Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Médica Costarricense
versión On-line ISSN 0001-6002versión impresa ISSN 0001-6012
Acta méd. costarric vol.54 no.1 San José ene./mar. 2012
Original
Abbreviations: TCI, transient cerebral ischemia; NIHSS, National Institutes of Health Stroke Scale
Contact information:
Monteromiguel@yahoo.com
Abstract:
Background and aim: To determine the morbi-mortality of patients treated with endovascular stenting for Carotid Artery disease at San Juan de Dios Hospital, Costa Rica; from January 2007 to February 2010.
Methods: A retrospective observational registry of patients treated with Carotid Artery endovascular stenting was maintained at our institution over 13 months. Based on the information acquired from medical records, two subgroups were identified: symptomatic and asymptomatic. Some aspects were researched and evaluated such as risk factors, ABCD2 scale, affected cerebral territory, invasive and non-invasive lesion measurements, stent sizing and finally peri-operatory complications.
Results: 76 patients were identified in this series, 87% (n=66/76) symptomatic and 13% (n=10/76) asymptomatic. The most frequent risk factor was hypertension, followed by smoking. Underestimation by ultrasound of lesion severity was found in up to 24% (n=18/76) of patients. Predilatation was done in 55% (n=42/76) and most frequent stent sizes identified were 7x30mm or 8x30mm in 47% (n=36/76) of patients. Neurologic morbidity of asymtomatic patients was 0%, and in the symptomatic group was a 3% (2/66)
Conclusion: Endovascular therapy demonstrated to be a safe and effective as a revascularization technique; however larger patient series should be investigated for grater statistical significance.
Keywords: Endovascular procedures, Carotid Stenosis, stroke
Strokes are a major cause of mortality and permanent disability in the world, affecting not only those that experience them,but also their family and community1. Circulatory system diseases are the leading cause of death2 in Costa Rica, and it has been deduced that as the elderly population increases,the number of stroke cases will increase worldwide;thus, by 2030, the number of deaths due to strokes will double.3
The NIH (National Institute of Health) and the NINDS (National Institute of Neurological Disorders and Stroke)4, as well as the Spanish guidelines for the primary and secondary prevention of ictus,1classify the risk factors for this disease in unmodifiable, among them, age, male gender, African-American race and hereditary factors; and modifiable, such as hypertension, diabetes mellitus, cigarette smoking, obesity, lack of physical activity, high blood cholesterol levels, sickle-cell disease, alcoholism, hormonal therapy, atrial fibrillation, carotid stenosis, left ventricular hypertrophy, hypercoagulation and prior strokes.5
Knowledge about these risk factors and the completion of massive studies on invasive treatment6-8 have allowed the implementation of primary and secondary preventive interventions that could lead to a decrease in stroke incidence. Among these, the carotid endarterectomyis considered the best therapeutic alternative1,9 for asymptomatic patients with stenosis equal or greater than 80%10, leading toa 5.9% fall in strokesat 5 years,11 and for symptomatic patients with stenosis greater than or equal to 50%1,9, resulting in a fallof up to 13.3 to 15.6% at 5 years.5,11
Materials and methods
The medical records of patients discharged from San Juan de Dios Hospitaland treated with carotid revascularization therapybetween January 2007 and February 2010 were reviewed. The information obtained was patient's general data (age, sex, reason for admission), site of admission (outpatient clinic, emergency room, transfer, re-admission), stroke risk factors(hypertension, diabetes mellitus, cigarette smoking, alcoholism, atrial fibrillation, high blood cholesterol levels, carotid stenosis, hormone therapy, hypercoagulation, priorstrokes), carotid artery disease (TCI or stroke) or asymptomatic,degree of carotid stenosis evidenced byultrasound and arteriography; and finally, peri and postoperative complications. It should be noted that neurological complications were identified througha NIHSS assessment performed by specialists in neurology. The hospital's Research Ethics Committee approved the study (document 16-2010 CLOBI-HSJD).
