Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Acta Médica Costarricense
versión On-line ISSN 0001-6002versión impresa ISSN 0001-6012
Acta méd. costarric vol.53 no.4 San José dic. 2011
Clinical Case
HIV associated Dementia, a case report
(Síndrome demencial asociado a VIH/sida. A propósito de un paciente)
Ricardo Boza-Cordero
Abtract:
HIV affects the nervous system producing different clinical manifestations, for which neuropsychological disorders are the most common. Up to 25% of autopsies have histopathological changes due to HIV. Currently it is considered that HIV-associated dementia (HAD) is the most common cause of dementia for people less than 40 years old. Diagnosing HAD is very important because it is considered an AIDS defining illness, its presence affects treatment adherence and antiretroviral drugs could revert its progress. Studying and following these patients should be based on clinical observation, neuropsychological analyses and neuroimaging. This case presents a 39- year-old male, who started with progressive memory loss and distal tremor; and diagnosed as an HIV associated dementia by clinical, neuropsychological and neuroimaging methods. Emphasis is placed on the pathophysiology of this disorder, the importance of proper diagnosis and the use of antiretroviral therapy.
Keywords:
HIV, Human
Immunodeficiency Virus; HAD, HIV associated
dementia;
CNS, Central Nervous System; SPECT, Single Photon Emission Computed
Tomography;
HAART, Highly Active Antiretroviral Therapy
Since first AIDS cases described in the 80´s, it was seen that neuropsychological changes were the main manifestations of CNS compromise.1,3 This is how it was demonstrated the presence of dementia as a direct patophysiological effect of HIV illness and as a chronic neurodegenerative process, with a variable frequency (15-50%) for different published series.
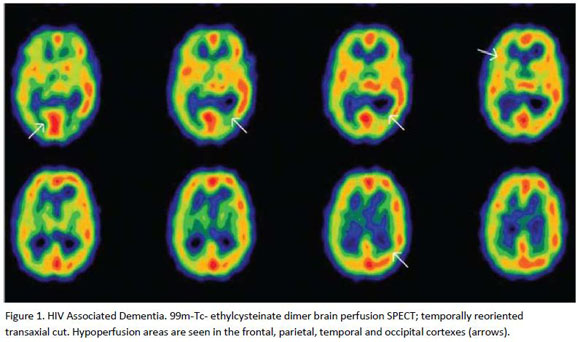
An HIV/AIDS patient is presented, diagnosed with Dementia Syndrome by several psychological tests, CT-scan and SPECT changes, compatible with brain atrophy and HAD.
Case Presentation
A 39-year-old, costarican salesman, with incomplete college education, started in 1996 with control at the San Juan de Dios Hospitals HIV/AIDS Clinic. At that time, he had a TCD4+ cell count of 672 cells/mm3 and was classified as having an asymptomatic HIV infection.
That same month a neuropsychological evaluation (performed at the Psychiatry and Mental Health service) using several tests showed "significant neuropsychological alterations in attention and concentration functions, as in verbal and visuospatial memory, compatible with dementia". The study at the Social Work service in 2005 and 2007 revealed "weak critical consciousness about his disease and without effective support networks. Absent to control appointments". The patient was proposed to start antiretroviral therapy (HAART), which he rejected. The last evaluation was made on July 2009. Insistence was made for him about the need to start HAART, which he rejected once again. The patient continued with an important recent and past memory, with a lot of difficulty to recognize his relatives and their names, his distal hand tremor persisted.
Discussion
The American Academy of Neurology recently established a nosology to classify these pathologies.6 Briefly, neurocognitive disorders could be 1. Asymptomatic 2. Mild 3. HAD. To get more information about them, look at references 3,5 and 6. In general, these entities evolve progressively, just like HIV/AIDS. This is a diagnosis of exclusion, by ruling out delirium and other causes of dementia such as depression, tumors, cardiovascular disease or infections.
In Costa Rica, at San Juan de Dios Hospital, Quesada C and co-workers (not yet published data), made an analysis of 31 recently diagnosed HIV/AIDS patients, and applying the international HAD test, they found that at least 24 of these patients had some degree of cognitive compromise (77.42%). Seven (22.6%) did not have any secondary cause for the disorder, therefore classified as having HAD.
Most of them were men, and all of them had TCD4+ lymphocyte counts < 200 cells/mm3.
On a multi-centric study14 it was concluded that there is not enough evidence to establish a relationship between cortical atrophy and cognitive defects, and probably studies need a great sensibility to find any relation. However, caudate nucleus atrophy is correlated to neuropsychological disorders, and there is a contributory role for cortical and subcortical atrophy, but to an uncertain level. In fact, by functional studies, it has been demonstrated that HAD diagnosis must be made by finding caudate nucleus atrophy, and not by determining the volume of white matter.10 Therefore, the presence of cortical or subcortical atrophy does not imply HAD.
