Introduction
Vital pulp therapy (VPT) is a dental procedure to preserve pulp vitality and consists of using a biocompatible material on the exposed pulp of the teeth (1). Several materials with a good sealing ability are used for pulp capping such as calcium hydroxide, mineral trioxide aggregate (MTA) and silicate-based cements (BioAggregate®, EndoSequence®, BiodentineTM (BD), etc.) (2).
BD (Septodont, Saint Maur des Fosses, France) is a unique calcium silicate-based cement, which has been used as a dentin replacement material under composite restorations, direct pulp capping and endodontic treatment (3). BD consists of dicalcium/tricalcium silicate, calcium carbonate (as a filler) (4), zirconium oxide (as an opacifier) (5), and calcium chloride containing liquid. Calcium chloride is a water-reducing agent that accelerates the setting time of BD. The incorporation of calcium chloride into the liquid improves the mechanical properties of the cement as well (6). Compared to MTA, BD has exhibited better sealing ability, biocompatibility and bioactivity, higher mechanical properties, shorter setting time and lower microleakage (7).
The capability to seal the pulp-capping materials is one of the most important issues in VPT. Keeping the cements intact affects the prognosis of the treatment procedure. Because of the fragility and unsatisfactory esthetics of BD, it is better to make the final filling with different restorative material, usually a composite one. Resin-based composites are common restorative materials, used both in anterior and posterior regions. The bond strength between BD and the composite resin has an important role in achieving the final restoration, which depends on the procedures associated with the application of the adhesive system. A sufficient bond between the restorative material and the pulp-capping material can distribute stresses beyond the bonded surface, reduce microleakage and increase the strength of the remaining tooth structure (8). Hence, the bond strength of any restorative material to pulp capping agents has been an issue of concern; consequently, the adhesive strategy used for the final restoration on calcium-silicate cement is of clinical interest.
Several studies investigated the bond strength of BD using various types of bonding systems. Some authors suggest the superiority of the self- etch (SE) systems over the etch-and-rinse (ER) mode (9,10), while other literatures report that the ER mode provides higher bond strength of the tested materials (11,12). The aim of this in vitro study was to evaluate the SBS of a ''no-wait'' universal adhesive (UA) applied to BD in different etching modes, followed by the placement of different composite resin types. The null hypotheses were: (1) the etching mode will have no effect on the SBS and there will be no significant difference between the ER and SE mode; (2) the composite resin type will have no effect on the SBS and there will be no significant difference between the tested composite resins.
Materials and methods
Sample size calculation
The sample size was determined according to the previous studies (13,14). To achieve a medium effect size (d=0.50), with 95% power and a 5% type 1 error rate, ten samples were needed for each group.
Specimen preparation
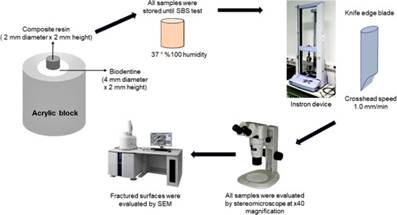
Eighty specimens of BD were fabricated using cylindrical acrylic blocks (Paladur, Heraeus Kulzer, Hanau, Germany) with a 5mm central hole in diameter and 2mm in depth. BD was mixed according to the manufacturer's instructions and placed in each acrylic block. To ensure standardization of the sample surfaces,a glass slab was placed on top of the blocks so that BD set against a smooth surface. After initial setting time of 12min, all specimens were covered with wet gauze and stored at 37ºC with 100% humidity in an incubator to encourage setting time.
The materials used in this study, their compositions and batch numbers are shown in Table 1.
Table 1 Adopted materials and their compositions, batch numbers, and application procedures.
The specimens were randomly assigned into four groups (n=20) according to the composite resin type used:
Group FZ250: Filtek Z250 Universal Restorative (3M ESPE, St Paul, USA)-microhybrid composite resin.
Group SDR: SDR Plus U Bulk Fill Flowable (Dentsply Sirona, USA)- low-viscosity bulk-fill composite resin.