Results
Overview
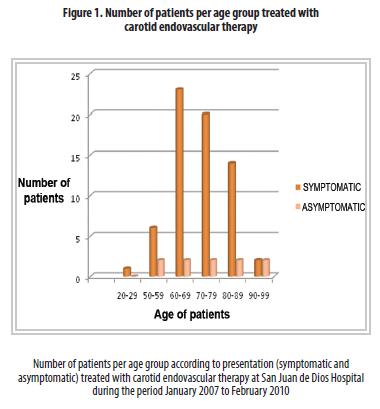
76 patients that received the mentioned treatment were identified. Out of this group, 13% (n=10) were asymptomatic and 87% (n=66) symptomatic. Most of them were in their 6thdecade (see figure #1) and only one patient that had suffered a previous strokewas in her twenties, she suffered from Takayasu Disease.
Out of the total of asymptomatic patients, 60% (n=6) came to the Department of Vascular Medicinevia the outpatient clinic, while 40% (n=4) of them were transferred by other departments. None of them was admitted through the emergency service.
In contrast, 64%(n=42) of the symptomatic patients were admitted by the emergency service due to acute cerebrovascular symptomatology (stroke or TCI), 27% (n=18) were admitted by the outpatient clinic, and 9% (n=6) were transferred by another service.
In terms of stroke risk factors, the most frequentone insymptomatic patients is hypertension; followed by high blood cholesterol levels, cigarette smoking, prior stroke, alcoholism and diabetes mellitus;whereas, in asymptomatic patients,both hypertension and cigarette smoking have the same prevalence, followed by atrial fibrillation and dyslipidemia; there is a lower incidence of diabetes mellitus and alcoholism (see table # 1). Hypercoagulation and sickle cell disease were not recorded in the medical records. However, when the patients'laboratory tests were reviewed, they showed that noneof the patients suffered fromsaid diseases. The presence of left ventricular hypertrophy was not recorded in 20 of the medical records reviewed. With respect to hormone replacement therapy, the patients' anamnesis did not record whether they had used it or not, therefore, it was not possible to determine the incidence of this risk factor.
Severity of injury (percent stenosis)
The preoperative ultrasound showed stenosis greater than 70% in 100% (n=10) of the asymptomatic patients, this concurred withthe arteriographic findings.
In the symptomatic patients, the ultrasound showed a 50-70% stenosis in 39% (n=26) of patients and a 70-99% one in 61% (n=40) of them. However, when the angiography was performed, 13% (n=8) showed an obstruction of 50-70%, while 87% (n=58) had an obstruction greater than 70%.
- Medical assessment at time of admission (symptomatic patients, n=66):
TCI was recorded for 33% (n=22) of symptomatic
patients;theinitial ABCD2 classification is shown in table #2.
67% (n=44) of patients were diagnosed with a cerebral infarction. The
most
frequent diagnoses recorded in these cases were the territory of the
middle
cerebral artery and multi-infarct disease, which represented 45% (n=20)
of
this subgroup. 18% (n=8) had an injury in the posterior cerebral artery
and
in 36% (n=16) of the cases; the brain territory injuredwas not
specified.
NIHSS Tool:
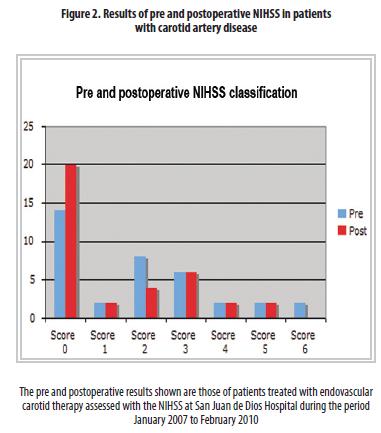
Regarding the assessment with the NIHSS, 36 patients underwent a pre and postoperative assessment, 4 only hada preoperative one,6 only a postoperative assessmentand 30 of the patients were not assessed with the scale.
Out of the 36 patients with pre and post assessment, 61% (n=22) maintained the same rating on the scale, 33% (n=12) scored higher and 6% (n=2) scored lower.
Out of the
patients who, according to the scale, improved their condition, 6
improved
it by one point, 2 improved it by 2 points, 2 by 3points and 2 by 5
points
(see figure # 2).
