Practice Study) is an observational, multinational investigation in which the objective was to assess the standard of care for patients with diabetes in different regions in the world and to evaluate adherence to international guidelines on diabetes management. A total of 15016 patients with type 2 diabetes, older than 18 years, were evaluated worldwide and 27 countries from Eastern Europe, Asia, Africa and Latin America, including Costa Rica, participated. In this paper, the results from the IDMPS study in Costa Rica are presented, and compared to the information obtained from Latin America.
Methods
The study was approved by the Institutional Review Board of Universidad de Ciencias Médicas (CEC-UCIMED). Patients with type 2 diabetes who attended the private practice of 5 Costa Rican endocrinologists were included, after accepting to participate voluntarily and signing the informed consent. A questionnaire designed to collect data on anthropometric measurements, diabetes evolution, glucose levels, glycated hemoglobin (HbA1c ) and type of treatment received was used.
Results
Each of the endocrinologists recruited an average of 10 patients, who visited their practice during a two week period. Forty nine patients with type 2 diabetes who had an appointment between March 22nd and April 24th 2007 comprise the study group. Mean age was 59,3± 11,6 years; body mass index (BMI) was 30,84 ± 5,71 kg/m2 (men 30,6 ± 4,6 and women 31,05 ± 6,5) and mean disease duration was 11,59 ± 8,44 years.
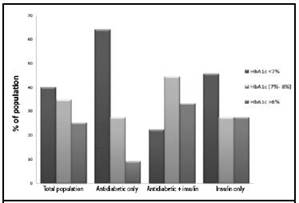
Sixty percent of patients had HbA1c >7%, and specifically, 17,5% of Costa Rican patients had HbA1c >9%. This percentage is similar to that from data collected for Latin America in the original study. HbA1c levels of Costa Rican patients and of patients from the Latin America study are shown in figure 1.
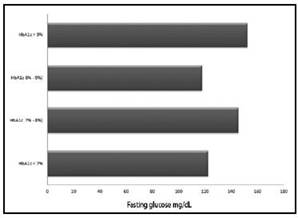
Regarding fasting glucose levels, the patients had a mean value of 140,45 ± 56,3 mg/dl. Figure 3 compares the results obtained for HbA1c to those obtained for fasting glucose. Patients with HbA1c lower than 7% had a mean fasting glucose of 122,3 ± 25,9 mg/dl, a figure similar to the one from the group that had HbA1c between 8% and 9%. Patients with HbA1c greater than 9% had a mean fasting glucose of 152,5 ± 36,3 mg/dl.
Discussion
When analyzing glycemic control in Costa Rican patients with diabetes in the study, it was found that the percentage not achieving the goal, those with HbA1c > 7%, was 60%. In fact, 17,5% of the patients in the study had a HbA1c higher than 9%. As it can be observed, most patients are not achieving the goal, similar to what has been found in other countries in Latin America, where the HbA1c goal is not achieved in 63% of the cases, which demands a call to action.1
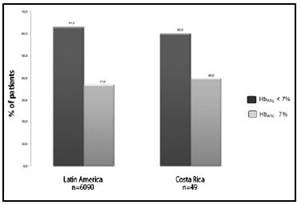
Figure 1: Glycemic control in patients with type 2 diabetes. Comparison between Latin America and Costa Rica.
By carefully analyzing the type of therapy used by these patients, it is seen that 100% were receiving pharmacotherapy, which is consistent with international guidelines that recommend adding at least metformin to diet and exercise for the treatment of type 2 diabetes mellitus.
Of all patients treated with oral antidiabetic agents exclusively, 63,6% reached the HbA1c goal of less than 7%. However, 36,4% did not achieve the goal (HbA1c >7%). Furthermore, as shown in figure 2, only 22,2% of the patients treated with a combination of oral antidiabetic agents and insulin reached the goal. Data on patients treated with insulin showed that 45,5% had a HbA1c <7%. This correlates with other studies, where the patient treated with insulin has less glycemic control, probably secondary to greater beta cell failure.2 Poor adherence also must be considered, since multiple studies have demonstrated that treatment adherence in type 2 diabetes is not optimal, and is comparable with that of other chronic diseases.3
Interestingly, the group of patients treated with a combination of oral antidiabetic agents and insulin was the one with the highest percentage of patients not controlled: 77,8%. Out of these, 44,4% had HbA1c levels in a range between 7% and 8%, and 33,4% had HbA1c levels > 8%.