Group FBP: FiltekTM Bulk Fill Posterior (3M ESPE, St Paul, USA)- high-viscosity bulk-fill composite resin.
Group EF: EsFlow™ Universal Flowable Compo- site (Spident Co Ltd, Korea)-nanohybrid flowable composite resin.
Then, each group was divided into 2 subgroups according to the etching mode (ER and SE) applied (n=10). Clearfil Universal Bond Quick (Kuraray Noritake, Tokyo, Japan) (CUQ) was applied to the specimens in two different etching modes according to the manufacturer's instructions. Resin composites were placed at the center of BD surfaces by using cylindrically shaped plastic tubes with an internal diameter of 2mm and a height of 2mm and polymerized with a light-emitting diode (VALO Cordless; Ultradent, South Jordan, USA) for 20 s. All specimens were stored in distilled water at 37°C for 24h before testing. After the storage period, the plastic tubes were removed carefully from all specimens using a sharp scalpel (Broche Medical, Istanbul, Turkey). Then the specimens were thermocycled for 10,000 cycles at 5°C and 55ºC. Following ISO 11405:2015 instructions (15), the dwell time in each bath was set 20 seconds, and the transfer time between the 2 baths was set 10 seconds.
Shear bond strength (SBS) test
A ''knife-edge'' blade with dimension of 2 mm was used in a universal testing machine (Shimadzu, Model AGS-X 5 kN; Shimadzu Corporation, Kyoto, Japan) to create a vertical loading force with a cross-head speed of 1.0 mm/min until debonding occured. Schematic design of the study protocol is presented in Figure 1. The SBS was calculated in megapascals (MPa) using the equation SBS (MPa) =F(Newton)/(π R2), where F was the applied load at failure and R was the radius of the resin composite cylinder.
Interface examination
The fractured surfaces were evaluated by a single operator after debonding, using a stereomicroscope (SMZ 1000, Nikon, Japan) at 40x magnification to identify the failure modes into one of the following categories:
Adhesive failure at the interface between composite resin and BD;
Cohesive failure within the BD or composite resin;
Mixed failure composed of adhesive and cohesive failure of the BD or the composite resin.
Representative specimens (n=6) chosen randomly from each group and imaged using a scanning electron microscope (SEM) (Hitachi SU3500, Japan) at magnification of 42x. Prior to SEM observations, the specimens were sputtercoated with gold at 45 mA current for 2 min (Sputter Coater S 150A; Edwards, Crawley, England).
Statistical analysis
SPSS 24.0 for Windows (SPSS Inc., Chicago, IL, USA) were carried out for data analysis. Shapiro-Wilk test was used to determine the normality. As the data were normally distributed, the data were consequently analysed using parametric tests. Descriptive statistics were used to summarize the study characteristics and SBSs for resin composite materials. Percentages were used to present the failure modes for different materials. One-way ANOVA test was used to compare the groups. Paired T-test was used within the groups to determine the effect of etching mode on SBSs. Pearson correlation coefficients were calculated to determine the relationships between measurements separately in groups. Statistical significance was determined at a confidence level of 0.05 in all the analyses (p<0.05).
Results
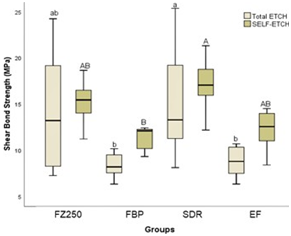
The SBS values of different resin composites to BD by applying a no-wait universal bond in different modes are shown in Figure 2. When taking into account the composite resins, a significant increase in the SBS of SDR was found compared to other composite resin groups (p<0.05). The lowest SBS value was obtained in Group FBP in ER mode (8.89±2.46 Mpa). The highest SBS value was obtained in Group SDR in SE mode (17.13±2.98 Mpa). When taking into account the etching mode, no significant difference was found between the SE and ER etching modes (p>0.05).