Surgical technique
The most frequent stent sizes identified were the 8x30 ones, usedin 31% (n=24) of the cases, followed by the 7x30 ones in 15% (n=12) of cases; the rest were not used that often. The performance of pre-dilation was recorded in 42 cases (55%) (n=42) and post-dilationwas performed in all cases (n=76).
Pharmacotherapy
All patients were administered a 100 mg dose of aspirin per day, regardless of whether they were taking it. In addition, all were administered Clopidogrelpremedication (a 300 mg loading dose on preoperative day), and a maintenance dose of 75 mg per day for a month after surgery.
During surgeryhigh molecular weight heparin was administered to all patients, the mean dose was of 6000 IU (maximum 10,000 U and minimum 4000 U). Likewise, a 1 mg dose of Atropine was administered 2 minutes before handling the carotid sinus.
Complications
The asymptomatic patients did not experience complications, so the associated morbimortality was zero percent. None of them was assessed with the preoperative or postoperative NIHSS.
With regard to symptomatic patients, only two had postoperative neurologic deterioration, resulting in a 3% morbimortality (n=2/66). During the postoperative, one of the patients developed a conversion from an ischemic to a haemorrhagicstroke, which required assisted mechanical ventilation. Afterwards, the patient died due to a nosocomial pneumonia that aggravated his condition. The other one deteriorated the NIHSS from 3 to 5because it suffered from left hemiparesis after surgery.
Discussion
Endovascular therapy for carotid artery disease is a matter of global concern. There is still no international consensus on its prescription. However, it seems prudent to determine the morbidity frequence in relation to the procedure for the sake of future decisions that impact on the welfare of our patients.
The age distribution of our patients follows the one reported by other authors in larger samples10. However, the number of octogenarian patients in our sample that had good results is remarkable, despite the existence of scientific reports that claim greater morbimortality in patients older than 80 years.13
A detail regarding the patient admission mechanism should be highlighted. Up to 27% of patients were admitted as a result of orders prescribed by the outpatient clinic. This does not guarantee a prompt admission of the patient.
Except for the case of very extensive ischemic events (which are readmitted at least 6 weeks later), all symptomatic events (transientor obstructive) are emergencies that require early treatment of the carotid emboligenic focus. This is why immediate admission, as an emergency, of patients in this condition must be required.
Sonographic screening is key to decision making in patients with carotid artery disease.14 However, there is no adequate correlation between the severity of the injury estimated fromthe ultrasoundand the one found through the arteriography. It is essential to strengthen training in vascular sonographic screeningof those responsible for undertaking the diagnosis studies, looking towards amore real correlation; this would greatly aid the clinicianin taking intelligent decisions regarding the management of these patients.
The objective measurement of the perioperative neurological condition was established with the assistance of the Neurology Department and using the NIHSS scale. 39% of patients were not assessed with this scale because it was established as a protocol only after the second half of 2008. However, today is a useful and replicable tool that validates the results of an invasive procedure.
Furthermore, it helps establish in an objective manner the perioperative morbidity, thus aiding the clinician in the adoption of treatment decisions according to the operative risks faced by its patients when undergoing an invasive procedure. In the case of San Juan de Dios Hospital, international standards are met, something which is evidenced by a 0% morbidity in the treatment of asymptomatic patients (up to 3% is allowed) and a 3% (n=2/66) in symptomatic patients (up to 6% is allowed).6
The deterioration in the NIHSS scale in 12 of the patients does not translate into adverse events forall this subgroup. This scale has a certain intra and inter-observer laxity, thus, the differences should be at least 4 points. This means that only 2 patients had a significant deterioration and were recorded as perioperatory morbidity.15
It is worth mentioning that one of the patients with the most morbidityhad no trans or post-operative embolic injuries. However, in the immediate postoperative (during recovery), he developeda hypertensive crisis.
Despite this being a modest and initial sample of carotid endovascular therapy at San Juan de Dios Hospital, the goal is to exhibit the internaltreatment protocol and determine the perioperative morbidity. It is clear that the number of patients in this samplemust be increased in order to seek greater statistical significance, however, the initial results are encouraging because they meet international standards. Moreover, they work as an objective tool to make appropriate clinical decisions.
Contribution of each author
Christian Fonseca-Bolaños, Miguel Montero-Baker and Johana Vasquez-Cespedes: Data collection, bibliographic research, preparation and review of discussion.