Some possible explanations could be the following: 1-delay in the onset of insulin therapy, 2- lack of adjustment of basal insulin dose, 3- delay in the start of a second prandial dose of insulin, or delay in adjustment of a mixed insulin regimen, or simply selection bias given the characteristics of the study.
Additionally, it must be considered that failure to reach the goal might be due to lack of adherence to a complicated treatment regimen, such as the combination of oral antidiabetic agents and insulin.4 When analyzing which group of patients, according to therapeutic group, had worst control (HbA1c > 8%), the same relation previously discussed was found, where the group with antidiabetic agents plus insulin had the highest percentage of uncontrolled patients (33,4%). Researchers like Lerman I., suggest strategies to improve treatment adherence, such as keeping the treatment regimen as simple as possible, discussing priorities with the patient, educating about treatment adherence and monitoring it on every visit, among others.4
The results displayed in figure 3 indicate that fasting glucose, by itself, is not enough to monitor control in a patient with diabetes, and it is necessary to measure postprandial glucose and, obviously HbA1c.5
This coincides with studies published by Monnier I. et al,6 which showed that at higher HbA1c levels, the main contributor to overall hyperglycemia is fasting glucose, and as HbA1c approaches the goal, the main contributor is postprandial glucose.7
Important studies have demonstrated the great impact that glycemic control exerts in terms of cardiovascular complications, as described by the UKPDS,8 that showed that for every 1% reduction in HbA1c the risk for microvascular complications decreased by 35% and the risk for macrovascular complications decreased by 16%.
Unfortunately, despite this and other publications, and recommendations regarding therapeutic approaches from organizations such as the American Diabetes Association, most Costa Rican patients did not achieve the HbA1c goal.8,9
Therefore, we conclude that it is necessary to emphasize on creating guidelines that are more efficient, and to increase efforts in seeking a broader access to diabetes education for patients and their families in Costa Rica, as well as in Latin America.
Referencias
1. Ringborg A, Cropet C, Johnson B, Gagliardino J, Ramachandran A, Lindsgren, P. Resourse use associated with type 2 diabetes in Asia, Latin America, the Middle East and Africa: Results from the International Diabetes Management Practices Study (IDMPS). Int J Clin Pract. 2009; 63:980-982. [ Links ]
2. Turner RC, Cull Ca, Frighi V, Hollman, RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA.1999; 281:2005-2012. [ Links ]
3. Sapkota S, Brien J, Greenfield J, Asiani P. A Systematic Review of Interventions Addressing Adherence to Anti-Diabetic Medications in Patients with Type 2 Diabetes - Components of Interventions. PLoS ONE. 2015; 10: e0128581. [ Links ]
4. Lerman I. Adherence to Treatment: The Key for Avoiding Long - Term Complications of Diabetes. Archives of Medical Research. 2005; 36:300-306. [ Links ]
5. Brown JB, Nichols GA, Perry A. The burden of treatment in type 2 diabetes. Diabetes Care.2004; 27:1535-1540. [ Links ]
6. Monnier L, Lapinsky H, Colette C. Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetes patients. Diabetes Care.2003; 26:881-885. [ Links ]
7. American Diabetes Association. Standards of Medical Care in Diabetes-2009. Diabetes Care. 2009; 32:193-203. [ Links ]
8. U.K. prospective Diabetes Study group. UK. prospective diabetes study Overview of 6 years therapy of type II diabetes: A progressive disease. Diabetes.1995; 44:1249-1258. [ Links ]
9. Chacra A, Davidson J, Diaz J, Escalante M, Litwack L, Mestman J, More L, Violante R. An algorithm for the treatment of type 2 diabetes in Latin America. Diabetes, Obesity and Metabolism. 2005; 7:148-160. [ Links ]
Received: March 27, 2015; Accepted: September 27, 2015











 text in
text in