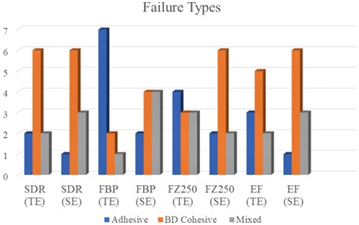
Failure types of the experimental groups are summarized in Figure 3. The majority of failures (48%) occurred cohesively within the BD followed by adhesive failures (28 %). Representative SEM and stereomicroscopy images of fractured BD samples exhibiting adhesive, cohesive, and mixed failures are shown in Figure 4.
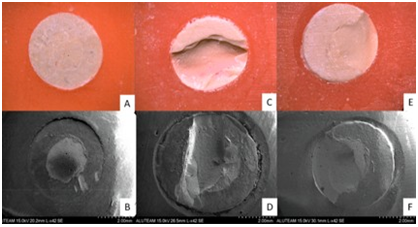
Figure 4 Stereomicroscopic images at x40 magnification and SEM micrographs (x42) of the representative failure types in different experimental groups. (A) Stereomicroscopic image of the adhesive failure. (B) SEM image of the adhesive failure. (C) Stereomicroscopic image of the BD cohesive failure. (D) SEM image of the BD cohesive failure. (E) Stereomi- croscopic image of the mixed failure. (F) SEM image of the mixed failure.
Discussion
When performing VPT procedures, after pulp capping material placement, a powerful bonding between the composite restoration and the biomaterial is crucial to a successful treatment (16). A wide range of study protocols with different adhesive systems and composite types do not allow a comparison between studies. Therefore, the design of a restorative protocol is important to maintain success of VPT. Literature remains uncertain concerning which should be the convenient adhesive strategy and restorative material (11,13,16,17).
In recent years, UA have been introduced with a 'quick bonding' concept by some manufacturers. These are recommended to be used in a short time following a 'no-wait' concept: apply and light cure without waiting. According to the manufacturer's instructions, UA can be light cured at the time of application as it no longer interacts with the dental tissue or additional time is required for the solvent to evaporate before light curing (18). One of the revolutionary "no wait" UAs is CUQ, whose manufacturer claims to have recorded a higher SBS to the dentin than other UAs that have been in use for a longer time. They attributed the excellent data obtained when CUQ was applied without waiting for the quick bonding protocol, to its lower HEMA content, higher purity of the functional monomer 10-methacryldecyl dihydrogen phosphate (10-MDP) and the new acrylamide monomer technology. which has been claimed to improve the infiltration properties of the adhesive (19). In our study, we chose to use this adhesive because of its superior properties.
In the literature there are no studies evaluating the SBS of resin composites when bonded to BD using a ''no-wait'' UA system. Odabaş et al. (10) evaluated the SBS of ER and SE adhesive systems to BD and reported that the highest bond strength value was achieved with SE adhesive systems.
The SBSs of three different dentin replacement materials (BD, Theracal LC, and Fuji IX) were reported to be lower when a one-step SE adhesive was used (11). Hashem et al. (20) found no statistically significant differences between using a UA in ER or SE modes when BD was used. Etching BD has been suggested to lead destruction of the microstructure and improves the leakage through the biomaterial/ composite interface (21). The authors also stated that the chemical composition of BD changed after the application of phosphoric acid, due to the formation of a Ca-phosphate precipitate (22). As mentioned, the application of phosphoric acid on BD showed mechanical and chemical changes on the biomaterial surface (11,20). Essentially, there are few studies evaluating the etching effect on the surface of BD, and no evidence is existing for CUQ. The most common monomer used in adhesive systems is 2-hydroxy-ethyl-methacrylate (HEMA) (23,24). Furthermore, it has been suggested that the functional monomer 10-MDP, present in CUQ, may bind to the calcium in calcium silicate cements, promoting chemical bond in addition to micromechanical attachment (20). The functional monomer can make the adhesion interface more resistant to degradation by forming hydrolytically stable 10-MDP salts, which ionically interact with calcium (25).