References
1. Guía de práctica clínica sobre la prevención primaria y secundaria de ictus. Madrid, España: Centro Cochrane Iberoamericano, 2009. [ Links ]
2. Situación de la Salud en Costa Rica, Indicadores básicos de salud 2008. Costa Rica: Ministerio de Salud, 2008. [ Links ]
3. Smith W, English J, Claiborne S. Enfermedades Cerebrovasculares. En: Fauci A., Braunwald E., Kasper D, Hauser S, Longo D, Jameson J., editors. Harrison Principios de Medicina Interna. 17a edición. México, Mc Graw Hill Interamericana, 2009: 2513-2536. [ Links ]
4. Stroke: Challenges, Progress and Promise. Estados Unidos: National Institute of Neurological Disorders and Stroke and National Institutes of Health, 2009. [ Links ]
5. Allan H. Ropper, Martin A. Samuels. Adams y Victor, "Principals of Neurology". Octava Edición. Mc Graw Hill, United States 2009. Pág. 660-740 [ Links ]
6. Moneta G, Edwards J, Chitwood R, Taylor L, Lee R, Cummnings C. "Correlation of North American Symptomatic Carotid Endarterectomy Trial (NASCET ) angiographic definition of 70% to 99% internal carotid artery stenosis with duplex scanning" Journal of Vascular Surgery. 1993 Jan;17:152-7 [ Links ]
7. Chang Y, Golby A, Albers G. "Detection of Carotid Stenosis from NASCET Results to Clinical Practice" Stroke. 1995;26:1325-1328. [ Links ]
8. Chambers BR, Donnan GA. "Carotid endarterectomy for asymptomatic carotid stenosis" (Cochane Review) en: http://www.update-software.com Consultado el 24 marzo 2010 [ Links ]
9. Marine L. "Tratamiento endovascular selectivo de la ateroesclerosis de la bifurcación carotídea". Rev. chil. cir 2008, 60: 503-510. [ Links ]
10. Gurm H, Yadav J, Fayad P, Katsen B, Mishkel G, Bajwa T. "Long- Term Results of Carotid Stenting versus Endarterectomy in High- Risk Patients". N Engl J Med 2008; 358:1572-1579. [ Links ]
11. Inzitari D, Eliasziw M, Gates P, Sharpe B, Chan R, et al. "The Causes and Risk of stroke in patients with asymptomatic internal- carotid-artery stenosis". N Engl J Med 2000; 342:1693-1700. [ Links ]
12. Chila S, Clagett P, Higashida R. "Management of Carotid Stenosis". N Engl J Med 2008; 358; 1617-1621 [ Links ]
13. Chaturvedi S, Matsumura JS et. Al. Carotid artery stenting in octogenarians: periprocedural stroke risk predictor analysis from the multicenter Carotid ACCULINK/ ACCUNET Post approval Trial to Uncover Rare Events (CAPTURE 2) clinical trial. Stroke 2010; 41:757-64 [ Links ]
14. Schreiber S, Schoof J, Heinze HJ, Kozian A, Huth C, Kropf S. "Implementation and efficacy of selective sonographic screening for carotid disease befote cardiac surgery" Ann Vasc Surg 2010; 24(3): 383-7 [ Links ]
15. Lyden PD, Lu M., Levine SR, Brott TG, Broderick J. "A modified NIGSS for use in stroke clinical trials: preliminary reliabiltiy and validity". Stroke 202; 32: 1131-7Allan H. Ropper, Martin A. Samuels. Adams y Victor, Principios de Neurologia. Mc Graw Hill, México 2011. Página 746-83 [ Links ]
16. Allan H. Ropper, Martin A. Samuels. Adams y Victor, Principios de Neurologia. Mc Graw Hill, México 2011. Página 746-837 [ Links ]
17. Allan H. Ropper, Martin A. Samuels. Adams y Victor, Principios de Neurologia. Mc Graw Hill, México 2011. Página 746-837 [ Links ]
Fecha recibido: 7
febrero
2011 Fecha
aceptado: 15
noviembre
2011











 texto en
texto en