In summary, the correlation with different imaging diagnostic methods is useful for both diagnosis and antiretroviral therapy follow up.
References
1. Koralnik IJ Neurologic Diseases Caused by HIV tipe 1 and Opportunistic Infections In Mandell, Douglas and Bennett´s Principles and Practice of Infectious Diseases 7th edition Philadelphia, PA Churchill Livingstone 2010;1737-1743. [ Links ]
2. Singer EJ Valdes-Sueiras M Commins D Neurologic Presentations of AIDS Neurol Clin 2010;28:253-275. [ Links ]
3. McArthur JC Brew BJ Nath A Neurologic complications of HIV infection Lancet Neurol 2005;4:543. [ Links ]
4. Levy JA HIV and the Pathogenesis of AIDS 2d edition Washington DC ASM Press 2007;183-200. [ Links ]
5. Goodkin K Aronow A Baldwin G HIV-1 Associated Neurocognitive Disorders in the HAART Era In Goodkin K Shapshak P Verma A The Spectrum of Neuro-AIDS Disorders First Edition Washington DC ASM Press 2009; 3-27. [ Links ]
6. Antinori A Arendt G Becker JT Brew BJ Byrd DA Cherner M et al Updated research nosology for HIV-associated neurocognitive disorders Neurology 2007;69:1789-1799. [ Links ]
7. Eggert D Anderson E Zheng J Chemokines and the Neuropathogenesis of HIV-1 Infection In Goodkin K Shapshak P Verma A The Spectrum of Neuro-AIDS Disorders First Edition Washington DC ASM Press 2009;151-171. [ Links ]
8. Wang Z Trillo-Pazos C Kim SY Effects of human immunodeficiency virus type 1 on astrocyte gene expression and function: potential role in neuropathogenesis. J Neurovirol 2004; 10 (suppl l):25-32. [ Links ]
9. Maki PM Cohen MH Weber K Little DM Fornelli D Rubin LH et al Impairments in memory and hippocampal function in HIV-positive vs HIV-negative women. Neurology 2009;72:1661-1668. [ Links ]
10. Ances BM Roc AC Wang J Korczykowsky M Okawa J Stern J et al Caudate blood flow and volume are reduced in HIV + neurocognitively impaired patients Neurology 2006;66:862-866 [ Links ]
11. Sacktor NC Wong M Matthew N Skolasky N Richard L Selnes O et al The International HIV Dementia Scale: a new rapid screening test for HIV dementia. AIDS 2005 ;19:1367-1374. [ Links ]
12. Marra CM Zhao Y Clifford DB Letendre S Evans S Henry K et al Impact of combination antiretroviral therapy on cerebrospinal fluid HIV RNA and neurocognitive performance AIDS 2009;23:1359-1366. [ Links ]
13. Robertson KR Smurzinski M Parsons TD Wu K Bosch R Wu J et al The prevalence and incidence of neurocognitive impairment in the HAART era AIDS 2007; 21: 1915-1921. [ Links ]
14. Thurner MM Post JD The Uses of Structural Neuroimaging in the Brain in HIV-1 Infected Patients In Goodkin K Shapshak P Verma A The Spectrum of Neuuro-AIDS Disorders First Edition Washington DC ASM Press 2009;247-272. [ Links ]
15. Thurner MM Post JD Neuroimaging in the Brain in HIV-1- Infected Patients Neuroimag Clin N Am 2007; 18:93-117. [ Links ]
16. Schwartz RB Komaroff AL Garada B Gleit M Doolittle TH Bates DW et al SPECT Imaging of the Brain: Comparison of Findings in Patients with Chronic Fatigue Syndrome, AIDS Dementia Complex and Major Unipolar Depression AJR 1993;162:943-951. [ Links ]
17. Camargo EE Brain SPECT in Neurology and Psychiatry J Nucl Med 2001;42:611-623. [ Links ]
18. Ernst T Tomasi D Chang L Functional Magnetic Resonance Imaging in HIV-Associated Dementia In Goodkin K Shapshak P Verma A The Spectrum of Neuro-AIDS Disorders First Edition Washington DC ASM Press 2009;273-280. [ Links ]
Infectologist
Physician, HIV/AIDS Clinic, San Juan de Dios Hospital. Associated professor at UCR (Universidad de Costa Rica)
School of Medicine *Correspondence:
Ricardo Boza Cordero E-mail:
ricardob49@hotmail.com











 texto en
texto en