In the present study, it was shown that the effect of the etching mode on the SBS of resin composites to BD was not significant (p>0.05). The effect of the addition of another material variable is eliminated by the use of the same UA in both SE and ER modes. The similar SBS values between SE and ER etching modes may be due to the porous structure of the BD surface which may have eliminated the effect of the differences between etching modes. Besides, the acidity from the etching modes may have been buffered by the alkalinity of the BD, reducing its effect as well. In a study investigating the effect of etching on BD compared with GIC and RMGIC, structural and chemical changes were found in the etched compared to non-etched BD (21). Other researchers reported that the placement of composite resin over BD using SE adhesive system resulted in better SBS (10). Conversely, the SBS of BD specimens was lower when SE adhesive was used, which debonded during thermocycling in accordance to a previous study (7). A low pH can interfere with the setting reaction, affect adhesion, or increase the solubility of calcium silicate-based materials (26,27,28,29,30). The development of hydroxyapatite crystals and thus a hybrid layer at the calcium silicate-based materials and dentin interface are likely to be limited in an acidic environment (27). The differences in results may be due to the differences in research methodology such as thermal cycling and different brands of adhesive systems used.
The highest SBS was observed in the Group SDR in SE mode. This may be due not only to the monomer chemistry of SDR bulk-fill flowable composite, but also to its surface energy and wettability characteristics which are better than those of the other composites used (31). Van Ende et al. (32) stated that bulk-fill flowable composites showed better internal adaption than methacrylate-based flowable composites with increased wettability in cavities with high C-factor. Adaptation of the composite resin is associated with higher surface energy and the high surface energy enhances the SBS. Likewise, Moorthy et al. (33) reported that bulk-fill composites have better cavity adaptation than methacrylate-based composites.
Therefore, the first null hypothesis that the composite resin type did not have significant effect on the SBS was rejected but the second null hypothesis that different etching mode did not affect SBS was accepted.
The bond strengths presented in this study were low when compared with the SBS of CUQ to dentin, which was reported by Saito et al. (34) to be as high as 34.5 MPa. This may lead to the belief that the bond between the tricalcium-based cement and the overlying composite restoration may be less important than the bond between the final restorative material and the surrounding dentin/enamel surfaces.
The overall distribution of the failure location was largely cohesive within the BD; this could be an indicative of durable interaction because the material itself collapsed prior to adhesion between the BD and the composite resin. The dominant cohesive mode of failure in BD specimens may reflect a low cohesive strength of the material itself (20). Furthermore, no specimens presented cohesive fractures within the composite resin, likewise Palma et al.'s (35) and Odabas et al.'s (10) results. It has been suggested that bonding is acceptable when the fractures are cohesive within the biomaterial, contrary to the occurrence of adhesive fractures (36). A cohesive failure within the pulp capping material represents the strength of the biomaterial itself and does not necessarily reflect the interfacial bond strength of composite/ biomaterial (20).
Our results showed a larger variability in the TE samples when compared with the SE. Although the initial setting time of BD is known as 12 min, it takes up to 2 wk to achieve complete maturation of BD and reach its maximum physico-mechanical properties (37). The early application of acid with low pH may have caused a non-uniform stress distribution that concentrated in the material substrate of some specimens and caused prema- ture failure of the interface itself (38). No statistically significant difference was found between the SBS values of TE and SE modes, however the results of TE specimens were found to be lower than those of SE samples. Clinically, this finding should be viewed with caution, as it influences the decision in which mode to apply the UA to the overlying resin composite restoration, as the cured shrinkage of the resin composite can stress the weak BD in this early sensitive setting phase, leading to premature failure.
Based on the results of this study, future studies should look into the SBS of BD leaving to set for a longer time period before the application of the resin composite materials.
Conclusion
Within the limitations of the present in vitro study, our findings suggest that SDR has shown superior SBS results when compared with all tested resin composites, which present a suitable alternative for performing restorative procedure immediately after BD placement. Besides, applying a ''no-wait'' universal adhesive on BD in SE or ER mode did not change the SBS of the tested resin composites.